8 Types of Schizophrenia and their differences
Table of content
- 1. Unspecified schizophrenia
- 2. Hebephrenic schizophrenia
- 3. Paranoid schizophrenia
- 4. Undifferentiated schizophrenia
- 5. Catatonic schizophrenia
- 6. Simple schizophrenia
- 7. Residual schizophrenia
- 8. Cenesthopathic schizophrenia
- What is Schizophrenia?
Schizophrenia is a serious mental illness characterized by an impaired perception of reality. A person with schizophrenia usually has delusions, hallucinations, and symptoms such as paranoia. These symptoms affect the way they perceive the world and people around them, which can lead to erratic thoughts and behaviors.
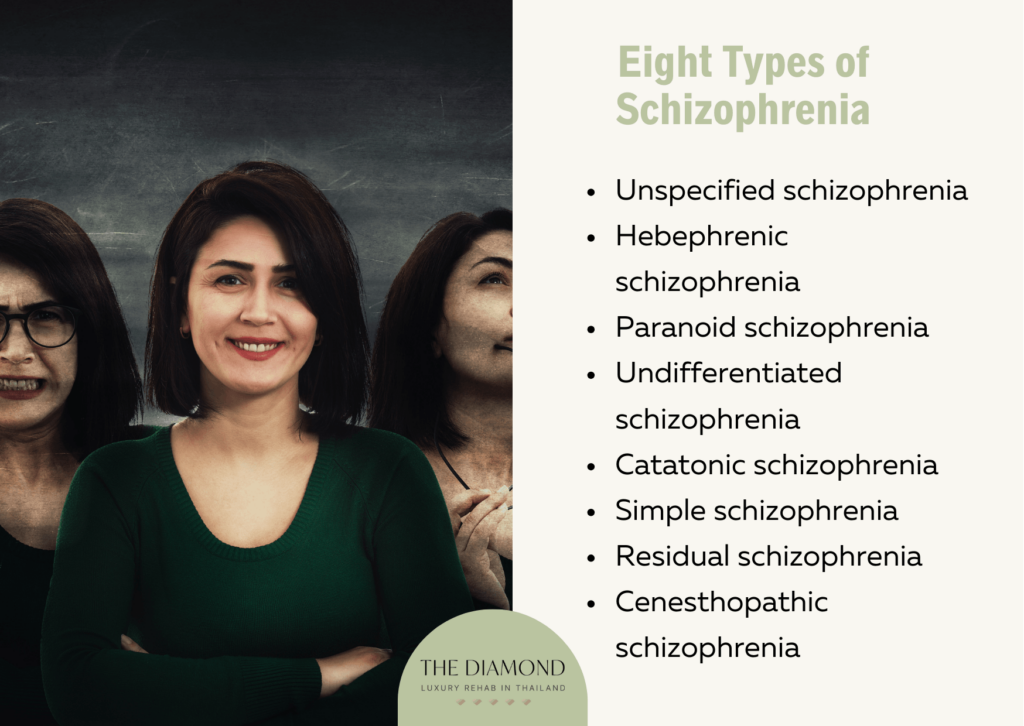
There are eight types of schizophrenia. They are listed below:
- Unspecified schizophrenia
- Hebephrenic schizophrenia
- Paranoid schizophrenia
- Undifferentiated schizophrenia
- Catatonic schizophrenia
- Simple schizophrenia
- Residual schizophrenia
- Cenesthopathic schizophrenia
1. Unspecified schizophrenia
Unspecified schizophrenia is a condition where a patient’s symptoms do not meet the full diagnostic criteria for schizophrenia or another more specific psychotic disorder. The other types of schizophrenias usually include a symptom that is more pronounced, and doctors are able to diagnose the problem. In some cases, a single subtype of schizophrenia can’t explain those symptoms because they overlap. That’s what happens in unspecified schizophrenia.
This type of schizophrenia may occur due to changes in brain structure and impaired levels of neurotransmitters in the brain. Other factors could also play a role, but a lot more research is necessary to determine what exactly causes unspecified schizophrenia.
Symptoms of unspecified schizophrenia include hallucinations, delusions, disorganized thinking, decreased emotional expression, impaired or disorganized speech, difficulty focusing, problems with decision-making, atypical movements, reduced motivation, and lack of interest.
People are more likely to develop unspecified schizophrenia if their close family members have it or if they have another mental health problem. Substance abuse, especially mind-altering drugs, is also a risk factor for unspecified schizophrenia.
The biggest effects of unspecified schizophrenia are a higher risk of developing anxiety disorders, including obsessive-compulsive disorder (OCD), suicidal thoughts and tendencies, and increased conflicts as well as difficulty keeping up at work or school.
The main course of treatment is a combination of psychotherapy and medications such as antipsychotics or benzodiazepines depending upon the symptoms. Addressing specific symptoms helps to stabilize the patient, improve communication, and clarify the diagnosis. Determining the accurate diagnosis is necessary for longer-term treatment.
2. Hebephrenic schizophrenia
Hebephrenic schizophrenia is a type of schizophrenia where the prominent symptoms are disorganization in speech, thoughts, or behaviors.
The causes of hebephrenic schizophrenia are not entirely known. The main theory is that the issue is in the function of the brain, but environmental and genetic factors could also play a role.
Symptoms of hebephrenic schizophrenia include hallucinations, delusions, abnormal behavior, negative symptoms, and disorganized thinking. A person with hebephrenic schizophrenia exhibits unusual speech patterns (disorganized speech), incongruent facial reactions, and emotions that don’t fit the situation, and they find it difficult to perform everyday tasks.
The risk factors behind hebephrenic schizophrenia include genetics, brain structure and chemistry, viral infection in the womb, maternal malnutrition, severe stress during early life, and the age of parents when the person was born. A study in the Scientific Reports journal states that a child born either to younger or older parents has a higher risk of developing schizophrenia than a person born to parents who were between 25 and 29 years old.
The main effect of hebephrenic schizophrenia is that disorganized thoughts and speech lead to disorganized behavior. As a result, it can be difficult for a person to perform properly at work or school. This may cause a chain of reactions that also include financial problems and greater susceptibility to developing some mental health disorders.
When it comes to the effects, it’s important to mention that patients with schizophrenia may have limited access to a nutritious or balanced diet and medical care.
Treatment goals are targeting symptoms, preventing relapse, and improving adaptive functioning in the community. For that purpose, a doctor may recommend psychotherapy such as cognitive-behavioral therapy, individual therapy, and group therapy. In addition to therapy, patients also receive a prescription for antipsychotic medications.
Assertive community treatment plays an important role in the management of hebephrenic schizophrenia and other types of this mental illness. Generally speaking, assertive community treatment is a multidisciplinary therapeutic team approach that can help reduce homelessness and hospitalization.
3. Paranoid schizophrenia
Paranoid schizophrenia is a type of schizophrenia where the prominent symptom is paranoia. The term paranoia describes a pattern of behavior where a person is distrustful and overly suspicious of other people and acts accordingly. Since their perception of reality is impaired, a person may feel that others are against them or even that someone wants to harm them.
It’s not clear what causes paranoid schizophrenia. Causes such as genetics, brain chemical imbalances, and congenital brain problems could be involved. A combination of different factors is usually the main culprit. Paranoia itself is not a disease or condition, it’s always accompanied by a serious mental health problem, such as schizophrenia in this case.
Symptoms of paranoid schizophrenia include hallucinations, delusions, incoherent or disorganized speech, disorganized behavior, and negative symptoms. These symptoms are accompanied by paranoia in people with this type of schizophrenia. People with this condition also have anosognosia (lack of insight) i.e., their brain can’t recognize any signs of medical problems they have. This explains why most people with paranoid schizophrenia don’t believe they have this mental illness and may resist their treatment.
Common risk factors for paranoid schizophrenia include personal mental health history, family history of schizophrenia, abusing mind-altering drugs, exposure to certain chemicals and substances, and certain age groups (from adolescence to early 30s).
Effects of paranoid schizophrenia include trouble keeping a job, financial problems, relationship issues with other people, marital problems, thoughts of suicide, anxiety, depression, and loneliness. Since the prominent feature of this mental illness is paranoia, a person’s excessive suspicion can cause significant problems with other people.
Treating paranoid schizophrenia usually revolves around multiple methods applied at the same time or one after the other. Common approaches are antipsychotic medications, psychotherapy, and self-management. The main purpose of therapy for patients with schizophrenia is to help them adapt to their condition more effectively. Self-management revolves around taking medications as prescribed, seeing a healthcare provider as recommended, avoiding alcohol and drugs, building relationships with people you trust, and going to therapy sessions regularly.
4. Undifferentiated schizophrenia
Undifferentiated schizophrenia is a type of this condition when a person meets the criteria for schizophrenia, but can’t be classified into other subtypes. Even though it’s no longer used in DSM, many healthcare providers still use this term. People with undifferentiated schizophrenia exhibit thoughts and behaviors of more than one type of this mental illness.
Researchers aren’t quite sure what causes undifferentiated schizophrenia. A combination of different causes is likely to lead to this psychiatric illness. These causes are similar for all types of schizophrenia and include genetics, changes in brain chemistry, substance abuse, and the environment.
Symptoms of undifferentiated schizophrenia can be positive, negative, and cognitive. They usually include hallucinations, delusion, thought disorder, paranoia, and catatonia. Sometimes one of these symptoms affects a person, but in other cases, they may overlap. When symptoms overlap and aren’t specific enough to meet the criteria for other subtypes of schizophrenia, the doctor may diagnose the condition as undifferentiated schizophrenia.
Common risk factors for undifferentiated schizophrenia include being in late adolescence or thirties, family history, substance use, and the environment. Types of environments that are linked to undifferentiated schizophrenia include poverty, stress, prenatal malnutrition, prenatal exposure to pathogens and viruses, and a history of abuse and neglect.
Effects of undifferentiated schizophrenia range from developing anxiety and depression to low productivity at work, difficulty communicating, and financial problems. People with undifferentiated schizophrenia are also more prone to alcohol and drug abuse.
Treatment options for undifferentiated schizophrenia include antipsychotic medications, family education and support, psychosocial treatment, and coordinated specialty care. Psychosocial treatment involves different types of therapy to reduce the cognitive and negative symptoms of this condition. Therapy also helps cope with everyday challenges. Patients usually attend cognitive-behavioral therapy sessions, but other therapies include behavioral skills training, supported employment, and cognitive remediation interventions.
On the flip side, the term coordinated special care describes a recovery-oriented treatment program where several health professionals help patients overcome their condition.
5. Catatonic schizophrenia
Catatonic schizophrenia is a type of schizophrenia whose main feature is catatonia. The term catatonia refers to cases when people react little or not at all to their environment or surroundings, or they may behave in ways that are unusual or unexpected. Catatonia has three main forms such as excited or hyperkinetic, withdrawn or hypokinetic, and mixed.
This type of schizophrenia includes extremely high levels of movement or no moving at all.
It’s not quite clear why catatonic schizophrenia happens. Potential causes include imbalances of chemicals in the brain, congenital brain problems, and disruption in communication between areas of the brain.
Symptoms of catatonic schizophrenia may include stupor, stereotypy, negativism, posturing, mutism, agitation, grimacing, echolalia (repetition of another person’s words), echopraxia (repetition of another person’s movements), and others. A person in a catatonic state may experience behaviors that are total opposites such as defiance and unexplained excitability.
The main risk factor for catatonic schizophrenia is family history, but a patient’s behavior and overall lifestyle also play a role. Substance abuse increases the risk of this condition.
The primary effects of catatonic schizophrenia are disconnection from reality and a lack of response to what’s happening. Sometimes people with catatonic schizophrenia aren’t aware of their surroundings. This can lead to a serious impact on a person’s quality of life, including their employees.
Although not curable, catatonic schizophrenia is treatable. The main treatment approaches are medication and therapy, especially cognitive-behavioral therapy. Some patients may also undergo electroconvulsive therapy, which sends a mild electrical current into a part of the brain to cause a brief seizure and changes in activity in the brain.
6. Simple schizophrenia
Simple schizophrenia is a type of schizophrenia whose development includes the erosion of affect and intelligence. This type of schizophrenia doesn’t function through positive symptoms involved in psychosis. Simple schizophrenia was also referred to as attenuated psychosis syndrome.
Causes of simple schizophrenia usually include heredity, imbalances of neurotransmitters in the brain, changes in brain structure, and substance abuse.
Symptoms of simple schizophrenia include alogia, social withdrawal, blunted affect, lack of interest or initiative, and functional impairment.
Factors that increase one’s risk of developing this condition include a family history of schizophrenia, personal history of mental health disorder, and using mind-altering substances.
Effects of simple schizophrenia may include anxiety, difficulty maintaining a job, homelessness due to unemployment, engaging in risky behaviors, social isolation, financial difficulties, and others.
Treatment of simple schizophrenia usually revolves around medications and therapy. The biggest objective of the treatment is to help patients manage their symptoms in order to have a better quality of life.
7. Residual schizophrenia
Residual schizophrenia is the third stage of schizophrenia. During this stage, a patient experiences fewer symptoms compared to the active stage. People with residual schizophrenia usually do not experience hallucinations, delusions, or disorganized speech or behavior. They mainly experience depression, low energy, and lack of motivation. A person was thought to have residual schizophrenia when they had at least one schizophrenic episode, but without positive symptoms.
The causes of residual schizophrenia are the same as those for schizophrenia in general. They may include a combination of genetics, impaired brain chemistry, mind-altering drug use, and the environment.
When it comes to the symptoms, positive symptoms are no longer present, as mentioned above. Instead, a patient may experience negative symptoms such as odd beliefs, distorted thinking, unusual perceptual experiences, diminished emotional expression, lack of motivation, reduced pleasure from positive stimuli, alogia or diminished speech, and becoming asocial.
Risk factors for residual schizophrenia include family history, exposure to toxic chemicals in the womb, malnutrition during pregnancy, and drug abuse.
Effects of residual schizophrenia tend to include impaired functioning in teams and society or difficulty establishing communication with others. This is mainly due to symptoms such as social isolation or difficulty communicating or having normal emotional responses.
Residual schizophrenia is treated primarily with antipsychotic medications and therapy, such as cognitive-behavioral therapy. For better quality of life, patients may also need psychosocial interventions such as behavioral skills training.
8. Cenesthopathic schizophrenia
Cenesthopathic schizophrenia is a type of schizophrenia indicated by bothersome or bizarre bodily sensations. These sensations are called cenesthopathy, a term that dates back to the early 20th century, and they usually occur without a physical cause. It’s important to mention that cenesthopathic schizophrenia has never been considered a specific subtype of schizophrenia in DSM mainly because the symptoms are present in other psychiatric disorders too.
This type of schizophrenia works by inducing aberrant sensations in a specific part of the body. People often use odd descriptions to describe these sensations and they are usually medically unexplainable.
The precise cause of cenesthopathic schizophrenia is unclear. One theory suggests that cenesthopathy is an extension of body image disturbance. That could explain why a person with schizophrenia may experience distortion about the anatomical size, function, or shape of the body. A patient with schizophrenia may depersonalize their body and thereby objectify the image they see in the mirror. This could lead to body dysmorphia, body boundaries (sense of shape is influenced by the perception of embodied state), and morbid identification (considering body parts as lifeless).
The symptoms of cenesthopathic schizophrenia are subjective and vary from one person to another. Two people can experience these unusual sensations in different parts of the body. That being said, most people experience symptoms of “moving” sensations such as cold flowing through the body, feeling as if the part of the body is detached or compressed, and feeling as if the brain is softening or hardening. Other symptoms include feeling as if a part of the body is hollow or exposed to the air and feeling the presence of nodules of foreign bodies inside the body.
The risk factors for this type of schizophrenia include a family history of schizophrenia, taking mind-altering drugs, dental treatment in the acute phase of depression, and other mental health disorders.
Effects of cenesthopathic schizophrenia include worsening of mental health problems and body image or perception of one’s body.
There is no specific treatment for this type of schizophrenia. The doctor may prescribe medications such as antipsychotics in combination with psychotherapy. The goal of the treatment is to help patients cope with schizophrenia in order to achieve and maintain remission.
What is Schizophrenia?
Schizophrenia is a mental disorder that affects a person’s perception of reality and interferes with their ability to think clearly, make decisions, manage emotions, and relate to others. The American Psychiatric Association’s Diagnostic and Statistical Manual of Mental Disorders, fifth edition (DSM-5) classifies schizophrenia as a mental illness in the chapter Schizophrenia Spectrum and other Psychotic Disorders.
According to the World Health Organization (WHO), schizophrenia affects 24 million people in the world. More precisely, the illness affects one in 300 people or 0.32% of the worldwide population. Schizophrenia isn’t as common as other mental health disorders. People usually develop schizophrenia in late adolescence and their twenties. Men are more likely to have an earlier onset of schizophrenia than women.
The term schizophrenia is about 100 years old; it was first used in 1911 by a Swiss psychiatrist Eugen Bleuler. The word schizophrenia comes from the Greek word schizo (split) and phrene (mind). Bleuler used the term to put an emphasis on mental confusion and fragmented thinking.
It’s important to mention that schizophrenia isn’t the same as multiple personality disorder (now called dissociative identity disorder). The latter includes separate identities and personalities that a person creates whereas a patient with schizophrenia experiences hallucinations, paranoia, and delusion. A person with schizophrenia doesn’t have multiple personalities.
Symptoms of schizophrenia vary but usually include hallucinations, delusions, disorganized speech, abnormal motor behavior, and negative symptoms such as lethargy, impaired emotional processing, social withdrawal, and loss of interest.
The exact cause of schizophrenia is unknown, but a combination of brain chemistry, genetics, and the environment contribute to its development. Mayo Clinic reports that some people with schizophrenia may have problems with certain neurotransmitters such as glutamate and dopamine. They also have differences in brain structure and central nervous system.
Although any individual can develop schizophrenia, some people are at a higher risk than others. Common risk factors include a family history of schizophrenia, pregnancy and birth complications, and taking mind-altering drugs.
Schizophrenia has a multitude of effects on a person’s life. The most common effects include anxiety, depression, substance use disorders, being victimized, health and medical problems, aggressive behavior, homelessness, financial problems, inability to work or attend school, and suicidal thoughts and tendencies.
What is the most common type of Schizophrenia?
The most common type of schizophrenia is paranoid schizophrenia. The exact statistics regarding the prevalence of paranoid schizophrenia are scarce. One of the older studies on this subject reported that the incidence of paranoid schizophrenia is 0.17 per 10,000 of the population. Around 40.8% of all cases of schizophrenia account for the paranoid type, as reported in a paper in International Islamic Medical Journal.
It’s unclear why paranoid schizophrenia is the most common type of this severe mental illness. The potential theory is that paranoid schizophrenia mainly includes typical symptoms that we associate with this condition such as hallucinations, delusions, paranoia, and others. Since most people with schizophrenia exhibit these symptoms and behaviors, it could explain why it’s more common than other types.
How to determine different types of Schizophrenia?
Different types of schizophrenia are determined based on the symptoms that patients experience and their moods and behaviors.
It’s important to mention, however, that DSM-5 doesn’t use types of schizophrenia. More precisely, the criteria for diagnosis of schizophrenia still contain symptoms such as paranoia, hallucinations, and delusions. But these symptoms aren’t considered different subtypes of this mental illness.
The main reason for this change is that some symptoms overlapped across different types of schizophrenia. But, if a patient experiences catatonia, they may be diagnosed with schizophrenia with catatonia.
How is Schizophrenia diagnosed?
Schizophrenia is diagnosed after a physical exam and psychiatric evaluation. The main purpose of a physical exam is to rule out health problems that may cause symptoms similar to those of schizophrenia. The doctor may recommend tests and screenings such as a CT scan or an MRI.
Based on the symptoms described by a patient or their family members, the doctor also recommends psychiatric evaluation. The psychiatrist evaluates a patient’s mental health by observing their demeanor and appearance. During the psychiatric evaluation, the patient answers questions regarding their moods, thoughts, hallucinations, and delusions. Questions about substance abuse and suicidal thoughts and tendencies are also included. For a complete psychiatric evaluation, the mental health professional discusses family and personal history.
The psychiatrist gathers all necessary information and checks whether the patient’s symptoms meet the diagnostic criteria for schizophrenia. For that purpose, the psychiatrist uses DSM-5.
Schizophrenia is usually diagnosed if a patient has experienced one or more symptoms most times of the month, especially if they have a significant impact on a person’s life and can’t be explained by other potential causes. These symptoms usually include hallucinations, delusions, incoherent speech, hearing voices, and negative symptoms like flattening emotions.
What does Type 1 schizophrenia mean?
Type 1 schizophrenia means a person experiences prominently positive symptoms of this mental illness. The term positive symptom refers to behavior or thinking a person with schizophrenia didn’t have before developing this mental health condition. These symptoms are being added to a person’s psyche. Positive symptoms of schizophrenia are hallucinations, delusions, paranoia, and hearing voices.
What does Type 2 schizophrenia mean?
Type 2 schizophrenia means a person has mainly negative symptoms. Negative symptoms are thoughts and behaviors that a person had before becoming ill but don’t have anymore or they are present to a lesser extent. In other words, these are normal thoughts or behaviors that have become lost or taken out of a person’s psyche.
Good examples of negative symptoms are losing interest and motivation in life and activities, changes in sleep patterns, social isolation, lack of concentration, absent emotional responses, speech reduction, anhedonia (inability to experience pleasure), sexual problems, and lethargy.
What is the highest type of Schizophrenia?
The highest type of schizophrenia is paranoid schizophrenia, also the most common type of this mental illness. What makes paranoid schizophrenia the highest, or most severe, form of schizophrenia is that patients are unable to control or understand what reality is and what are hallucinations or delusions. At the same time, paranoid delusions make people feel threatened and angry. This explains why people with this type of schizophrenia are often perceived as dangerous and unpredictable, even though they aren’t usually violent.
What is the lowest type of Schizophrenia?
The lowest type of schizophrenia is residual schizophrenia, mainly because it is not cyclical. It can disappear and reappear at any time. As the lowest, and the least severe, type of schizophrenia, residual schizophrenia still causes symptoms. However, the symptoms aren’t as disordered or severe as in other types of this mental illness. It’s particularly important to mention residual schizophrenia doesn’t have positive symptoms like hallucinations and delusions. Instead, patients usually have negative symptoms.
Is Schizophrenia caused by trauma?
Yes, trauma may be a contributing factor to schizophrenia, but the jury is still out there on whether it causes this mental health disorder. Experiencing trauma, particularly in childhood, could raise the likelihood of psychotic symptoms and schizophrenia development.
Changes in the nervous system and brain may occur as a consequence of trauma. It can also cause oxidative stress, which leads to inflammation and difficulty controlling emotional responses. As a result, the affected individual is more susceptible to mental health problems including schizophrenia.
In a paper from the Frontiers in Neuroscience, childhood trauma is linked to impaired working memory, verbal learning, attention, and executive function in schizophrenia. However, scientists report a lot more research is necessary to establish whether trauma on its own can cause schizophrenia.
Besides childhood trauma, schizophrenia is also linked to PTSD. Post-traumatic stress syndrome develops after exposure to a traumatic experience. A review from Neuropsychiatry found that symptoms of PTSD may overlap with schizophrenia symptoms. Both conditions have common symptoms such as hallucinations, social isolation, and dissociative symptoms. The same review also explained PTSD is more prevalent in people with schizophrenia than in the general population.
To sum up, trauma is more of a risk factor or contributor to schizophrenia rather than a specific cause.
