Postpartum depression: definition, causes, symptoms, and treatments

Postpartum depression is a mood disorder emerging after childbirth marked by persistent sadness, anxiety, and emotional fatigue. The illness affects an individual’s capacity for self-care and infant care, often interfering with everyday activities and attachment.
The causes of postpartum depression include hormonal changes, physical recovery from stress, genetic predisposition, environmental pressures, and social support deficits.
The symptoms of postpartum depression include emotional changes, sleep disturbances, behavioral changes, physical manifestations, cognitive symptoms, and social withdrawal.
The available treatments for postpartum depression are antidepressant medications, psychotherapy, combination therapy, and early intervention care.
What is postpartum depression?
Postpartum depression (PPD) is a serious mood disorder affecting individuals within one year after childbirth. PPD is a type of depression characterized by intense feelings of sadness, anxiety, and despair that interfere with daily functioning.
Postpartum depression differs significantly from temporary “baby blues,” a condition affecting up to 80% of new mothers, according to a 2023 paper by Modak et al., titled “A Comprehensive Review of Motherhood and Mental Health: Postpartum Mood Disorders in Focus.”
According to a publication by Carlson et al., last updated in January 2025, titled “Perinatal Depression,” perinatal depression is now a term encompassing postpartum depression, following the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, Text Revision (DSM-5-TR). Depression during such a period is marked by prolonged emotional distress affecting a person’s ability to care for themselves and their newborn.
Peripartum depression is defined as a serious depressive episode known to start during pregnancy or within four weeks of giving birth. The scope of the term includes both prenatal and postpartum depression.
What is the other term for postpartum depression?
The other term for postpartum depression is perinatal depression or postnatal depression (PND). Medical community recognizes PPD as the common acronym.
Medical professionals in the United Kingdom and Commonwealth countries typically use postnatal depression, while postpartum depression is more common in North American medical literature.
The United States Food and Drug Administration (US FDA), in a 2023 news release, titled “FDA Approves First Oral Treatment for Postpartum Depression,” used the term postpartum depression to announce the approval of Zurzuvae (zuranolone) as the first oral medicine for treating PPD in adults.
How common is postpartum depression?
Postpartum depression is a common mood disorder affecting 10–15% of adult mothers annually, with depressive symptoms persisting for more than six months in 25–50% of sufferers, according to a 2018 paper by Anokye et al., titled “Prevalence of postpartum depression and interventions utilized for its management.”
A publication from the National Health Service, last reviewed in August 2022, titled “Overview – Postnatal Depression,” substantiated the incidence of PPD, indicating the disorder affects about 1 in 10 women within a year following childbirth. Postpartum depression impacts fathers and partners as well.
What is the difference between postpartum depression and baby blues?

The difference between postpartum depression and baby blues refers to the distinction between two types of emotional experiences emerging after childbirth. The differences between postpartum depression and baby blues are listed below.
- Occurrence rate: Baby blues affect 70-80% of new mothers, according to an article titled “Baby Blues vs. Postpartum Depression” from the South Dakota Department of Health,” while postpartum depression impacts approximately 1 in 10 women after childbirth.
- Timing and duration: Baby blues typically appear between the third and fifth day after childbirth and resolve within two weeks. Postpartum depression develops between two to eight weeks postpartum and tends to persist up to one year after delivery.
- Symptom severity: Baby blues present as mild mood swings, crying spells, and temporary anxiety that naturally subside. Postpartum depression manifests as persistent severe symptoms including extreme sadness, despair, and clinical anxiety requiring professional intervention.
- Treatment requirements: Baby blues are self-limiting and resolve without medical intervention. Postpartum depression requires professional treatment including medication, therapy, or a combination of both approaches.
When does postpartum depression start?
Postpartum depression (PPD) typically begins between 2-8 weeks after childbirth, though onset is possible anytime within the first year postpartum. Clinical presentation varies by onset timing. Early onset cases often show more severe symptoms.
Delayed onset cases develop more gradually. Both onset patterns require professional evaluation for proper treatment. According to a 2024 study by Radoš et al., titled “Diagnosis of peripartum depression disorder: A state-of-the-art approach from the COST Action Riseup-PPD,” women with postpartum depression (PPD) who experienced onset within the initial eight weeks postpartum exhibited more severe depression, identified as the subtype anxious anhedonia.
Postpartum onset was linked to obsessive-compulsive and psychotic symptoms, whereas pregnancy onset was more closely linked to psychosocial stressors.
How long does postpartum depression last?
Postpartum depression lasts between a few months to one year with consistent treatment. However, without proper treatment, symptoms potentially persist for up to three years. It is worth noting that postpartum depression duration varies among individuals.
To determine how long PPD lasts, understanding its typical duration patterns is essential. Recovery often improves with early intervention, though the timeline differs for each person based on the severity and response to treatment.
Who is at risk for postpartum depression?
First-time mothers, mothers under 25 years old, mothers of twins, individuals with a history of depression, and females experiencing significant hormonal changes after childbirth are at risk for postpartum depression.
Results of a 2022 study by Bradshaw et al., titled “Risk factors associated with postpartum depressive symptoms: A multinational study” revealed first-time mothers face elevated risks of PPD due to the significant life adjustments and new responsibilities of parenthood. Younger mothers often have less financial stability, social support, and relationship stability. Multiple birth mothers caring for twins encounter increased physical demands and stress levels contributing to PPD risk.
As per a 2017 report by Silverman et al., titled “The Risk Factors for Postpartum Depression: A Population Based Study,” compared to women without a history of depression, females with a history were 21 times more likely to develop PPD.
Women with thyroid imbalances or other endocrine disorders experience additional biological risk factors for developing postpartum depression.
How to prevent having a postpartum depression?
To prevent having a postpartum depression, pregnant individuals must establish early support systems before delivery. Postpartum depression risk decreases when individuals maintain healthy sleep patterns during pregnancy and after birth.
Open communication with partners about emotions and concerns contributes to reducing one’s risk of PPD as well. Accepting support from family and friends for newborn care further lessens the likelihood of developing symptoms. Regular check-ups with healthcare providers after delivery play a key role in prevention and early intervention.
How is postpartum depression diagnosed?
Postpartum depression is diagnosed by starting with a thorough screening using the Edinburgh Postnatal Depression Scale (EPDS). PPD screening examines symptoms occurring within the first year after childbirth. Healthcare providers assess the severity and duration of symptoms through detailed patient interviews.
Doctors additionally order laboratory tests to check thyroid function and other relevant markers. Mental health specialists evaluate the impact of symptoms on mother-child bonding and relationships.
In a 2023 study by Atuhaire et al., titled “Validating the Edinburgh Postnatal Depression Scale Against the Diagnostic and Statistical Manual of Mental Disorders, 5th Edition for Use in Uganda,” the EPDS accurately detected 86.8% of genuine PPD cases, establishing the tool’s validity and reliability in detecting the majority of PPD cases without necessitating highly qualified mental health professionals—crucial for areas with limited resources.
What can I expect from postpartum depression?
One can expect a range of emotional and physical symptoms from postpartum depression. Persistent sadness, hopelessness, or emotional numbness become part of daily life. Mood swings, frequent crying, and irritability often feel overwhelming.
A sense of disconnection from the baby or difficulty bonding potentially occurs. Fatigue and lack of motivation interfere with basic tasks and self-care. Appetite changes and disrupted sleep—beyond typical new-parent exhaustion—are common as well. Concentration problems or feelings of guilt and worthlessness often worsen the condition.
How to deal with postpartum depression?
To deal with postpartum depression, postpartum individuals must seek professional medical evaluation immediately upon noticing persistent feelings of sadness or anxiety. The most commonly utilized way to treat PPD involves a combination of professional counseling and medication prescribed by healthcare providers.
Recovering from postpartum depression involves creating a solid support system including loved ones and medical professionals. Joining support groups tailored for new parents provides a sense of community and shared understanding.
Healing often includes engaging in self-care habits such as light physical activity and maintaining a balanced diet. Involvement from a postpartum care team—consisting of doctors, therapists, and nurses—ensures consistent monitoring and guidance throughout the recovery process.
What are the causes of postpartum depression?
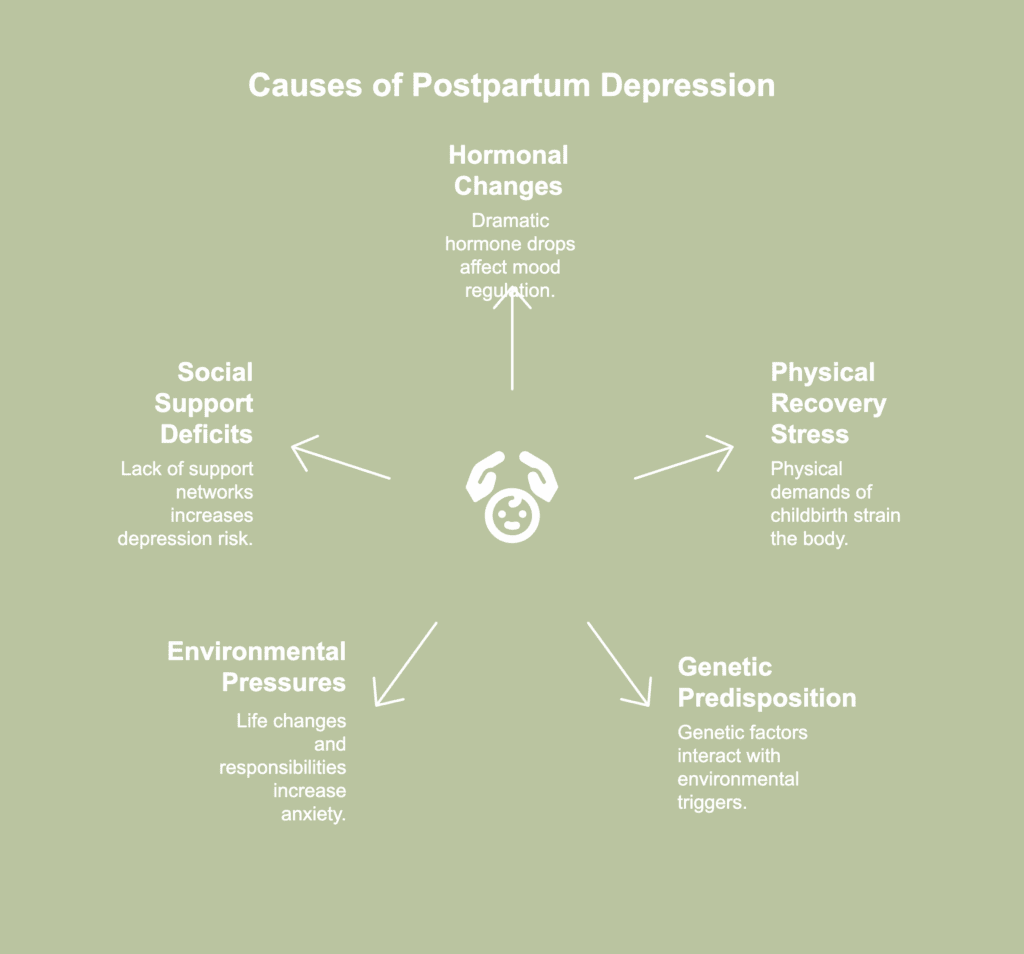
Causes of postpartum depression denote the diverse factors driving the onset of depressive symptoms subsequent to childbirth. The causes of postpartum depression are listed below.
- Hormonal changes: Dramatic drops in estrogen and progesterone levels immediately after childbirth trigger chemical changes in the brain. Hormonal fluctuations affect neurotransmitter function and mood regulation during the first two weeks postpartum, leading to both baby blues and potential depression.
- Physical recovery from stress: Physical demands of childbirth and recovery create significant bodily strain. Labor complications, cesarean delivery recovery, and sleep deprivation overwhelm the body’s natural healing processes, contributing to mood disturbances and increased risk of depression.
- Genetic predisposition: Postpartum depression seems to be influenced by intricate gene-environment interactions. Genetic predisposition—particularly in serotonin and stress control systems—necessitates environmental and hormonal circumstances (e.g., stress during birthing) for expression, according to a 2015 paper by Couto et al., titled “Postpartum depression: A systematic review of the genetics involved.”
- Environmental pressures: New parent responsibilities, financial strain, and changes in family dynamics create drastic life changes. Demands of infant care, career changes, and relationship modifications contribute to overwhelming anxiety levels and emotional instability.
- Social support deficits: Lack of family support, isolation from social networks, and limited access to healthcare resources increase depression risk. Single parents and individuals with limited community connections experience higher rates of postpartum mood disorders.
What are the symptoms of postpartum depression?
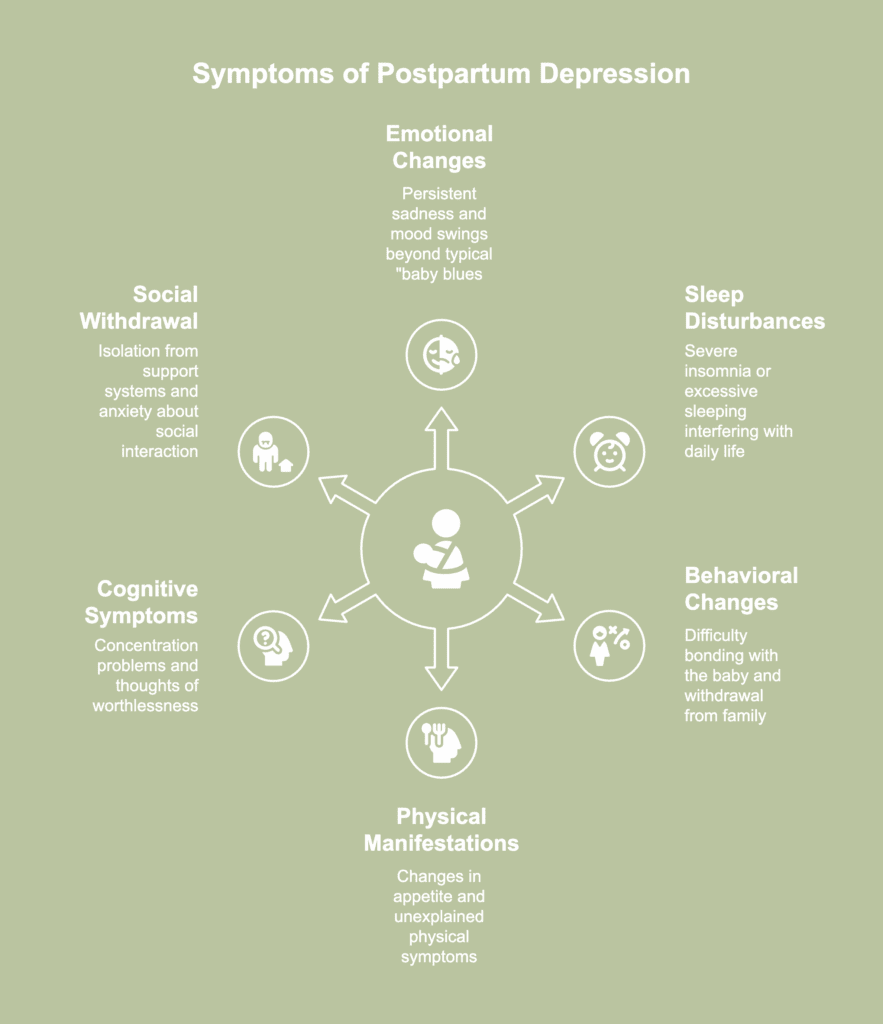
Symptoms of postpartum depression refer to the signs indicating the presence of depression after childbirth. The symptoms of postpartum depression are listed below.
- Emotional changes: Persistent feelings of sadness, hopelessness, and despair characterize postpartum depression. New mothers experience frequent crying spells, severe mood swings, and overwhelming anxiety lasting beyond the typical “baby blues” period of two weeks.
- Sleep disturbances: Changes in sleep patterns extend beyond normal new parent fatigue. Mothers experience severe insomnia even when the baby is sleeping, or conversely, excessive sleeping that interferes with daily responsibilities.
- Behavioral changes: Extreme difficulty bonding with the baby or withdrawal from family relationships emerge as prominent symptoms. Mothers tend to show disinterest in previously enjoyed activities, avoid social interactions, or experience panic attacks in social situations.
- Physical manifestations: Notable changes in appetite patterns occur, either eating more or less than usual. Physical symptoms include unexplained headaches, digestive problems, and chronic fatigue persisting beyond normal postpartum recovery.
- Cognitive symptoms: Severe concentration problems and difficulty making decisions impact daily functioning. Recurring thoughts of worthlessness often arise, along with overwhelming guilt related to parenting responsibilities, and in more serious situations, thoughts of self-harm develop.
- Social withdrawal: Complete isolation from support systems and inability to ask for help characterize severe cases. Intense anxiety about leaving the house or engaging with others often emerges, further deepening the sense of isolation.
What are the available treatments for postpartum depression?

Available treatments for postpartum depression are highly individualized and depend on symptom severity and patient preferences. The available treatments for postpartum depression are listed below.
- Antidepressant medications: The first-choice drugs for perinatal depression are selective serotonin reuptake inhibitors. For medical therapy, sertraline or escitalopram are suitable first-line options. Sertraline has a wealth of reassuring safety research. Fluoxetine and paroxetine are possible choices to be considered if they have been previously effective for a specific individual, according to an article by Carlson et al., last updated in January 2025, titled “Perinatal Depression.” The FDA recently approved Zurzuvae (zuranolone) as the first oral medication specifically for postpartum depression treatment.
- Psychotherapy: Professional counseling and talk therapy provide essential mental health support for mild-to-moderate cases. Therapy helps mothers develop coping strategies and process emotional challenges during the postpartum period.
- Combination therapy: For many women, a combined approach using both antidepressant medication and psychotherapy offers the most comprehensive treatment. Dual approach addresses both biological and psychological aspects of postpartum depression.
- Early intervention care: Healthcare providers actively screen and monitor new mothers for symptoms, enabling early treatment intervention. Regular check-ups with doctors, midwives, or health visitors help identify and address postpartum depression symptoms promptly.

