Psychotic depression: causes, symptoms, and treatments

Psychotic depression, also known as depressive psychosis, is a form of major depressive disorder indicated by psychotic symptoms such as hallucinations and delusions. Psychotic depression is not a separate illness, but it can be debilitating and have a major impact on a person’s quality of life.
The causes of psychotic depression include genetics, gender, age, health problems, stress, trauma, and isolation. Further research is necessary to elucidate all the underlying mechanisms behind the relationship between psychosis and depression.
Symptoms of psychotic depression include agitation, anxiety, constipation, hypochondria, insomnia, intellectual impairment, physical immobility, and delusions or hallucinations.
Treatments for psychotic depression are medications such as antidepressants and antipsychotics, and electroconvulsive therapy.
What is psychotic depression?
Psychotic depression is a serious mood disorder where a major depressive episode occurs together with psychotic symptoms. Psychotic depression can be debilitating, scary, and traumatic for an affected individual. Other names for psychotic depression are depressive psychosis and major depressive disorder (MDD) with psychotic features.
Depression with psychotic features is separated into two categories, Healthline explains. The first category is MDD with mood-congruent psychotic features where hallucinations and delusions reflect feelings and emotions that occur with depression. The second category is MDD with mood-incongruent psychotic features where hallucinations and delusions conflict with depression-related emotions. One person can have both mood-congruent and mood-incongruent types of psychotic depression.
Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) by the American Psychiatric Association categorizes psychotic depression as a subtype of major depressive disorder rather than a separate condition. That being said, the psychosis specifier is independent of severity meaning depression doesn’t have to be severe to justify psychotic depression diagnosis, according to a paper that S.L. Dubovsky et al. published in the April 2021 issue of Psychotherapy and Psychosomatics. The same paper reveals that psychotic depression is a common condition that tends to be underrecognized and inadequately treated.
Over the years, the definition of psychotic depression changed and evolved. Psychosis itself was first defined in DSM-2, which was released in 1968, as a mental impairment that is so severe a patient couldn’t adapt to ordinary demands of daily life. Psychotic depression was defined only by severe impairment with or without the presence of delusions or hallucinations, which are the main characteristics of psychosis. As a result, psychotic depression is not considered a distinct disorder, but rather one end of the spectrum of severity. According to the abovementioned paper, the reports of major depression involving delusions that had a different response to treatment than depression without delusions led to a change in the definition of psychotic depression. The change came with DSM-3, which was published in 1980, and it required delusions, hallucinations, or depressive stupor. In DSM-4, released in 1994, psychotic depression was categorized as a severe type of major depressive disorder indicated by hallucinations and delusions. That categorization remained in DSM-5, published in 2013, but psychosis is independent of the severity of depression.
Although the history of psychotic depression is unclear, it’s useful to mention that the term psychosis appeared in psychiatric literature in 1841, when it was introduced by a German physician and author Karl Friedrich Canstatt. At that point, psychosis was an abbreviation for psychic neurosis and described psychological manifestations of brain disease. The biggest contribution to the understanding of psychosis came from a German psychiatrist Emil Kraepelin in the late 19th century. Kraepelin described symptoms of schizophrenia and psychotic disorders, and he also hypothesized that specific combinations of symptoms in relation to the course of the psychiatric illness can help identify a particular mental disorder. His classification indicates that patterns of symptoms help diagnose a mental illness rather than the presence of common symptoms. This is quite similar to a psychotic depression diagnosis, which doesn’t require depression to be severe if symptoms of psychosis are present.
How common is psychotic depression?
Psychotic depression is not a rare disorder, with a current prevalence of 0.4%, according to a paper that Dr. Maurice M. Ohayon and Dr. Alan F. Schatzberg at Stanford University published in the American Journal of Psychiatry. For comparison sake, the prevalence of depression without psychotic features was 2%. The paper included 18,980 subjects and found that 10% of people who reported feelings of guilt and worthlessness also experienced delusions. These feelings also co-occurred with hallucinations in 9.7% of people. Ohayon and Schatzberg concluded that depression with psychotic features is relatively frequent in the general population as it affects four in 1000 people and it’s more prevalent in women than men.
In a study from Jan 2009 issue of Depression and Anxiety, B.A. Guadiano et al. found that of 2500 patients diagnosed with major depression, 5.3% had psychotic symptoms. When it comes to subjects with psychotic depression, 68% reported hallucinations in the past month and 80% reported a lifetime history of hallucinations. Past-month prevalence of delusions was 20% whereas the lifetime prevalence of delusions was 32%. The presence of both hallucinations and delusions was reported by 17% of participants. In a Chinese study of 1718 subjects, published in the February 2020 issue of the Journal of Affective Disorders by Y. Zhou et al, the prevalence of psychotic depression in patients with MDD was 10%.
According to a post by Dr. Anthony J. Rothschild on UpToDate, lifetime prevalence of psychotic depression varies depending on the setting, but surveys in European countries estimate it’s between 0.4% and 0.5%.
What are the causes of psychotic depression?
The causes of psychotic depression are listed below:
- Genetics
- Gender
- Age
- Health problems
- Stress
- Trauma
- Isolation
1. Genetics
Genetics is heredity or the passing of genetic information and traits from parents to their children. The term genetic predisposition is used for an increased risk of developing a specific physical or psychological condition based on the presence of one or more genetic variants or mutations. Certain genes and gene variations are linked to mental disorders, according to the National Institute of Mental Health. Genetics is one of the causes of psychotic depression, as well.
Genetics becomes a cause of psychotic depression because parents can pass on specific genes to their children and increase their risk of this mental illness. Genes associated with a predisposition to developing psychotic depression include BDNF, DTNBP1, DBH, DRD2, DRD4, MAO-A, and GSK-3beta, according to a review by Dr. Katharina Domschke at the University of Wuerzburg, which was published in the July 2013 issue of Schizophrenia Bulletin. The review also showed that there is a familial aggregation and a considerable heritability (39%) of psychotic depression. Heredity of this condition is shared with schizophrenia, schizoaffective disorder, and affective disorders. Genetic factors contribute to psychotic depression disease risk in partial overlap with disorders along the affective-psychotic spectrum.
Psychotic depression is influenced by polymorphism of the serotonin transporter gene, according to a study by T.J. Stamm et al. in the November 2013 issue of the Journal of Affective Disorders. The study observed a high prevalence of the s-allele of 5-HTTLPR (serotonin-transporter-linked promoter region) in patients with psychotic depression. The term polymorphism in genetics refers to a common variant in a specific sequence of DNA, whereas 5-HTTLPR is a degenerate repeat polymorphic region in the SLC6A4 gene that codes for the serotonin transporter. Variation in 5-HTTLPR is associated with individual differences in emotional resilience and predisposes a person to depressive symptoms, according to a paper by M.B. Stein et al. in the October 2009 issue of the American Journal of Medical Genetics Part B, Neuropsychiatric Genetics.
Genetics is a cause of psychotic depression because people inherit genes that predispose them to the development of this disorder or genes that affect their emotional resilience. More precisely, genetic variations can influence the way people process emotions and make them more vulnerable to affective disorders such as psychotic depression. It’s useful to mention that genetics is not the only cause of psychotic depression. A combination of different factors paves the way to this condition, and genetics is one of them.
2. Gender
Gender refers to the biological characteristics of men and women. These characteristics play a role in their health and well-being. Gender plays a role in a person’s physical and psychological health. According to the Mental Health Foundation from the United Kingdom, women between the ages of 16 and 24 are almost three times as likely to experience common mental health issues such as Post-traumatic stress disorder (PTSD) and anxiety as men of the same age. Gender is also one of the causes of psychotic depression.
Gender becomes a cause of psychotic depression due to a wide range of reasons, including different ways men and women deal with their emotions. When it comes to depression, women more often present with internalizing symptoms, whereas men usually present with externalizing symptoms, according to a paper by Dr. Paul R. Albert at the University of Ottawa published in the July 2015 issue of the Journal of Psychiatry and Neuroscience. The paper suggests that women are more sensitive to interpersonal relationships while men are more vulnerable to external career and goal-oriented factors. Additionally, women also experience specific forms of depression-related illnesses, including anxiety, premenstrual dysphoric disorder, postpartum depression, and postmenopausal depression. Changes in ovarian hormones could also contribute to increased rates of depression in women, according to Dr. Albert.
Mayo Clinic reports that women are more prone to depression and multiple factors are involved, such as hormonal changes, premenstrual problems, pregnancy, life circumstances, and culture including unequal power and status, sexual or physical abuse, and work overload. Women are also more prone to other conditions that may contribute to depression such as anxiety, eating disorders, and substance abuse.
When it comes to psychosis, men and women are equally susceptible to it, but there are differences in how psychotic symptoms affect them, according to Women and Psychosis, an Information Guide by the Centre for Addiction and Mental Health (CAMH). The guide explains that women’s delusions tend to focus on relationships, whereas men have more abstract concerns. Women are also more likely to experience mood-related symptoms, especially depression.
A paper from the January 2015 issue of The Scientific World Journal, published by A. Barajas et al, also confirmed that men and women have differences in the expression of psychosis that extend across a continuum ranging from subclinical forms of illness to the onset of psychosis. The differences are usually present in aspects of clinical expression and social functioning.
Gender is a cause of psychotic depression because genetic and biological differences between men and women can affect the way they process emotions or perceive reality. While women and men have the same risk of psychosis, they experience it differently. More research is necessary to elucidate how gender plays a role in the development of psychotic depression.
3. Age
Age is defined as a period of time a person has been alive. A person’s age plays a role in the development of chronic diseases and mental health problems. For example, natural body changes linked to aging may raise the risk of depression, according to the American Psychological Association. Age is also one of the causes of psychotic depression.
Age becomes a cause of psychotic depression because there is an average onset of this mental illness. Although people of all ages can develop psychotic depression, the average age of onset of unipolar major depression among people with psychotic depression is 29 years, according to a post on UpToDate. In a study by J.J. McGrath et al. in the July 2016 issue of Schizophrenia Bulletin, the average age of onset of psychosis is 26 (17 to 41 years).
Age is a cause of psychotic depression because mental illnesses begin when dramatic biological changes in the brain occur from childhood through adolescence to adulthood, as per findings of the large-scale meta-analysis that M. Solmi et al. published in the June 2021 issue of Molecular Psychiatry. These changes involve grey matter density, cerebral metabolic rate, white matter growth, myelination, and synaptic density. For example, adult mental illnesses originate early during the neurodevelopmental phases of life and peak by mid to late adolescence. More precisely, age plays a role in the development of psychotic depression because it has a lot to do with brain structure and function. Brain structure and function affect how people process emotions and perceive the world around them.
4. Health problems
A health problem is a state in which a person is unable to function normally or without pain. It can be acute (short-term) or chronic (long-term or persistent). Physical and mental conditions have a strong connection. For that reason, health problems can cause psychotic depression.
Health problems become a cause of psychotic depression because they provide the life event or chronic difficulty that may trigger a depressive episode in vulnerable individuals, explained Dr. Guy M. Goodwin from Oxford University in his paper from the June 2006 issue of Dialogues in Clinical Neuroscience. Another mechanism that connects health problems and depressive symptoms, according to the same paper, is that there are specific associations between depression and physical illnesses, suggesting an etiological aspect. This particularly relates to brain mechanisms underlying reward and stress/autonomic regulation.
Health problems are a cause of psychotic depression because chronic pain or illnesses such as cancer involve a great deal of worry about one’s treatment and future. Dealing with serious health problems can be overwhelming, and a patient may feel hopeless. The difficulty of their situation can be a traumatic experience and may pave the way to psychotic depression symptoms.
5. Stress
Stress is a state of worry or mental tension resulting from a difficult situation. It is a natural human response to threats and challenges in life. Every person experiences stress at one point in their lifetime. However, stress becomes a problem when it’s persistent and unmanaged. When left unresolved, stress can affect physical and mental health alike. The result of long-term activation of the stress response system is overexposure to stress hormones such as cortisol, which can disrupt the body’s processes. In turn, the risk of mental problems such as anxiety and depression goes up, according to the American Psychological Association. Stress is a significant cause of psychotic depression.
Stress becomes a cause of psychotic depression because it disrupts a person’s coping mechanisms, according to a post by Dr. Alice Boyes on the Psychology Today website, published in March 2013. Dr. Boyes explains that people under stress stop engaging in healthy coping strategies that keep their mood balanced. At the same time, low mood caused by stress generates even further stress, thereby contributing to depressive symptoms. The same post also describes other factors through which stress contributes to depressive symptoms such as its negative impact on relationships, unhealthy coping mechanisms, and disruption of everyday routines.
When it comes to symptoms of psychosis, stress may lead to such a state by activating dopaminergic transmission. That happens because cortisol increases serum levels of a dopamine metabolite called homovanillic acid. Stress may cause psychosis because its effects could be mediated by excitatory inputs of the amygdala to the hippocampus, according to a paper by C. Corcoran et al. in the January 2002 issue of CNS Spectrums.
Stress is a cause of psychotic depression because it negatively affects brain structure and function, thereby paving the way to symptoms of this condition. L. Yang et al. explain in their article from the July 2015 issue of Current Neuropharmacology that chronic stress acts on brain areas involved in depression, such as the amygdala, prefrontal cortex, hippocampus, thalamus, and striatum. These regions are involved in mood, processing emotion, and perception of reality. It’s also useful to mention that chronic stress affects brain chemicals and is involved in the dysregulation of the neurotransmitter serotonin, according to a paper by R. Natarajan et al. in the June 2017 issue of The Journal of Neuroscience. Low serotonin levels can lead to depression, as confirmed by D. Erritzoe et al. in their article from the October 2022 issue of Biological Psychiatry.
6. Trauma
Trauma is an emotional response to a terrible event or extremely upsetting experience such as sexual abuse or assault, natural disaster, physical abuse, or war. It affects people who either witness or experience a frightening event. Trauma makes a person more vulnerable to developing mental health problems and may directly cause PTSD, according to the Mental Health Foundation. Trauma is one of the causes of psychotic depression.
Trauma becomes a cause of psychotic depression because it shapes beliefs, intrusions, appraisals, and coping responses. According to a May 2017 paper in Frontiers in Psychology written by Dr. Amy Hardy at King’s College London, trauma may contribute to the rise of sensory-perceptual intrusions that lead to a search for meaning. These attributions of meaning may result in psychotic experiences. Then, a person maintains these experiences as a way to cope with a traumatic event. Lack of opportunity to talk about trauma aggravates a person’s difficulties and contributes to psychotic experiences, according to a qualitative study by C. Campodonico et al. in the March 2022 issue of BMC Psychiatry.
Trauma is a cause of psychotic depression because it can lead to PTSD, which reduces a traumatized person’s opportunities to obtain positive reinforcement, explained psychology writer Arash Emamzadeh in his post from April 2019 on Psychology Today. More precisely, trauma victims have limited opportunities to feel pleasure or obtain rewarding experiences, which paves the way to depressive symptoms. Additionally, people who have witnessed or experienced trauma may engage in actions that further contribute to their symptoms. A good example of these actions is substance abuse. It’s also useful to mention that childhood trauma is associated with abnormal brain connectivity in major depressive disorder, according to a study that M. Yu et al. published in the April 2019 issue of Proceedings of the National Academy of Sciences of the USA (PNAS). More precisely, trauma can cause abnormalities in the dorsal attention network, frontoparietal network, cingulo-opercular network, ventral attention network, subcortical regions, auditory network, visual network, and sensorimotor network.
7. Isolation
Isolation is defined as the lack of social contact or having few people to interact with regularly. It is the absence of social interactions and relationships with other people, including friends, family, coworkers, and neighbors. Although social isolation is a symptom of mental illnesses such as depression, it can also cause them. Social isolation affects every aspect of mental health, WebMD explains. That’s why it’s one of the causes of psychotic depression.
Isolation becomes a cause of psychotic depression because it increases stress levels, disrupts sleep, and may even contribute to anxiety, according to a post by Amy Novotney in the May 2019 issue of the print version of the American Psychological Association. The neuroendocrine, behavioral, and neural responses to social isolation can lead to negative mental and physical outcomes, according to a paper by L. Brandt et al. from the September 2022 issue of Translational Psychiatry. Social isolation can heighten alertness to potential harm from people and it is accompanied by symptoms of anxiety and depression.
Isolation is a cause of psychotic depression because it leads to loneliness, which triggers both positive and negative psychotic symptoms in clinical and non-clinical populations alike, reported A. Andreu-Bernabeu et al. in the January 2022 issue of Nature Communications. One of the pathways to developing psychotic symptoms is poor self-esteem or self-concept. According to a paper by B. Michalska da Rocha et al. published in the January 2018 issue of Schizophrenia Bulletin, people with psychosis tend to have low self-esteem whereas people with hallucinations and delusions have a negative self-concept. The feeling of loneliness could strengthen negative self-esteem or self-concept and thereby contribute to the onset of psychosis. For that reason, isolation causes psychotic depression with a negative effect on mental processes that contribute to both psychosis and depression.
Who is at risk for psychotic depression?
People who have no close friends or loved ones to confide in and those with infrequent contact with family and friends are at risk for psychotic depression. Risk factors for psychotic depression also include a family history of mental illness and experiencing a major negative life event in the past year, according to a paper by M. Heslin et al. published in the February 2016 issue of Social Psychiatry and Psychiatric Epidemiology.
The paper investigated the psychosocial and biological risk factors associated with psychotic depression and psychotic disorders such as schizophrenia. Scientists found that risk factors associated with psychotic depression overlap with those for schizophrenia, but less so for bipolar disorder. Besides the abovementioned risk factors, the paper also listed living alone, being unemployed, negative events in childhood, and a family history of psychosis.
According to Healthline, risk factors for psychotic depression also include major hormonal changes such as menopause and the postpartum period, extreme stress or trauma, ongoing financial difficulties, chronic pain or chronic health condition, older age, and being transgender.
Research regarding risk factors for psychotic depression is limited, but a paper by M. Nietola et al. published in the February 2020 issue of Social Psychiatry and Psychiatric Epidemiology showed that low school sports grades in adolescence and familial mental illness are common risk factors for psychotic depression.
V. Rodriguez et al. published a systematic review and meta-analysis in the July 2021 issue of Schizophrenia Bulletin and their results showed some overlap between environmental risk factors for psychotic depression and bipolar disorder. These risk factors include parental age >40 years, early or late gestational age, childhood adversity, substance misuse, and being from an ethnic minority. Researchers found evidence confirming the link between affective psychosis and exposure to specific insults (listed above) from early development to adulthood.
A comparative study by M. Thakur et al, published in the May 1999 issue of Psychiatry Research, showed that common characteristics among patients with psychotic depression were younger age, psychomotor retardation, feelings of worthlessness and guilt, history of delusions, suicidal thoughts, and tendencies. Poor subjective social support was also associated with psychotic depression.
What are the symptoms of psychotic depression?
Symptoms of psychotic depression are a combination of symptoms of major depressive disorder (MDD) and psychosis. The severity of symptoms varies from patient to patient. The most significant symptoms of psychotic depression are listed below:
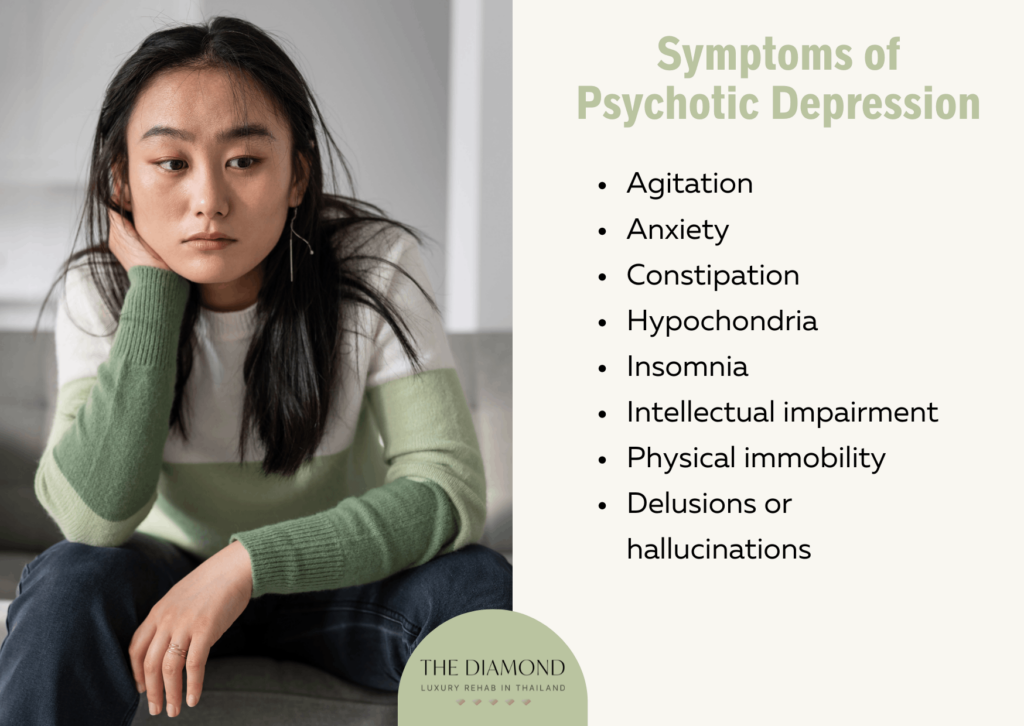
- Agitation
- Anxiety
- Constipation
- Hypochondria
- Insomnia
- Intellectual impairment
- Physical immobility
- Delusions or hallucinations
1. Agitation
Agitation is a state of extreme arousal. It is described as a feeling of irritability and severe restlessness, according to a post by W. Siddiqui et al. on the website of the National Library of Medicine. The same post explains that agitation can be a normal physiological process associated with specific situations, but it can also occur due to underlying conditions, drug intoxication or withdrawal, alcohol in the system, or medical conditions. Psychotic depression can cause agitation as well.
Agitation becomes a symptom of psychotic depression due to low serotonin. People who feel irritated a lot tend to have low serotonin activity, Medical News Today explained. Irregularities involving serotonin are also associated with depression, as explained above in this post. Serotonin helps regulate mood. For that reason, impaired activity of this neurotransmitter can affect an individual’s mood and lead to agitation.
Agitation is one of the symptoms of psychotic depression because it is closely associated with psychosis. In psychosis, agitation is associated with positive symptoms (delusions and hallucinations). Development of these symptoms involves several neurotransmitter systems such as dopaminergic, serotonergic, GABAergic, and glutamatergic. Development of this symptom and the state of psychosis could be due to mesocortical disconnection syndrome caused by limbic dopaminergic hyperactivity and interruption of glutamatergic modulation of dopaminergic transmission with decreased GABAergic inhibition, according to a paper called The Pathophysiology of Agitation written by Dr. Jean-Pierre Lindenmayer. The paper was published in The Journal of Clinical Psychiatry. More precisely, the dysfunction of several neurotransmitters and their transmission could contribute to psychosis and agitation. That explains why a person with psychotic depression may be agitated as well.
As a symptom of psychotic depression, agitation is identified as a feeling of unease, an urge to move, being impatient or cranky, stubbornness, excessive excitement, and nervousness.
2. Anxiety
Anxiety is defined as a feeling of unease such as fear, which can range from mild to severe. Occasional anxiety is a normal part of life. For example, a person may experience anxiety before an exam, a job interview, or when going through major life changes. However, anxiety can become a problem when it is intense, excessive, and persistent. Factors such as childhood trauma, major life stress, or physical and mental conditions, can cause anxiety. It can occur as a symptom of psychotic depression as well.
Anxiety becomes a symptom of psychotic depression because people with depression tend to become worried and anxious. Nearly one-half of people diagnosed with depression also develop an anxiety disorder, according to the Anxiety and Depression Association of America. Even though depression is a low-energy state and anxiety is a high-energy state, they can occur together. According to a post by Thomas Tjornehoj on the website of Hartgrove Behavioral Health System, depressed persons tend to experience anxiety that may become so serious it leads to panic attacks. When it comes to the relationship between depressive disorder and anxiety, it’s useful to mention that the presence of anxiety symptoms worsens the outcomes of a mental illness such as this one. People with anxious depression are more likely to have severe symptoms, including suicidal ideation, according to a post by Dr. Ned H. Kalin published on the website of the American Journal of Psychiatry in May 2020.
Anxiety is one of the symptoms of psychotic depression because psychosis can be an overwhelming experience that may lead to nervousness and anxiety. A person with this condition may feel anxious about their symptoms, especially hallucinations and delusions, which can contribute to anxiousness. Psychotic symptoms can lead to panic attacks, according to a post by R.D. Goodwin et al. in the January 2004 issue of the American Journal of Psychiatry. The same paper explained that psychotic episodes can precede and predict the onset of specific anxiety disorders such as PTSD. Although there are no studies regarding anxiety and psychotic depression, it’s useful to mention that prevalence of anxiety in people with schizophrenia (characterized by psychotic symptoms such as hallucinations and delusions) is higher than in the general population, according to a post by C. Kiran and S. Chaudhury in the January-June 2016 issue of the Industrial Psychiatry Journal.
As a symptom of psychotic depression, anxiety is identified as restlessness, nervousness, irritability, difficulty concentrating, worry, sleep problems, and headaches or unexplained pains.
3. Constipation
Constipation is defined as having fewer than three bowel movements a week. Occasional constipation is common, but this gastrointestinal problem can become chronic and affect a person’s quality of life. Common causes of constipation are insufficient fiber intake, changes in eating habits, not drinking enough fluids, and a sedentary lifestyle. Constipation is common in the psychiatric population with a two-year period prevalence of 36.3% in schizophrenic patients and 57.7% in depressive patients, reported J.G. Jessurun et al. in a cross-sectional study published in the March 2016 issue of Psychiatry Journal. Constipation may occur as a symptom of psychotic depression as well.
Constipation becomes a symptom of psychotic depression due to the effect of the disease itself or due to other factors such as an unhealthy lifestyle. The abovementioned paper explained that people with serious mental illnesses tend to have an unhealthy lifestyle indicated by insufficient fluid intake, poor diet, and physical inactivity. These factors can lead to constipation.
When it comes to the effect of the disease, it is important to mention low serotonin levels as a factor that may cause constipation problems. Low serotonin is associated with depression, but it also affects gut health. The gut, often referred to as the “second brain”, has more neurons than the spinal cord and it functions with a similar suite of neurotransmitters as the human brain. Low serotonin levels in the gut led to a reduced number of neurons, caused deterioration of the gut lining, and decreased the speed of movement through the gut, showed a study by N. Israelyan et al. in the August 2019 issue of Gastroenterology.
Constipation is one of the symptoms of psychotic depression because the affected persons may have elevated stress hormones. Disorders that involve psychosis are associated with elevated cortisol levels, according to a paper by E.F. Walker et al. in the September 2013 issue of Biological Psychiatry. Stress hormones affect bodily processes and may directly influence bowel movements. In people with psychosis, the gut microbiome is altered, reported A-K Kraeuter et al. in a study from the August 2020 issue of Frontiers in Psychiatry. Constipation may also occur as a side effect of antipsychotic medications such as clozapine and tricyclic antidepressants.
Mental illnesses such as depression may contribute to gut inflammation, according to M. Clapp et al. who published their paper in the September 2015 issue of Clinics and Practice. Inflammation can lead to constipation.
As a symptom of psychotic depression, constipation is identified as having fewer than three bowel movements a week, stools that are hard or dry and lumpy, stools that are painful and difficult to pass, and feeling that not all stool has passed.
4. Hypchondria
Hypochondria or hypochondriasis is a persistent, unrealistic fear and excessive worry about becoming sick or having a serious illness. A person with hypochondria is preoccupied with their health and tends to focus on specific symptoms such as gastric or cardiac problems. People develop hypochondria due to multiple reasons including major life stress such as serious illness in the family, history of abuse and neglect, and personal history of serious physical illness. The presence of mental illness can also contribute to hypochondria. Mental illnesses such as anxiety, depression, compulsive disorder, and psychotic disorders can cause hypochondria, according to HealthDirect Australia. Hypochondria may also occur as a symptom of psychotic depression.
Hypochondria becomes a symptom of psychotic depression due to impaired emotion regulation. J. Bailer et al, reported in their study from the November 2017 issue of Clinical Psychology and Psychotherapy, that both depression and hypochondriasis involve emotion dysregulation. Depression tends to include a more generalized pattern of emotion dysregulation whereas hypochondriasis is associated with somatic symptoms, health anxiety, and illness behavior. More precisely, people with depressive disorder exhibit impaired regulation of emotions, which is also associated with hypochondriac behavior. Emotion dysregulation is a common characteristic of psychotic disorders, H.C. Chapman et al. confirmed in a study from the February 2020 issue of Development and Psychopathology. That means psychosis is also associated with the inability to regulate emotions.
Hypochondria is one of the symptoms of psychotic depression because hypochondria itself is a mild form of psychosis. Dr. Berit Brogaard explained in her post from October 2016 on the Psychology Today website that hypochondriacs display a deep and ungrounded worry about developing a serious illness. This is important because psychosis involves false beliefs and impaired perception of reality, as well. Psychosis includes hallucinations and delusions. People with delusions may be convinced they are sick or that they will develop an illness, even if they’re actually healthy. Hypochondriacal delusions are based on altered body perception in mental illness, indicated by dysesthesias (unpleasant/abnormal sense of touch) to the point of depersonalization and the patient’s increased attention to their body, according to a case report by T. Fuchs from Technischen Universitat Munchen published in the April 1992 issue of Zeitschrift fur Klinische Psychologie und Psychotherapie.
As a symptom of psychotic depression, hypochondria or hypochondriasis is identified as spending a lot of time thinking about having a serious illness, seeing a doctor many times and refusing to accept reassurances, and seeking out medical tests or exams. Hypochondriasis manifests itself as spending hours online studying symptoms to make a diagnosis, talking about health with friends and family all the time, and worrying that minor symptoms indicate the presence of a serious disease.
5. Insomnia
Insomnia is a sleep disorder where a person struggles to fall asleep or stay asleep. A person with insomnia may wake up too early and not be able to go back to sleep again. Insomnia may be a primary problem, but other factors can cause it. These factors are stress, travel or work schedule, poor sleep habits, medications such as pain/allergy/cold medicines, and health conditions such as chronic pain, diabetes, heart disease, cancer, Parkinson’s disease, and Alzheimer’s disease. Caffeine, nicotine, and alcohol intake can also lead to insomnia. Mental health conditions do too. According to the Mayo Clinic, anxiety disorders such as PTSD are associated with insomnia. Waking up too early can also be a sign of depression. Insomnia is also a symptom of psychotic depression.
Insomnia becomes a symptom of psychotic depression because the depressive disorder can cause behavioral, psychological, and physiological changes that disrupt sleep. Depression may cause behavior changes such as increased intake of caffeine or alcohol, waking up later than usual, meaning a person is less tired at bedtime, and increased screen time. These behaviors can affect sleep and cause insomnia, according to Medical News Today. Psychological changes that cause insomnia in people with depression include stress and the increased presence of negative thoughts, especially if a person tends to ruminate at bedtime. As a result, it becomes difficult to fall asleep. Physiological changes that lead to insomnia include the influence of depression on brain chemistry, hormones, and brain activity. The same article explains that depression-related insomnia can be acute (short-term) and chronic (long-term).
About three-quarters of patients with depression have symptoms of insomnia, reported D. Nutt et al. in a paper from September 2008 issue of Dialogues in Neuroscience. The same paper explains that sleep-related problems in depression point to the disruption of homeostatic and circadian drives to sleep. A contributory factor to insomnia in patients with depression is the general hyperarousal or psychic anxiety, present in 80% of depressed individuals. Insomnia and depression have a two-way relationship. For example, people who experience insomnia are also more likely to develop depression.
Insomnia is one of the symptoms of psychotic depression because the increased dopaminergic states implicated in the causation of psychosis can cause insomnia as well, explained Dr. Khurshid A. Khurshid from the University of Florida College of Medicine in Gainsville in the March-April 2018 issue of the journal Innovations in Clinical Neuroscience. In people with psychosis, insomnia is the most prevalent sleep disorder, according to S. Reeve et al. who published their article in the March 2019 issue of Schizophrenia Bulletin. People with symptoms of psychosis, such as delusions, especially, persecutory type, have difficulties initiating and maintaining sleep, reported D. Freeman et al. in a paper from the March 2009 issue of Schizophrenia Research. Psychosis and insomnia have a complicated relationship because insomnia can lead to a psychotic state as well.
As a symptom of psychotic depression, insomnia is identified as difficulty initiating sleep, waking up several times during the night, lying awake at night, waking up too early and being unable to fall asleep again, feeling tired after waking up, difficulty taking a nap during the day despite the tiredness, and feeling irritated during the day.
6. Intellectual impairment
Intellectual impairment refers to problems with general mental abilities that affect functioning in two areas such as intellectual and adaptive functioning. Intellectual functioning involves learning, judgment, and problem-solving whereas adaptive functioning refers to daily life activities such as communication and independent living. Mental illnesses can affect cognitive functioning and thereby contribute to intellectual impairment. For example, intellectual impairment can be a symptom of psychotic depression.
Intellectual impairment becomes a symptom of psychotic depression due to decreased motivation, impaired concentration, attenuated attentional capacity, intrusive thoughts, and slowness, all of which occur in people with depressive disorder. Significant cognitive disturbances could be one of the major symptoms of depression, according to a paper called Cognitive Deficits in Psychiatric Disorders: Current Status in the January-March 2006 issue of the Indian Journal of Psychiatry. In the acute phase of depression, people tend to make more attention-related mistakes, and their verbal memory is also impaired. Problems are also evident in non-verbal memory, spatial working memory, and implicit non-declarative memory of depressed individuals. Intellectual impairment in people with psychotic depression occurs because this condition affects more than mood and emotion. The depressive disorder affects brain functioning thereby impairing cognitive abilities.
Intellectual impairment also involves problems with adaptive functioning. For that reason, it’s important to keep in mind that mental illnesses such as depressive disorder can cause speech deficits such as long pauses during conversation. Due to long pauses, a person with depression gets interrupted a lot, which worsens their communication skills, according to Williamsville Psychiatry.
Intellectual impairment is one of the symptoms of psychotic depression because psychosis and psychotic-like symptoms can affect cognitive functioning too, as per findings of the study that W. ten Velden Hegelstad et al. published in the July 2020 issue of Frontiers in Psychology. Symptoms of psychosis, such as delusions, can affect cognitive functioning. Although there are no studies on psychotic depression and cognitive impairment, evidence focusing on delusional disorder showed the impact of delusions on cognitive abilities. For example, a paper by I. Ibanez-Casas et al. in the July 2013 issue of PLoS One reported that people with delusions exhibited lower levels of flexibility, slower speed processing, poorer memory and reasoning, and restricted capacity for learning.
As a symptom of psychotic depression, intellectual impairment is identified as having decreased attention, poor memory, reduced speed of processing information, learning difficulties, trouble with reasoning and thinking abstractly, and impaired ability to understand social information such as body language and emotional expression. Their communication skills are also impaired.
7. Physical immobility
Physical immobility is a state wherein a person is at a high risk or experiences limitation of physical movement. Causes of physical immobility can be cardiovascular, neurological, and musculoskeletal disorders and associated pain, but psychological factors can play a role. For example, mental health symptoms are strongly linked to mobility limitation, according to S. Rask et al. who published their study in the March 2015 issue of BMC Public Health. Physical immobility can be a symptom of psychotic depression.
Physical immobility becomes a symptom of psychotic depression because the depressive disorder has a negative impact on physical activity. Depressive symptoms manifest themselves physically as well and reduced motivation to move or exercise is one example. Depression depletes energy levels thus making it more difficult for a person to be active or exercise.
B. Roshanaei-Moghaddam et al. confirmed in their paper from the July-August 2009 issue of General Hospital Psychiatry that depression contributes to a sedentary lifestyle and leads to a decline in activity. The paper explains that the relationship between lack of mobility and depressive disorder is bidirectional. Depression leads to physical immobility through lower motivation and energy levels, while a lack of physical activity increases the risk of depressive symptoms.
Factors that make it difficult for a person with a depressive disorder to exercise are low dopamine, anxiety regarding what people will think, changing daily routine can be overwhelming, lack of social support, and negative self-talk, Dr. Samantha Rodman explained in her TalkSpace post from January 2018.
Psychomotor retardation is associated with depressive symptoms, but this connection requires more research. Patients with depression tend to have frontostriatal abnormalities such as white matter changes in basal ganglia and reduced volumes of the prefrontal cortex, putamen, and caudate. These particular deficits are more expressed in presence of psychomotor retardation, according to a paper that J.S. Buyukdura et al. published in the March 2011 issue of Progress in Neuro-Psychopharmacology and Biological Psychiatry. The same study suggests that reduced blood flow in the dorsolateral prefrontal cortex, left prefrontal cortex, anterior cingulate, and angular gyrus are all associated with psychomotor retardation in depression. Abnormalities regarding dopaminergic transmission, serotonin, and the hypothalamus-pituitary-adrenal (HPA) axis are involved in psychomotor retardation in patients with this condition, too.
Physical immobility is one of the symptoms of psychotic depression because symptoms of psychosis (hallucinations and delusions) may lead to avoidance or being unable to do any activity. For example, the majority of people with persecutory delusions are physically inactive, according to a study that R. Diamond et al. published in the October 2022 issue of Mental Health and Physical Activity.
As a symptom of psychotic depression, physical immobility is identified as problems with movement, physical activity, and high levels of sedentary behavior.
8. Delusions or hallucinations
Delusions are false beliefs despite the evidence that those beliefs are not true. The false belief is based on incorrect inference about external reality that a person firmly sustains regardless of evidence to the contrary. Delusions are a symptom of psychosis. People can have persecutory, erotomanic, jealous, grandiose, or somatic delusions.
On the flip side, hallucinations are false perceptions of objects or events involving senses (sound, sight, touch, taste, and smell). Hallucinations are a symptom of psychosis, as well. To an affected person, hallucinations such as hearing voices or seeing objects or people seem real, but they are not.
The difference between a hallucination and delusion is that the latter is a false belief in something that isn’t true (e.g. beliefs of being followed or spied on) whereas hallucination is false sensory perception. Delusion is based on a firm belief in things that aren’t correct whereas hallucination affects the senses only.
Both symptoms occur due to psychotic disorders such as schizophrenia, but other factors can also cause them. For instance, delusions and hallucinations can be symptoms of psychotic depression.
Delusions or hallucinations become a symptom of psychotic depression because depression can become so severe it triggers symptoms of psychosis. Other factors such as high levels of tension, excitement, and suicidal ideation can contribute to psychosis in depression, according to a paper by S-C Park et al. in the July 2014 issue of Psychiatry Investigation. The paper showed that it’s possible for people with mild to moderate depression to experience symptoms of psychosis. Types of delusions and hallucinations are associated with feelings of a person with depression, Mount Sinai explains. For instance, a person with psychotic depression may hear voices that suggest they don’t deserve to live. Voices may criticize the affected individual, as well. It’s also possible that a person with psychotic depression adopts false beliefs (delusions) regarding their body. One such belief is that they have cancer.
The key symptom of psychotic depression, according to a review from the May 2017 issue of Der Nervenarzt, is a depressive delusion. The author of the review, M. Burgy from Klinikum Stuttgart in Germany, suggests that delusional topics are limited to guilt, hypochondria, and impoverishment, which are three primordial fears of human beings. A randomized controlled trial by S. Hartley et al, published in the January 2012 issue of Behavior Research and Therapy, confirmed that depression and anxiety are associated with distinct aspects of psychotic experience and play a role in the onset of early psychosis. Mania plays a significant role in the development of psychotic symptoms in depression, reported L. Zaninotto et al. in their paper from the April 2015 issue of Clinical Psychopharmacology and Neuroscience.
Delusions or hallucinations are one of the symptoms of psychotic depression due to higher cortisol levels. The concentration of stress hormones is elevated in people with depression, but it is also associated with psychosis. Stress is particularly powerful when connected with past trauma. Early exposure to trauma is a risk factor for depression in adulthood, V.V. McCutcheon et al. explained in their paper from the March 2009 issue of Psychological Medicine. Trauma can also lead to psychotic symptoms such as hallucinations, according to A.C. Wright et al. who published their study in the January 2020 issue of Schizophrenia Bulletin. For that reason, the development of psychotic symptoms such as delusions or hallucinations in depression occurs due to several factors, including past trauma and high-stress levels.
As a symptom of psychotic depression, delusions or hallucinations are identified as holding firm beliefs that aren’t based on evidence or reality (e.g. having a disease, being followed, feeling superior to others), arguing with friends or family members who attempt to explain a specific belief is not true, seeing colors or shapes and people that aren’t there, hearing voices or sounds, feeling touched when nobody’s there, sensing odor that other people can’t smell, and feeling a taste when there’s nothing in the mouth.
What can I expect from psychotic depression?
From psychotic depression, a person can expect to experience symptoms of both depression and psychosis. Feeling sad and hopeless almost every day is the biggest sign of depression. A person with this condition may lose interest in activities they used to enjoy. Social withdrawal or isolation is a common consequence of both depressive and psychotic symptoms. People with depressive disorder may notice their appetite changes and they are unable to concentrate on work or task at hand. With the changes in appetite comes along weight gain or weight loss.
When it comes to the psychotic aspect of this condition, hallucinations and delusions reflect the depressed mood. A person may become convinced they have committed a crime or it’s their fault an unfortunate event happened. The UK’s NHS reports psychomotor agitation is common in people with psychotic depression. The term psychomotor agitation refers to the inability to be still or relaxed e.g. a person may constantly fidget. Psychomotor retardation, where both physical movements and thought patterns slow down, is also expected in psychotic depression, as explained in the symptoms above.
People with psychotic depression are at a higher risk of suicidal thoughts and tendencies. In a study that K.J. Fredriksen et al. published in the Spring 2017 issue of Psychiatry, participants experienced being directed to perform impulsive (potentially fatal) actions, feeling hounded to death, being left bereft of mental control, and becoming trapped in a darkness from which they can’t escape. To people with psychotic depression, suicide was considered an escape from life problems, intense anxiety, and psychotic experiences. Unfortunately, their inability to identify and communicate symptoms of psychosis and suicidal thoughts or tendencies was compromised. As a result, patients with psychotic depression in this study struggled alone with uncomfortable experiences.
T. Paljarvi et al. reported in their research paper from the January 2023 issue of the Journal of Affective Disorders that psychotic symptoms doubled the risk of suicides compared to severe depression. Moreover, psychotic depression was associated with more violent methods of suicide, such as suffocation. Suicides mainly occur within two years from the first diagnosis. This only intensifies the need to encourage a patient with psychotic depression to get help and adhere to the treatment protocol.
Depressive and psychotic symptoms can have a deep impact on a person’s quality of life including problems in relationships, with school, or with employment.
How is psychotic depression diagnosed?
Psychotic depression is diagnosed after psychological evaluation and physical exam. People who experience depression with psychotic symptoms usually don’t seek help on their own. Family and friends play an important role because they encourage an affected person to see a doctor.
Psychiatrists or psychologists may ask a patient questions regarding persistent worries or fixed beliefs, health concerns, the presence of symptoms such as difficulty sleeping, or things they see or hear that no one else does. A healthcare professional asks about the patient’s personal and family history of health problems and mental issues.
A physical exam may be necessary to rule out conditions that could be causing the symptoms. For that person, a doctor may order blood or urine tests. Physical examination also involves checking the heart and reflexes.
In order to diagnose psychotic depression, a psychiatrist uses DSM-5 to check whether a patient meets the diagnostic criteria for major depressive disorder. If a patient meets the diagnostic criteria for MDD and they are experiencing hallucinations and/or delusions at the same time, the psychiatrist establishes a psychotic depression diagnosis.
Diagnostic criteria for MDD include depressed mood most of the day, noticeable reduction of interest or pleasure in all/almost all activities, significant weight loss or weight gain, insomnia or hypersomnia (excessive sleep), psychomotor agitation or retardation, fatigue nearly every day, feelings of worthlessness or inappropriate guilt, reduced ability to think or concentrate, and recurrent thoughts of death and suicidal ideation. These symptoms must affect a person’s quality of life and must not be a result of other conditions such as diabetes, thyroid disease, adrenal disorders, Alzheimer’s disease, Parkinson’s disease, epilepsy, and substance abuse. In order to meet the diagnostic criteria for MDD, the symptoms need to last two weeks or longer.
For an accurate diagnosis of psychotic depression, healthcare professionals and family or friends of people with MDD shouldn’t assume hallucinations or delusions aren’t present just because the affected person hasn’t mentioned them. This is important because psychotic depression is often misdiagnosed. Data from the National Institute of Mental Health (NIMH) study carried out by A.J. Rothschild et al. and published in the August 2008 issue of The Journal of Clinical Psychiatry show that 27% of a sample of patients with psychotic depression diagnosis were initially incorrectly diagnosed. Instead, those patients were usually diagnosed with MDD without psychotic features, depression not otherwise specified, and mood disorder not otherwise specified.
People with depression don’t always report symptoms of psychosis. The reason for failing to do so is that they don’t consider those symptoms abnormal. Additionally, a person experiencing psychotic symptoms fails to disclose their experiences because they don’t want to be perceived as ill. It’s possible that a person doesn’t recall those symptoms in one mental state or may not think abstractly enough to answer broad questions such as “do you hear sounds or voices”.
What are the available treatments for psychotic depression?
The available treatments for psychotic depression are based on the severity of the symptoms. For most severe cases, hospitalization is necessary. Generally speaking, the most significant treatments for psychotic depression are listed below:
- Medication
- Electroconvulsive therapy (ECT)
1. Medication
Medication is defined as a form of medicine used in the treatment or prevention of disease. For the treatment of psychotic depression, patients may need to take a combination of antidepressants and antipsychotics.
Antidepressants are prescription medications formulated specifically to manage depression, but they can be used for the management of other conditions, such as anxiety. There are different types of antidepressants such as selective serotonin reuptake inhibitors (SSRIs), serotonin and noradrenaline reuptake inhibitors (SNRIs), tricyclics and tricyclic-related drugs, and monoamine oxidase inhibitors (MAOIs).
Doctors usually prescribe SSRIs to patients with MDD alongside one of the following antipsychotics: olanzapine (Zyprexa), quetiapine (Seroquel), and risperidone (Risperdal). Antipsychotics, also known as neuroleptics, are medications formulated specifically to treat psychosis.
Medication helps to treat psychotic depression because it acts on processes in the brain that contribute to symptoms of this disorder. The most frequently described antidepressants, SSRIs, work by blocking or inhibiting the reuptake of serotonin, meaning more of this neurotransmitter is available to pass further messages between nearby nerve cells. Low levels of serotonin are associated with symptoms of depression. After carrying a message, serotonin is reabsorbed by nerve cells. This reduces the concentration of this neurotransmitter. The SSRI medications work to block that process and increase the levels of serotonin.
Antipsychotics work by modifying how the brain uses neurotransmitters. The exact mechanism of action through which antipsychotics treat psychotic depression depends on the type of this medication. First-generation antipsychotics, or typical antipsychotics, block the way the brain uses neurotransmitters, primarily dopamine, while also blocking acetylcholine, histamine, and norepinephrine from latching onto receptors. Second-generation antipsychotics, or atypical antipsychotics, block certain dopamine and serotonin receptors while activating specific receptors of these neurotransmitters at the same time. Atypical antipsychotics are more frequently prescribed for the treatment of psychosis than typical antipsychotics. By changing the way a person’s brain utilizes neurotransmitters, antipsychotics can help manage delusions and hallucinations.
Medication is one of the best treatments for psychotic depression because it works well with other treatment approaches, including cognitive-behavioral therapy (CBT). CBT is a type of talk therapy that helps a patient identify negative or irrational thought patterns in order to replace them with more rational alternatives. By changing the thinking pattern, CBT helps improve moods, emotions, and behaviors. During CBT sessions, patients also learn skills that help manage the symptoms they experience. Olof Hjorth et al. at Uppsala University in Sweden, carried out research that showed that treatment with SSRIs is even more effective when combined with CBT. The research, published in the October 2022 issue of Translational Psychiatry, revealed that CBT and SSRIs induce neurochemical changes in the brain that help treat symptoms of depression.
Medication is an effective treatment approach for the treatment of psychotic depression and it is scientifically confirmed. For example, Dr. A. Farahani and C.U. Correll from The Zucker Hillside Hospital in New York reported that a combination of antidepressants and antipsychotics is superior to monotherapy in the treatment of psychotic depression. Their paper was published in the April 2012 issue of The Journal of Clinical Psychiatry emphasizes the need for further research on the effect of these medications on symptoms of psychotic depression. The effectiveness of combined treatment with antidepressants and antipsychotics was also confirmed in a review that is a part of BJPsych Advances Cochrane Corner and Round the Corner Collection and published online by Cambridge University Press in January 2018. The review confirmed that a combination of these medications should be the first-line treatment for psychotic depression.
Besides combination therapy, monotherapy could be also effective in the treatment of psychotic depression. The January 2014 issue of The Journal of Neuropsychiatry and Clinical Neurosciences published a case report by Y. Mizoguchi and A. Monji reported about a patient whose psychotic depression was successfully treated with sertraline (Zoloft). Sertraline is an antidepressant that belongs to the class of SSRIs. About two weeks after the 54-year-old woman with psychotic depression started sertraline therapy, she experienced improvements in depressive symptoms and suspiciousness. Within a month, her delusions disappeared completely.
It takes two to four weeks for antidepressants to work for psychotic depression. When it comes to antipsychotics, a patient begins to notice some improvement within six weeks of initiation of this pharmacotherapy. Several months may be necessary to experience full benefits. The optimal continuation and maintenance therapy for psychotic depression is a challenging task. The main goal is to prevent relapse and avoid other concerns such as chronic illnesses, high mortality, and disability rates. Pharmacotherapy with antidepressants is maintained longer than the use of antipsychotics. For people who relapse while discontinuing the antipsychotic during maintenance treatment of prior episodes of psychotic depression, the doctor may decide to maintain the use of antipsychotics for at least six to 12 months. For patients who discontinue the use of antipsychotics successfully but relapse during maintenance therapy with antidepressants, it is recommended to restart antipsychotic therapy, explained Dr. Anthony J. Rothschild from the University of Massachusetts Medical School in his paper published in the Spring 2016 issue of Focus.
2. Electroconvulsive therapy (ECT)
Electroconvulsive therapy is a treatment that relies on sending an electronic current through a person’s brain to induce a generalized seizure and manage symptoms of specific mental health problems. Uses of electroconvulsive therapy include severe major depression or bipolar disorder that doesn’t respond to other treatments such as talk therapy or medications.
Electroconvulsive therapy helps to treat psychotic depression because it induces chemical and cellular changes in the brain that alleviate the symptoms. A patient receives ECT under anesthesia in a hospital. During the session, the healthcare professional places electrodes against the skin of the patient’s head. The electrical stimulation triggers a brief surge of electrical activity within the brain i.e. seizure. Seizures from electroconvulsive therapy tend to last between 30 and 90 seconds, Cleveland Clinic explains. After ECT, molecular changes occur. These changes increase communication between neurons in the brain area that responds to antidepressants too, I.M. Reti and researchers at Johns Hopkins found in a study they published in the October 2017 issue of Neuropsychopharmacology. More precisely, after ECT new brain cells develop in the hippocampus. Repeated a few times, ECT eliminates symptoms of depression.
Electroconvulsive therapy is one of the best treatments for psychotic depression because it works well in combination with medications and it can also help treat symptoms of psychosis. For example, the doctor may recommend ECT to patients with schizophrenia who didn’t benefit from medications and therapy. This is important because schizophrenia involves symptoms of psychosis such as hallucinations and delusions. Healthline explains that ECT may change the function of certain parts of the brain that cause these symptoms.
The effectiveness of electroconvulsive therapy is confirmed by numerous studies, including a review by M. Li et al. in the February 2020 issue of Frontiers in Psychology. The review showed ECT can alleviate symptoms of depression independent of antidepressants, but when used in combination with these medications, it enhances their anti-depressive effects. A paper called Electroconvulsive Therapy and Its Different Indications from the March 2008 issue of Dialogues in Clinical Neuroscience confirmed that ECT is an effective treatment approach for depression and even schizophrenia, which is indicated by psychosis. Moreover, ECT is also effective in relapse prevention during maintenance therapies. Another review, published by M.J. Park et al. in the January 2021 issue of Psychiatry Investigation, explained that the use of ECT in the management of depressed patients with psychotic depression, bipolar depression, and postpartum depression has therapeutic benefits. ECT is helpful for depressed patients with suicidal tendencies, which is important because psychotic depression increases the risk of suicidal ideation. The remission rates after ECT often exceed 50% among patients with depressive disorders, according to a paper by P. Guney et al. in the December 2020 issue of The Journal of ECT. The paper confirmed ECT could improve health-related quality of life in both genders and across all age groups.
When it comes to the effectiveness of ECT, this therapy was significantly associated with a lowered risk of suicide in patients with MDD with psychotic features and those aged 45 to 64 years, according to a study that I. Ronnqvist et al. published in July 2021 issue of JAMA Network Open. The remission rates are higher and occur earlier when ECT is used for depression with psychotic features than in patients with non-psychotic depression, as per findings of a clinical trial by G. Petrides et al. published in the December 2001 issue of The Journal of ECT.
It may take around six treatments to notice improvements with ECT, but full improvement may take longer, according to Mayo Clinic. The ECT is usually given twice a week for three to six weeks. That means, mental health resource website Mind explains, that patients may need six to 12 sessions.
What are the complications of psychotic depression treatment?
The complications of psychotic depression treatment are side effects of medications and ECT used to manage symptoms of this condition. For example, antidepressants such as SSRIs may cause side effects such as nausea and/or vomiting, diarrhea, headache, dry mouth, drowsiness, weight loss or weight gain, dizziness, nervousness or restlessness and agitation, insomnia, and sexual problems such as low sex drive and erectile dysfunction. Mayo Clinic explains that adverse reactions tend to go away after a few weeks of treatment. If the side effects are persistent, the patient may want to consider consulting a doctor who may prescribe a different medication.
On rare occasions, SSRIs may lead to serotonin syndrome, which occurs with the accumulation of high levels of this neurotransmitter in the body. Symptoms of serotonin syndrome include agitation, anxiety, sweating, high fever, lack of coordination, and rapid heart rate.
Antipsychotics may cause side effects such as weight gain, constipation, dry mouth, and urinary retention. Drug-induced movement disorders can occur with both first- and second-generation antipsychotics. These disorders include akathisia (inability to hold still) and tardive dyskinesia (uncontrolled face muscle movements). Antipsychotics may affect heart rhythm and cause orthostatic hypotension (when blood pressure drops as a person stands up or sits down too quickly). Cleveland Clinic explains that antipsychotic medications may cause high blood sugar and high cholesterol, dizziness, and increase the risk of falls and injuries. Other complications of antipsychotic medications include immune disruption, jaundice, and high levels of the hormone prolactin.
Right after the treatment with ECT, a patient may experience immediate side effects such as drowsiness, headache, confusion, muscle aches, loss of appetite, and feeling sick. Long-term side effects of ECT include loss of interest, creativity, and energy, decreased emotional responses, and difficulty concentrating and learning new information. Memory loss may occur after ECT, but this complication is usually short-term.
Can psychotic depression be treated?
Yes, psychotic depression can be treated, but not entirely cured. A patient may need ongoing treatment. A review from 1996, titled Psychotic Depression in the Journal of Clinical Psychiatry confirmed the prognostic disadvantage of psychotic depression. More precisely, the paper showed that psychotic features might recur at high rates in subsequent episodes, which means these symptoms in MDD have a lifelong significance.
Major depressive disorder is difficult to treat because it is a complex mental illness that distorts the perception of reality, self-esteem, and thinking pattern. A patient may find it difficult to get out of a depressive state, which is why a well-structured treatment and support system is vital.
Even though psychotic depression is often debilitating, it is possible to manage its effects and improve the overall quality of life. WebMD explains that people can recover from symptoms of psychotic depression, but medical follow-up may be necessary.
How to prevent having psychotic depression?
In order to prevent having psychotic depression, a patient may want to process their trauma in a healthy manner. Witnessing or experiencing trauma can increase the risk of psychotic depression. Finding a healthy way to process trauma, such as therapy, may help lower the risk of psychotic depression. Keep in mind, however, there is no foolproof strategy to prevent or avoid psychotic depression entirely. What patients can do is they can prevent relapse and complications including suicidal ideation.
Stressful life events and problems such as financial worries may trigger symptoms of psychosis. Manage stress and worry in a healthy manner through relaxation strategies. These strategies include deep breathing, mindfulness, yoga, reading, and writing. There are no rules in terms of relaxation strategies, the most important thing is that a patient chooses the approach that works best for them. By learning to manage stressful times, it becomes easier to lessen their impact on mental health.
Identify triggers of psychotic or depressive symptoms. Once the triggers are identified, make sure to create a plan to avoid them entirely or reduce exposure to those factors. Besides stress, it can be any event that reminds of past trauma, drinking alcohol, or substance use. A good way to identify triggers is to keep a diary of what is happening before and during psychotic episodes. Asking friends and family can be helpful since they can provide valuable insight into a person’s behavior.
Don’t be afraid to ask friends and family for their support while recovering from psychotic depression or when tough times come along. Their support can have a positive or empowering influence on mental well-being and helps deal with problems in a healthier manner.
How to deal with psychotic depression?
In order to deal with psychotic depression, making lifestyle modifications is necessary. Modify diet by reducing intake of unhealthy, heavily processed foods and increasing consumption of nutritious foods mainly fruits and vegetables. For example, a healthy diet such as the Mediterranean diet can help manage depression and protect against its symptoms, according to a review by O. Pano et al. in the November 2021 issue of the World Journal of Psychiatry. In addition to healthy eating, regular exercise also helps deal with psychotic depression because it has a positive effect on the mind and body.
Practice mindfulness and relaxation to reduce stress and decrease the intensity of the symptoms of this condition. Engage in hobbies and activities in order to improve mood. Get enough sleep in order to support both mental and physical health and well-being. Avoid alcohol and drugs because they could worsen the symptoms of psychotic depression. Make sure to set realistic goals regarding recovery and ask friends and family to help achieve them. Create a crisis plan that consists of everything necessary during psychotic episodes, in which a person is unable to tell their friends or family when the episodes occur.
Adhere to the treatment approach recommended by the doctor. Engage in treatment and provide valuable and honest insight into how medications and therapy or ECT make you feel. That way, the doctor will know whether they need to modify the treatment or not.
What is the difference between psychotic depression and major depression?
The difference between psychotic depression and major depression is that the latter is a specific mental illness. Psychotic depression is just one form of major depression. That is the first point of difference between the two. The second difference is that major depression (without psychotic features) doesn’t include symptoms of psychosis such as hallucinations and delusions. On the flip side, psychotic depression involves hallucinations and/or delusions.
The third major difference between the two is that psychotic depression includes more numerous symptoms and they are more severe. People with psychotic depression are at a higher risk of suicide than their counterparts with non-psychotic depression, as discussed above in this post.
The fourth major difference between psychotic depression and major depression is in the treatment. Patients with major depression may need antidepressants and therapy, whereas people with psychotic depression need antidepressants, antipsychotics, and more advanced treatments such as ECT.
The fifth difference between psychotic depression and major depression is that the latter may be easier to treat. A comparative study by M. Buoli et al. in the August 2013 issue of the Asian Journal of Psychiatry found that patients with psychotic depression had a more severe course of illness, longer hospitalizations, and lower rates of remission. Additionally, they more frequently showed a family history of major psychoses thus suggesting a continuum in disorders involving psychosis.
What is the difference between psychotic depression and schizophrenia?
The difference between psychotic depression and schizophrenia is that the latter is categorized as a psychotic disorder, whereas psychotic depression is a form of MDD, a mood disorder. That is the first difference between these conditions. The second difference is that psychotic depression includes symptoms of depression and psychosis, whereas schizophrenia only includes psychotic symptoms.
The third difference is that people with psychotic depression have delusions or hallucinations that are consistent with the theme of their depression (failure or worthlessness). On the flip side, hallucinations and delusions in schizophrenia tend to be more bizarre and have no apparent connection to a person’s mood.
The fourth difference between psychotic depression and schizophrenia is that in the former, psychotic features are episodic and they only occur during the episode of major depression. People with schizophrenia experience psychotic symptoms without identifiable mood disorders, according to a paper by Anthony J. Rothschild in the April 2013 issue of Schizophrenia Bulletin.
The fifth difference between psychotic depression and schizophrenia is that the treatment of psychotic depression is more extensive, with a combination of antidepressants and antipsychotics in addition to ECT and talk therapy. A person with schizophrenia may need antipsychotics and psychotherapy.

