Paranoid schizophrenia: definition, symptoms, treatments
Table of content
- What is paranoid schizophrenia?
- What are the symptoms of paranoid schizophrenia?
- What are the causes of paranoid schizophrenia?
- How does paranoid schizophrenia affect the body?
- What are the possible treatments for paranoid schizophrenia?
- What is the difference between paranoid schizophrenia and paranoid personality disorder?
Paranoid schizophrenia is a chronic mental disorder marked by persistent delusions and auditory hallucinations, often centered on persecution, conspiracy, or grandeur. Cognitive function and emotional responsiveness remain relatively intact compared to other forms of schizophrenia.
Paranoid schizophrenia is an outdated term because the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) no longer recognizes schizophrenia subtypes, including paranoid, disorganized, and catatonic types.
Instead, the DSM-5 classifies schizophrenia as a single disorder with varying symptoms, emphasizing a dimensional approach rather than outdated term-based subcategories.
The symptoms of paranoid schizophrenia are delusions, hallucinations, disorganized or incoherent speech, disorganized or unusual behavior, and negative symptoms.
The possible treatments for paranoid schizophrenia include psychotherapy and electroconvulsive therapy (ECT).
What is paranoid schizophrenia?
Paranoid schizophrenia, previously considered a distinct type of schizophrenia, is a long-term mental disorder characterized by deeply ingrained false beliefs and sensory distortions, often accompanied by paranoia.
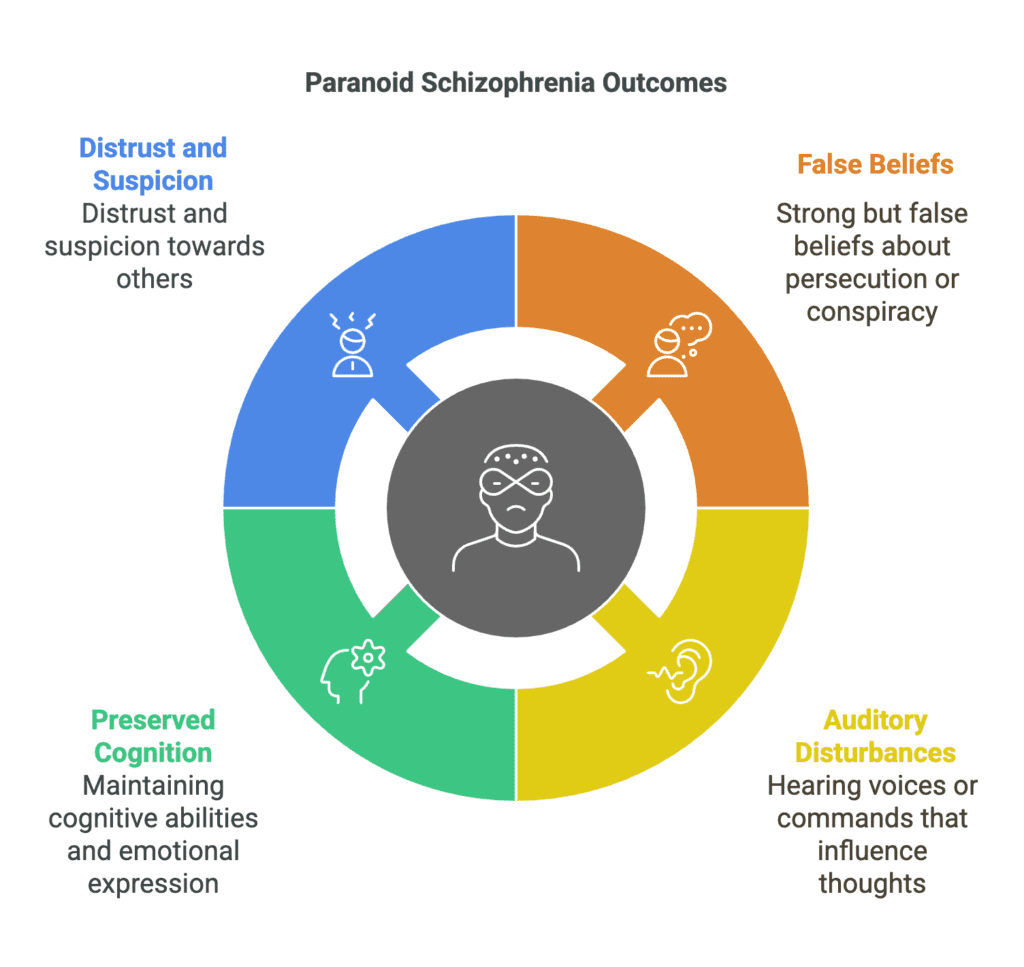
Individuals experiencing the condition frequently hold strong but false beliefs related to persecution, conspiracy, or grandeur, leading to distrust and suspicion of others. Auditory disturbances often manifest as voices issuing commands, providing commentary, or strengthening deceptive thoughts.
Unlike other forms of schizophrenia, cognitive abilities and emotional expression often remain relatively preserved, allowing individuals to function at a higher level in daily life.
Nearly 50% of people seeking initial treatment for a psychotic diagnosis exhibit paranoia, the most often reported delusion among patients with schizophrenia spectrum disorders, according to a 2016 paper by Pinkham et al., titled “Paranoid individuals with schizophrenia show greater social cognitive bias and worse social functioning than non-paranoid individuals with schizophrenia.”
Is paranoid schizophrenia in the DSM-5?
No, paranoid schizophrenia is no longer in the DSM-5. Formerly classified as a separate form, paranoid schizophrenia was removed to reflect a broader understanding of schizophrenia as a spectrum disorder.
The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) no longer categorizes schizophrenia into rigid subtypes, as symptoms often overlap and change over time.
Paranoid schizophrenia was once a separate diagnosis, but no longer holds such a distinction. The DSM-4 categorized schizophrenia as a spectrum disorder with multiple subtypes. Among them, the paranoid form ranked as the most prevalent and severe.
The release of the DSM-5 brought significant changes. The updated edition removed schizophrenia subcategories entirely. With the elimination of subtypes, diagnosis and treatment have grown more flexible, concentrating on the severity of each particular symptom rather than utilizing predetermined categories.
Paranoia is still a prevalent symptom of schizophrenia, but it is regarded as one of many possible symptoms rather than a distinguishing trait of a certain type.
Is paranoid schizophrenia still considered a subtype of schizophrenia?
No, paranoid schizophrenia is no longer considered a subtype of schizophrenia. The American Psychiatric Association (APA) removed all schizophrenia subtypes, including the paranoid form, from the DSM-5.
A 2014 study by Mattila et al., titled “Impact of DSM-5 Changes on the Diagnosis and Acute Treatment of Schizophrenia” identified several reasons for the removal of schizophrenia subtypes from the psychiatry text, including the inability of classifications to reflect the disorder’s diverse effects on individuals.
Categories lacked stability over time, with patients shifting between groups, and some were rarely applied in clinical practice. Studies found no significant differences in background or thinking abilities among people assigned to separate subtypes, nor did classifications help predict illness progression or treatment response.
Additionally, when researchers attempted to group patients based on symptoms, many did not align with a specific category. Due to such limitations, DSM-5 introduced a more flexible, symptom-based approach designed to reflect each patient’s unique experiences more accurately.
How common is paranoid schizophrenia?
Paranoid schizophrenia is relatively uncommon. While the condition is no longer part of formal diagnoses, schizophrenia, sometimes involving paranoia, remains a serious but rare mental disorder, affecting roughly 1 in 300 individuals or 24 million people within the global population, according to a 2022 publication from the World Health Organization, titled “Schizophrenia.”
A 2022 study by Adhikari et al., titled “Differentiating Childhood-Onset Schizophrenia From Other Childhood Disorders” stated that very early-onset schizophrenia, or childhood-onset schizophrenia (COS), characterized by symptoms beginning before the age of 13, is uncommon, and its global prevalence remains undetermined.
The estimated incidence in the United States is approximately 0.04% within the general population. The worldwide rate of early-onset schizophrenia (symptoms manifesting before the age of 18) is estimated at approximately 0.5%.
Finally, according to a 2019 report by Tampi et al., titled “Psychotic disorders in late life: a narrative review,” schizophrenia has a prevalence of 0.1% to 0.5% in the elderly population.
What are the symptoms of paranoid schizophrenia?
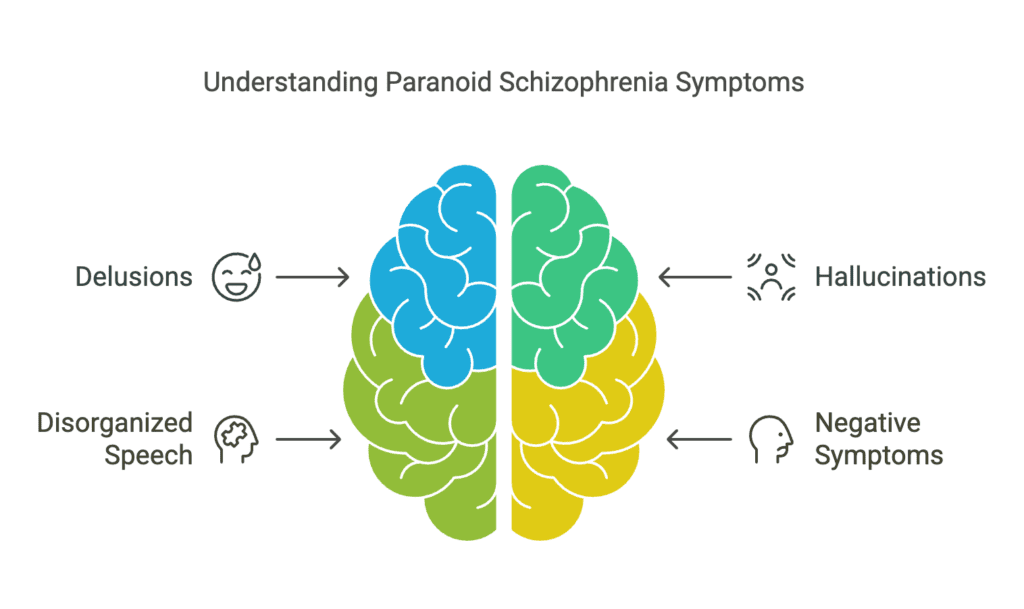
Symptoms of paranoid schizophrenia describe the manifestations of schizophrenia wherein paranoia is a defining characteristic. The symptoms of paranoid schizophrenia are listed below.
- Delusions
- Hallucinations
- Disorganized or incoherent speech
- Negative symptoms
1. Delusions
Delusions are a symptom of paranoid schizophrenia because deeply held false beliefs alter perception of reality and shape behavior. Individuals with the condition often develop strong convictions about being persecuted, watched, or targeted by conspiracies, even without supporting evidence.
Irrational assumptions foster intense distrust of others, complicating social interactions and resulting in isolation. Grandiose delusions additionally emerge, with individuals convinced of possessing extraordinary abilities, power, or a special purpose.
Such rigid ideas persist in the face of contradicting evidence, fueling psychological stress and paranoia. Delusions compromise judgment, therefore impairing daily performance and decision-making.
2. Hallucinations
Hallucinations signify the presence of paranoid schizophrenia, as false sensory perceptions seem real, causing confusion and distress. Hearing voices is the most common type, with individuals perceiving sounds others cannot detect.
The voices often issue commands, provide commentary on actions, or reinforce delusions, increasing paranoia and fear. Some hear multiple voices engaging in conversations, arguing, or whispering threatening messages.
A 2023 paper by Kakar et al., titled “A Phenomenal Depiction of Paranoid Schizophrenia With Auditory Hallucinations: A Case Report” provided a clinical case of a 59-year-old individual with paranoid schizophrenia.
The patient mostly had auditory hallucinations, paranoid delusions, and aggressive conduct. Voices instructed the man to take action. This heightened his mistrust and drove him to think his wife was trying to kill him. Particularly in cases when hallucinations include “command voices” the patient believes to be genuine, aggression is often linked with paranoid schizophrenia.
3. Disorganized or incoherent speech
Disorganized or incoherent speech reflects disruptions in thinking, making communication difficult for individuals with paranoid schizophrenia. Fragmented thoughts result in sentences lacking logical connections or shifting rapidly between unrelated topics.
Jumbled words make conversations difficult to follow and intentions harder to understand. Disorganized speech often reflects underlying cognitive disturbances, with the brain struggling to process and organize information effectively.
Confused verbal expression shapes behavior, as unclear communication causes frustration, withdrawal, or misunderstandings in social settings. Affected individuals repeat words excessively, invent new phrases, or stop speaking mid-sentence after losing track of thoughts.
4. Disorganized or unusual behavior
Disorganized or unusual behavior in paranoid schizophrenia appears through unpredictable actions disrupting daily functioning. Bizarre responses to situations, such as laughing at inappropriate times or wearing heavy clothing in hot weather, reflect impaired judgment.
Motor disturbances appear as repetitive movements, unusual postures, or sudden agitation without clear reasons. Certain individuals display abnormal gestures, pace aimlessly, or remain motionless for extended periods.
Behavioral patterns hinder social interactions, making relationships harder to maintain and routines challenging to follow. Impulsivity and erratic behavior raise safety concerns because affected people struggle to assess risks.
5. Negative symptoms
Negative symptoms involve a decrease in normal emotional expression, motivation, and social engagement. Affected individuals often display a flat affect, showing little facial expression or vocal variation, making interactions seem unresponsive.
Speech becomes limited, with responses reduced to short phrases or a lack of spontaneous conversation. Motivation declines, leading to difficulty initiating tasks, maintaining personal hygiene, or completing daily responsibilities. Social withdrawal becomes common, as individuals struggle to form or sustain relationships due to a lack of interest or emotional connection.
According to a 2017 paper by Stephen R. Marder and Silvana Galderisi, titled “The current conceptualization of negative symptoms in schizophrenia,” poor functional outcomes are most notably predicted by negative symptoms. However, present treatments fall short in sufficiently targeting negative symptoms, therefore new approaches are crucial.
When does paranoid schizophrenia occur?
Paranoid schizophrenia usually occurs in late adolescence or early adulthood, with signs often appearing from the late teenage years to the early 30s, though onset at a later age remains possible.
Early symptoms tend to be subtle, making detection difficult before more severe manifestations emerge. Males commonly experience onset during the late teens or early 20s, while females tend to show symptoms at a slightly later age. Stressful life experiences, inherited traits, and brain chemistry influence the timing of appearance.
How is paranoid schizophrenia diagnosed?
Paranoid schizophrenia is diagnosed by evaluating symptoms and ruling out other potential illnesses. A physical exam aids in the identification of medical causes impacting cognitive or behavioral problems.
Imaging tools like MRI or CT scans as well as blood testing help identify neurological diseases or reasons connected to drugs. Questions regarding medical history, symptoms, and family history are part of clinical interviews.
Examinations of mental status evaluate cognitive abilities, emotional reactions, and thought processes. Diagnosis follows DSM-5 criteria, requiring delusions, hallucinations, disorganized speech, or other impairments to persist for a significant period.
According to a 2010 article by Assen Jablensky, titled “The diagnostic concept of schizophrenia: its history, evolution, and future prospects,” no definitive biological markers for schizophrenia have been identified; the condition is instead defined by symptoms, functional impairments, and an unpredictable progression.
Research has suggested possible biological signs, though none have proven sufficient for diagnosis. Identified factors include neurocognitive dysfunction, structural brain differences, and neurochemical disruptions.
What are the causes of paranoid schizophrenia?
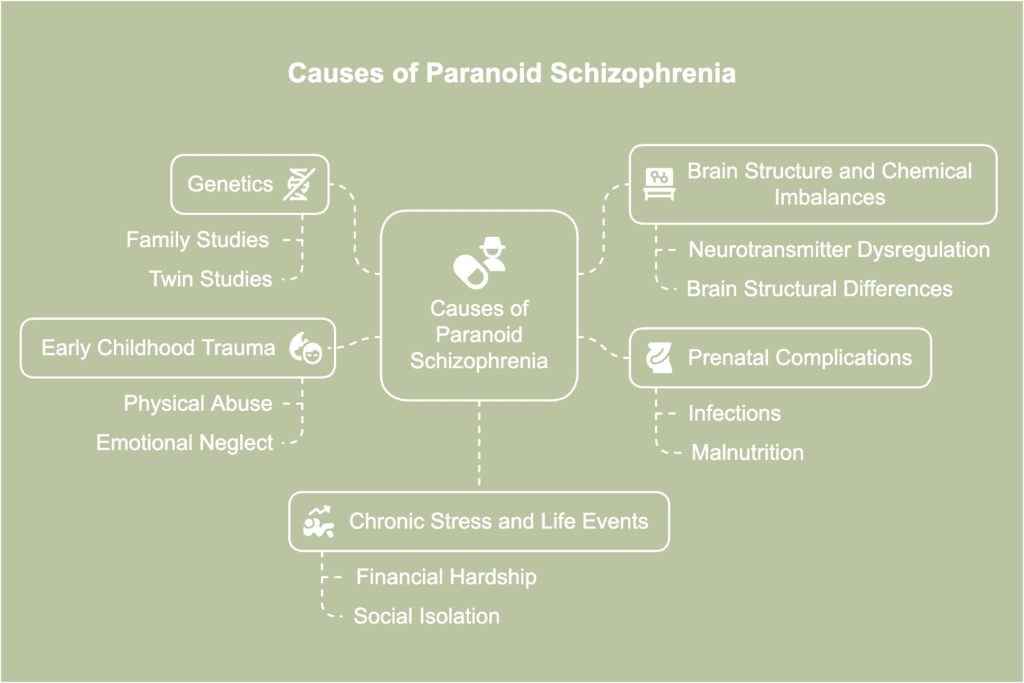
Causes of paranoid schizophrenia concern different factors influencing the onset of the disorder. The causes of paranoid schizophrenia are listed below.
- Genetics: Schizophrenia often runs in families, suggesting a genetic link in its development. Although no single gene has been found to be the sole cause of schizophrenia, twin and family studies consistently demonstrate a significant genetic component, according to a 2010 study by Gejman et al., titled “The Role of Genetics in the Etiology of Schizophrenia.” Rather, schizophrenia seems to be polygenic, meaning it emerges as a result of several genetic variations.
- Brain structure and chemical imbalances: Schizophrenia has been associated with neurotransmitter dysregulation, specifically in the dopamine, glutamate, and gamma-aminobutyric acid (GABA) systems. As per a 2023 study by Xu et al., titled “Changes in neurotransmitter levels, brain structural characteristics, and their correlation with PANSS scores in patients with first episode schizophrenia,” brain scans reveal structural differences in specific areas, such as the corpus callosum connecting the brain’s left and right sides and the ventricles, fluid-filled spaces that appear enlarged or shaped differently in schizophrenic patients.
- Prenatal complications: Exposure to infections, malnutrition, or oxygen deprivation during fetal development increases schizophrenia risk. Viral infections affecting the mother during pregnancy disrupt brain formation, leading to long-term neurodevelopmental issues. Birth complications, such as premature labor or low birth weight, have been associated with a higher likelihood of developing schizophrenia later in life.
- Early childhood trauma: Adverse childhood experiences, such as physical abuse, emotional neglect, or severe stress, contribute to schizophrenia development. Chronic exposure to trauma affects brain development, altering stress response mechanisms and increasing susceptibility to psychotic symptoms. Repeated traumatic events potentially lead to paranoia and distorted thought patterns, reinforcing the risk of delusions. Individuals with a genetic predisposition are particularly vulnerable when exposed to childhood adversity.
- Chronic stress and life events: Prolonged exposure to stressful situations, such as financial hardship, social isolation, or major life changes, contribute to schizophrenia onset. High stress levels influence cortisol production, affecting brain function and increasing vulnerability to psychotic episodes. Stressful environments additionally worsen existing symptoms, leading to greater paranoia and disorganized thinking. While stress alone does not lead to schizophrenia, exposure to high levels trigger symptoms in individuals with underlying risk factors.
What are the risk factors for paranoid schizophrenia?
Risk factors for paranoid schizophrenia refer to various influences increasing the likelihood of developing the mental disorder. The risk factors for paranoid schizophrenia are listed below.
- Urbanization: Growing up or living in densely populated areas increases exposure to social stressors. According to a 2016 report by Davis et al., titled “A review of vulnerability and risks for schizophrenia: Beyond the two hit hypothesis,” growing up in an urban setting correlates with a higher incidence of schizophrenia. The social defeat hypothesis explains this connection by proposing that individuals in urban areas, especially marginalized or immigrant groups, experience heightened social stress. Factors such as exclusion, discrimination, and limited community integration create psychological strain. Persistent exposure to these challenges increases vulnerability to psychotic illnesses.
- Social isolation: Lack of meaningful social connections leads to emotional distress and cognitive decline, potentially triggering schizophrenia symptoms. Individuals who withdraw from relationships or struggle with social interaction experience heightened paranoia and mistrust. Social support is essential in reducing risk, since strong connections offer stability and reassurance.
- Family history of the disorder: Having a close relative with schizophrenia raises the likelihood of developing the condition due to shared genetic and environmental factors. Individuals with an affected parent or sibling face a higher risk compared to the general population. While genetics play a significant role, environmental influences often determine whether symptoms emerge. Early awareness of family history allows for monitoring potential signs and seeking support if needed.
- Substance abuse: Substance use during adolescence or early adulthood, when the brain is still developing, increases the likelihood of long-term mental health disturbances. According to findings of a 2017 paper by Khokhar et al., titled “The Link Between Schizophrenia and Substance Use Disorder: A Unifying Hypothesis,” compared to just 16% of the general population, 47% of people with schizophrenia struggle with drug or alcohol usage. Substance abuse exacerbates the symptoms of schizophrenia, increasing the chance of hospitalization and relapse, causing more severe psychotic symptoms, increasing the risk of violence and suicide, and decreasing treatment compliance.
Can paranoid schizophrenia be prevented?
No, paranoid schizophrenia cannot be prevented. Since biological and genetic factors are major contributors to the disorder’s development, there is no definitive way to prevent it. However, symptoms are less severe and long-term results are better with early management.
Looking out for warning signs—such as social disengagement or cognitive decline—allows for quick medical assistance. Managing stress, avoiding substance abuse, and maintaining strong social connections lower the risk of symptom progression. Following treatment guidelines and having access to mental health care enable people at great risk to control possible triggers.
How does paranoid schizophrenia affect the body?
Paranoid schizophrenia affects the body by changing bodily reactions and upsetting normal motor abilities. People have irregular postures, stiff muscles, or involuntary motions, impairing the ability to coordinate and control physical behavior.
Physical discomfort results from altered senses, increasing one’s sensitivity to touch, sound, or light. Fatigue and low energy levels become common due to sleep disturbances and high stress levels.
Weakened immune function increases vulnerability to infections and other illnesses. Unintended weight loss or gain occurs as appetite fluctuates, often due to medication side effects or irregular eating habits.
How does paranoid schizophrenia affect the brain?
Paranoid schizophrenia affects the brain by changing its structure and function, causing problems with perception and cognition. The cortex, responsible for processing thoughts and sensory input, undergoes changes reducing gray matter volume, impairing reasoning and awareness.
Disruptions in dopamine activity interfere with neural communication, contributing to hallucinations and delusions. Impaired connectivity among various brain regions hinders information integration and decision-making processes.
What are the possible treatments for paranoid schizophrenia?
Possible treatments for paranoid schizophrenia are several medical, therapeutic, and supporting interventions meant to control symptoms and raise quality of life. The possible treatments for paranoid schizophrenia are listed below.
- Psychotherapy
- Electroconvulsive therapy (ECT)
1. Psychotherapy
Being able to understand and deal with paranoid-type schizophrenia is made easier with psychotherapy, otherwise referred to as talk therapy. Talk therapy provides a controlled environment where patients freely talk to a qualified professional about anxieties, fears, and delusions.
Cognitive behavioral approaches challenge illogical ideas, therefore reducing the intensity of paranoid thoughts and emotional instability. A person’s ability to express concerns and handle social situations more adeptly are enhanced through talking therapy.
Stress management techniques introduced in therapy help lower emotional triggers, preventing symptom escalation. The establishment of trust with a therapist facilitates the process of confronting challenging emotions by establishing a sense of security.
2. Electroconvulsive therapy (ECT)
Electroconvulsive therapy (ECT) helps manage schizophrenia symptoms by stimulating brain activity through controlled electrical currents. ECT is considered when medications fail to reduce persistent delusions, hallucinations, or catatonia.
Brief seizures brought on by electrical stimulation result in neurochemical alterations known to enhance mood control and cognitive performance. Treatment-resistant schizophrenia often responds well to electroconvulsive therapy (ECT), especially in cases where other interventions have been ineffective. Sessions occur under medical supervision with anesthesia to ensure safety and minimize discomfort.
The 2017 study “Impacts of Electroconvulsive Therapy on 1-Year Outcomes in Patients With Schizophrenia: A Controlled, Population-Based Mirror-Image Study” by Lin et al., the largest to date in favor of electroconvulsive treatment, examined 2,074 ECT-treated schizophrenic patients versus a control group.
Post-treatment psychiatric hospitalization rates were considerably lower for ECT-treated patients. Patients receiving large doses of antipsychotics or clozapine additionally experienced the most significant effect.
How can you help a loved one with paranoid schizophrenia?
You can help a loved one with paranoid schizophrenia by offering patience, understanding, and consistent support. Educate yourself about the condition to recognize symptoms and challenges they are facing.
Foster a secure environment for candid dialogue by asking about personal emotions and listening without criticism. Allow personal space when necessary while maintaining a reassuring presence to prevent feelings of abandonment or isolation. Suggest joining a support group to engage with individuals facing similar challenges.
Communicate in a calm, clear manner to minimize misunderstandings and ease paranoia. Finally, recommend stress management techniques such as relaxation exercises or structured routines to help lower anxiety.
Can paranoid schizophrenia be cured?
No, schizophrenia cannot be cured. Although there is no known cure for the condition, treatment options serve to alleviate symptoms and enhance quality of life. Psychotherapy offers coping mechanisms and emotional assistance, tackling issues associated with the disease.
For patients with treatment-resistant schizophrenia, electroconvulsive therapy (ECT) lowers severe symptoms and changes brain activity. Timely intervention improves treatment results, averting the exacerbation of symptoms over time. Though a total cure is still unattainable, regular treatment helps people to maintain fulfilling lives.
What can a person expect with paranoid schizophrenia?
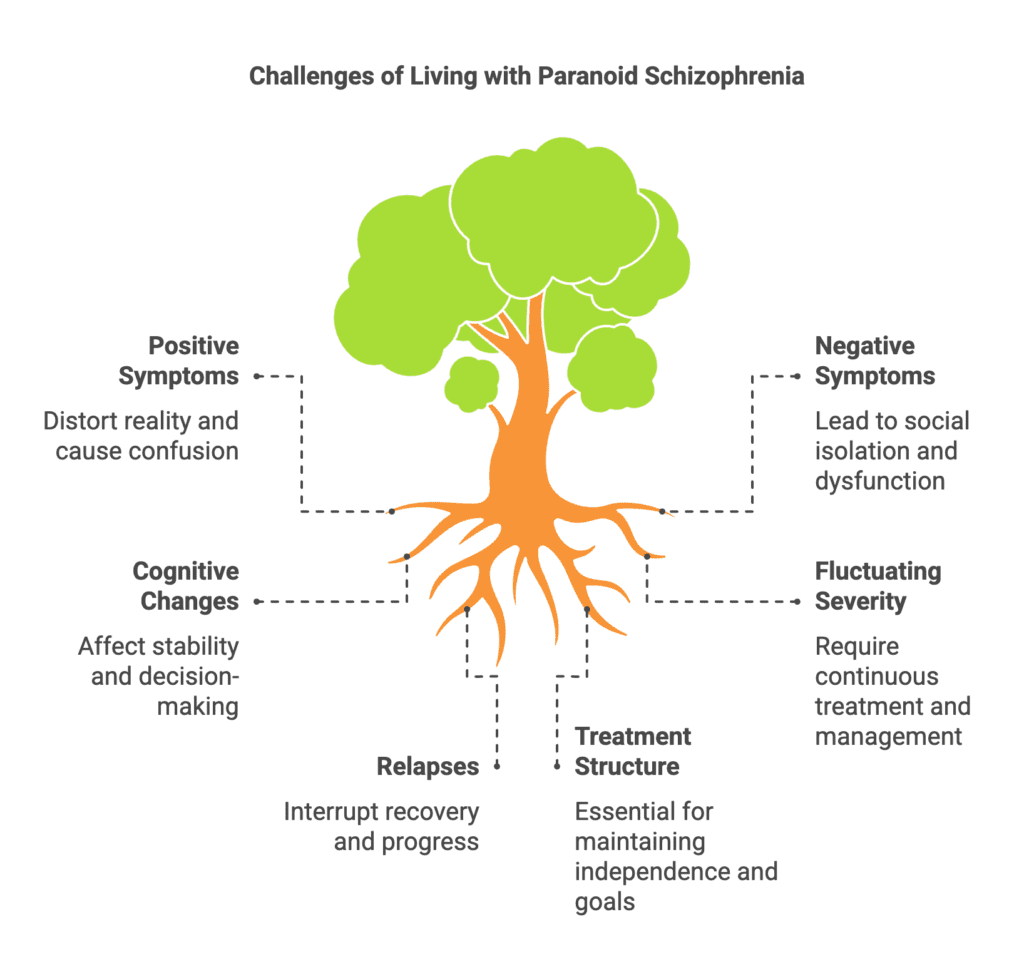
With paranoid schizophrenia, a person can expect a variety of difficulties impacting one’s ideas, feelings, and actions. Confusion and mental distress result from a warped view of reality brought forth by positive symptoms, such as delusions and hallucinations.
Negative symptoms like social isolation and limited emotional expressiveness disrupt relationships and everyday functioning. Drastic changes in cognition, mood, and drive affect general stability and decision-making.
Treatment for fluctuating symptom severity must be continuous, with possible relapses occurring after intervals of recovery. Structured treatment helps people maintain independence and reach personal objectives despite all the difficulties.
What is the difference between paranoid schizophrenia and paranoid personality disorder?
The difference between paranoid schizophrenia and paranoid personality disorder is based on the severity of symptoms, the fundamental causes, and each condition’s impact on daily life. The differences between paranoid schizophrenia and paranoid personality disorder are shown in the table below.
| Difference Between Paranoid Schizophrenia and Paranoid Personality Disorder | ||
| Feature | Paranoid schizophrenia | Paranoid personality disorder |
| Core symptoms | Delusions, hallucinations, disorganized thinking | Persistent distrust, suspicion, and hypersensitivity without delusions or hallucinations |
| Reality perception | Significant impairment; detachment from reality | Maintains a connection to reality, though overly suspicious |
| Severity | Severe, disabling mental illness | Milder but persistent personality disorder |
| Cognitive function | Impaired reasoning, memory, and organization | Generally intact cognitive function |
| Onset | Typically late teens to early adulthood | Usually emerges in early adulthood |
| Social functioning | Severe impairment in relationships and daily life | Distrustful but maintains relationships, though often strained |
| Response to criticism | Responds with paranoia and withdrawal, believing others are part of a conspiracy | Easily offended, defensive, and argumentative but without psychotic symptoms |
| Course of illness | Chronic and progressive if untreated | Chronic but stable over time |
While both conditions involve paranoia, paranoid schizophrenia causes a significant break from reality, whereas paranoid personality disorder leads to persistent distrust without delusions or hallucinations. Accurate diagnosis and customized treatment strategies facilitate symptom management and enhance quality of life.


