Hypnotic addiction: symptoms, causes, effects, and treatment

Hypnotic addiction is a substance use disorder marked by the uncontrollable and compulsive use of hypnotic drugs despite their adverse medical and psychosocial outcomes. The disorder is typically associated with the abuse of prescription medications for treating insomnia.
The symptoms of hypnotic addiction include impaired control over drug use; inability to quit; cravings; persistent usage despite negative health issues and social problems; recurrent use in physically dangerous situations; tolerance; and dependence. An individual spends increasing amounts of time on drug-related activities, neglects responsibilities, and reduces meaningful activities to engage in drug use.
The causes of hypnotic addiction are misusing prescription drugs; self-medicating; developing tolerance; becoming dependent; and manifesting withdrawal upon stoppage.
The effects of hypnotic addiction are cognitive decline, psychomotor impairment, respiratory depression, ataxia, magnification of sleep apnea symptoms, daytime sleepiness, reduced daytime performance, increased risk of falls and accidents, reduced quality of life, increased risk of overdosing, and greater mortality.
The treatments for hypnotic addiction are detoxification, inpatient care, outpatient care, psychotherapy, and aftercare.
What is hypnotic addiction?
Hypnotic addiction is a substance use disorder characterized by a problematic pattern of behaviors and functional impairments associated with the use of hypnotic drugs. The distinguishing features of the disorder are the compulsive use of hypnotics despite significant adverse medical, psychological, and social outcomes caused by these substances and the development of tolerance to and cravings for the drugs.
Hypnotic addiction typically involves the use of prescription sleep medications. The disorder is diagnosed under the broader category of Sedative-, Hypnotic-, or Anxiolytic-Related Disorders, according to the classification by the Diagnostic and Statistical Manual of Mental Disorders, fifth edition.
What are hypnotic drugs?
Hypnotic drugs are medications that reduce the activity of the central nervous system (CNS) by targeting the inhibitory neurotransmitter GABA (gamma-aminobutyric acid) and thereby, promoting sleep, according to the definition provided by authors Sophie G. Carter and Danny J. Eckert in the 2021 article titled “Effects of hypnotics on obstructive sleep apnea endotypes and severity: Novel insights into pathophysiology and treatment” published in the journal Sleep Medicine Reviews. These drugs are usually prescribed for treating insomnia and sleep disturbances, such as those linked to air travel.
Hypnotics are a large group of drugs consisting of benzodiazepines and non-benzodiazepines. Barbiturates are an older class of hypnotics. Specific types of hypnotics like benzodiazepines are federally controlled substances.
What are some examples of hypnotic drugs?
The examples of some hypnotic drugs are listed below.
- Benzodiazepines: Benzos are prescribed as short-duration treatment for insomnia. They are available in short- and long-acting formulations and are effective in reducing the time needed to fall asleep, lengthening sleep duration, and reducing wakefulness during sleep. Common examples of benzodiazepines are diazepam (Valium®), alprazolam (Xanax®), lorazepam (Ativan®), clonazepam (Klonopin®), estazolam (ProSom®), flurazepam (Dalmane®), temazepam (Restoril®), and triazolam (Halcion®).
- Non-benzodiazepines: These medications are also referred to as “Z-drugs” and were developed to overcome the disadvantages of benzodiazepines, such as high dependence potential and hangover effects, according to a 2016 article by Seema Varma published in the journal Medicine, titled “Benzodiazepines and hypnotics.” Common examples of non-benzodiazepines are zopiclone (Imovane®, Zimovane®, etc), zolpidem (Ambien®), eszopiclone (Lunesta®), and zaleplon (Sonata®).
- Barbiturates: Barbiturates are an older class of hypnotics that have been largely replaced by benzodiazepines to overcome disadvantages like hangovers associated with the former. They also possess a less favorable safety profile than benzos. However, barbiturates are still used as anesthetics and to treat epilepsy. Common examples of barbiturates are phenobarbitone, barbitone, butobarbitone, amylobarbitone, and pentobarbitone.
- Melatonin receptor agonists: Melatonin, a substance secreted by the pineal gland, is responsible for maintaining the circadian rhythms and regulating the sleep/wake cycle. Melatonin receptor agonists work by activating melatonin receptors to promote sleep. They are used for treating insomnia; sleep disturbances linked to jet lag, shift work, depression, and tapering off from hypnotics; and circadian disorders in older adults and the blind. Examples of these drugs include ramelteon and tasimelteon.
- First-generation antihistamines: First-generation antihistamines are widely used for their sleep-inducing properties. These drugs include diphenhydramine, doxylamine, doxepin, chlorpheniramine, hydroxyzine, meclizine, promethazine, and cyproheptadine, as mentioned in the chapter titled “Clinical Pharmacology of Other Drugs Used as Hypnotics” by Buysse et al., in the book Principles and Practice of Sleep Medicine (Fourth Edition) published in 2005.
- Antidepressants: Antidepressants like trazodone have sleep-inducing properties. Trazodone is one of the most prescribed, though off-label, treatments for chronic insomnia.
- Orexin antagonists: Orexin is a neurotransmitter that promotes wakefulness. Orexin antagonists promote sleep by blocking the action of orexin receptors. Dual orexin receptor antagonist (DORA) drugs have been approved by the U.S. Food and Drug Administration for treating chronic insomnia and helping patients fall and remain asleep.
- Miscellaneous hypnotics: Melatonin oral supplements are used as short-term treatment options for insomnia associated with jet lag and sleep cycle disorders. These supplements are believed to help patients fall asleep quicker, reduce wakefulness during sleep, and increase sleep duration. Valerian is a botanical agent that has hypnotic properties and has been found to improve sleep quality, decrease the time needed to fall asleep, and reduce awakenings during sleep, as mentioned in the chapter titled “Clinical Pharmacology of Other Drugs Used as Hypnotics” by Daniel J. Buysse and Shachi Tyagi in the book Principles and Practice of Sleep Medicine (Sixth Edition) published in 2017.
What is the difference between hypnotics and sedatives?
The differences between hypnotics and sedatives stem from the intent of their usage and the effects they produce on the human body. Hypnotics induce drowsiness and promote the onset and maintenance of a state of sleep that is similar to natural sleep. These drugs are thus prescribed to treat sleep disorders. On the other hand, sedatives induce a state of calmness and relaxation by reducing tension and anxiety. They do not induce sleepiness but make it possible for an individual to fall asleep.
Both hypnotics and sedatives reduce the activity of the CNS. So, the same drugs are able to produce sedating and hypnotic effects depending on the medication prescribed and their dosage. For instance, specific benzodiazepine formulations have both hypnotic and sedating properties. These drugs are known to cause physiological dependence, especially in long-term users, which is a potent risk factor for developing hypnotic use disorder and sedative addiction.
What is the difference between hypnotics and anxiolytics?
The differences between hypnotics and anxiolytics arise from their intended use and effects on the body. Hypnotics are a class of drugs that induce sleepiness and help an individual fall and remain asleep. They are prescribed for treating insomnia. Anxiolytics, on the other hand, are a class of medicines that reduce emotional anxiety and tension and are used for treating generalized anxiety and panic disorders.
Both hypnotics and anxiolytics work by slowing down the activity of the brain. Like hypnotics, anxiolytics too have the potential to cause dependency. Both drugs are habit-forming and so, are prescribed for a short duration to prevent hypnotic use disorder and anxiolytic addiction.
Why are hypnotic drugs addictive?
Hypnotic drugs are addictive because they disrupt the way the brain’s reward circuitry works. The reward system of the brain is programmed to reinforce rewarding activities, such as those performed to survive. When individuals engage in such an activity–eating, for example–the reward system releases dopamine that produces a feeling of euphoria. This motivates the individual to repeat the activity in the future.
The calming and sleep-inducing effects of hypnotic drugs are pleasurable and rewarding for their users. In response to drug use, the reward pathways trigger a dopamine surge that over-stimulates the system. There is a strong reinforcement effect that motivates future drug use. Tolerance develops with repeated drug use. Additionally, hypnotic drugs are habit-forming and have a high potential for dependency. These properties contribute to sustained and compulsive drug use undertaken to experience euphoria-inducing effects and avoid the distress of withdrawal.
How common is hypnotic addiction?
Hypnotic addiction is common among individuals who tend to use prescription medications for non-medical purposes. Of the 707 inpatients and outpatients in a study who were prescribed benzodiazepines to treat insomnia, 32.4% exhibited a preoccupation with drug availability, 29% did not adhere to their prescribed dosage, and 32.4% showed problematic drug use, according to a 2020 article by Yamamoto et al., published in the journal Neuropsychopharmacology Reports, titled “Current state of hypnotic use disorders: Results of a survey using the Japanese version of Benzodiazepine Dependence Self‐Report Questionnaire.” Of these 707 patients, 324 had stopped using the drug or tapered off from it voluntarily. Among them, 10.8% exhibited severe withdrawal symptoms and 30.9% manifested severe withdrawal insomnia.
Data from a nationwide population register in Germany reveals that 14.8% of hypnotic drug users misuse the drug and 15.3% of users are dependent on it, according to a 2015 article by Janhsen et al., published in the journal Deutsches Ärzteblatt International, titled “The Problems of Long-Term Treatment With Benzodiazepines and Related Substances: Prescribing Practice, Epidemiology, and the Treatment of Withdrawal.”
What are the symptoms of hypnotic addiction?
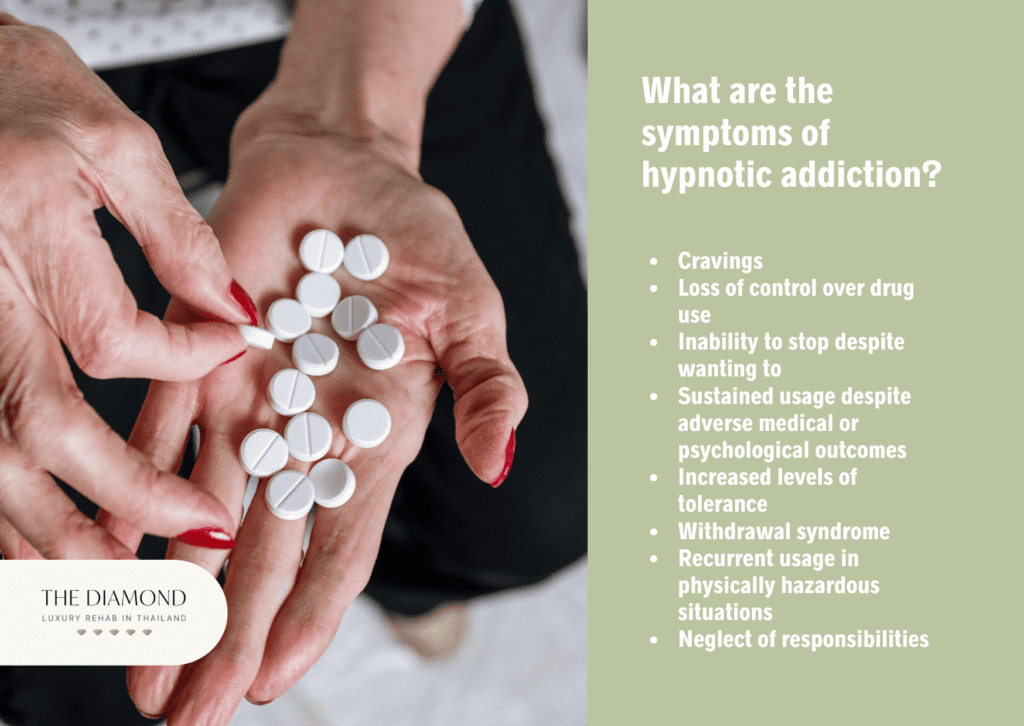
The symptoms of hypnotic addiction are listed below.
- Cravings: Craving is a core feature of addiction. It is a powerful desire for the psychoactive effects of hypnotics that the individual had previously experienced and is quickly magnified in the presence of internal and/or external triggers and the perceived availability of drugs. Cravings are believed to predict relapse and are known to contribute to the maintenance of addiction.
- Loss of control over drug use: Impaired control over the use of hypnotics manifests in one or more of the following ways: using more of the drug than intended or prescribed originally; using it for longer than intended or medically advised; and being unable to keep track of the amount consumed.
- Inability to stop despite wanting to: An individual with hypnotic addiction is unable to quit using the substance despite a persistent desire to do so or after multiple unsuccessful attempts.
- Sustained usage despite adverse medical or psychological outcomes: Individuals with hypnotic addiction continue using the substance despite knowing about the adverse medical and psychiatric issues that their addiction is causing or aggravating.
- Increased levels of tolerance: Increased tolerance indicates problematic substance use. In individuals with hypnotic addiction, it is marked by needing more of the drug to experience the earlier level of “high” or feeling the effects of the drug less even at the same dose.
- Withdrawal syndrome: The manifestation of withdrawal syndrome indicates dependence on a substance. Hypnotic withdrawal symptoms are distressful, and the motivation to avoid going through the discomfort of withdrawal compels individuals to continue abusing the substance.
- Recurrent usage in physically hazardous situations: Individuals persist in using hypnotic drugs in physical situations where it is hazardous to do so, such as when driving a vehicle or operating heavy machinery.
- Increased amounts of time and effort spent on drug-related activities: Individuals with hypnotic addiction are likely to spend increasing amounts of time and effort procuring, consuming, and recovering from the effects of the drug. For instance, doctor shopping is a common behavior among prescription drug abusers who consult multiple treatment providers to obtain prescription medications illegally.
- Disregard of important activities because of drug use: There is a tendency to give up or reduce participation in meaningful social, occupational, and/or recreational activities because of drug use.
- Neglect of responsibilities: Individuals tend to neglect their responsibilities at work, home, or school, which manifests as declining grades, being persistently late to work, and poor performance reviews.
- Sustained usage despite social and interpersonal problems: Individuals continue to use hypnotic drugs despite being aware that their substance use is persistently causing or aggravating interpersonal or social problems. For instance, relationship distress or dissatisfaction results when substance-using individuals neglect to carry out their familial duties or spend increasing amounts of time on drug-related activities instead of being with their loved ones.
What are the causes of hypnotic addiction?

The causes of hypnotic addiction are listed below.
- Misuse: CNS depressants like hypnotics are one of the most commonly misused prescription drugs, as noted by the National Institute on Drug Abuse (NIDA) in their October 2011 publication titled “Misuse of Prescription Drugs Research Report: Overview.” The misuse takes one or more of the following forms: using a hypnotic drug in more amounts or for longer than what was originally prescribed; using the drug for a non-medical purpose, such as to get a “high;” using it in a way than what is recommended, such as crushing a tablet and snorting it; and using sleep medications prescribed to another individual.
- Self-medication: Self-medication is the act of using a substance like hypnotics without consulting a doctor, usually in an attempt to chemically cope with emotional stress or pain or manage the symptoms of a mental health problem. It is widely held that self-medication contributes to the development of addiction.
- Developing tolerance: Becoming tolerant to the effects of a hypnotic entails that the individual is compelled to take higher amounts of the substance to achieve the earlier level of “high.” With sustained use of the drug, tolerance is likely to progress to dependence.
- Development of dependence: Developing dependence on a hypnotic drug is one of the most potent causes of addiction. Psychological dependence is associated with feelings of pleasure and a strong desire to use drugs to feel pleasure or avoid pain. Physical dependence refers to the physiological state where the body becomes accustomed to the presence of a substance and experiences unpleasant effects when usage is stopped.
- Manifestation of withdrawal symptoms: Withdrawal indicates physical dependence on a substance and manifests as a cluster of uncomfortable symptoms when drug use is stopped or reduced. Attempting to avoid the discomfort of withdrawal compels individuals to continue abusing a substance.
What are the risk factors for hypnotic addiction?
The risk factors for hypnotic addiction are listed below.
- Prolonged or heavy use: A majority of hypnotic drugs lose their efficacy after prolonged use, possibly due to the development of tolerance, which increases the risk of the individual taking more of the drug.Using these drugs for longer than a month and/or taking them in high doses are associated with an increased risk of developing dependence.
- History and/or presence of a substance use disorder (SUD): Individuals with a history of SUD have an increased risk of abusing sleep medications, according to a 2015 article by Michael F. Weaver published in the Yale Journal of Biology and Medicine, titled “Prescription Sedative Misuse and Abuse.” Individuals with existing substance use disorders are known to abuse sleep medicines, for instance, to magnify the “rush” of opioids or to reduce the withdrawal symptoms associated with cocaine.
- Age: Adults older than 64 years have an increased risk of developing dependence on medications prescribed for insomnia (Weaver, 2015).
- Genetic vulnerability: Individuals with a family history of alcohol use disorder are believed to be genetically vulnerable to developing benzodiazepine dependence.
- Presence of a mental disorder: The presence of a mental illness is one of the significant risk factors for addiction to sleep medications (Weaver, 2015).
- Emotional stress: Hypnotic agents like benzodiazepines are effective in treating symptoms of anxiety. It is probable that individuals who have been prescribed benzodiazepines for insomnia abuse the drug to achieve a euphoric feeling that numbs their emotional stress or pain.
- Non-recreational prescription medication sharing: This refers to the practice of lending or borrowing prescription medicines where the user is an individual other than the one for whom the medications were originally prescribed. For instance, an individual shares their unused hypnotic drugs with a family member with similar sleep problems so that the latter does not have to incur the cost of visiting a physician or buying the drug. This practice is risky because no patient-specific counseling or dosage instructions from the physician are available to the final user.
- Easy access: Hypnotic agents like benzodiazepines are safer than barbiturates because of a higher therapeutic index ratio and flatter dose-response curves. They are thus less stringently controlled and more widely prescribed, making them more likely to be abused.
What are the effects of hypnotic addiction?
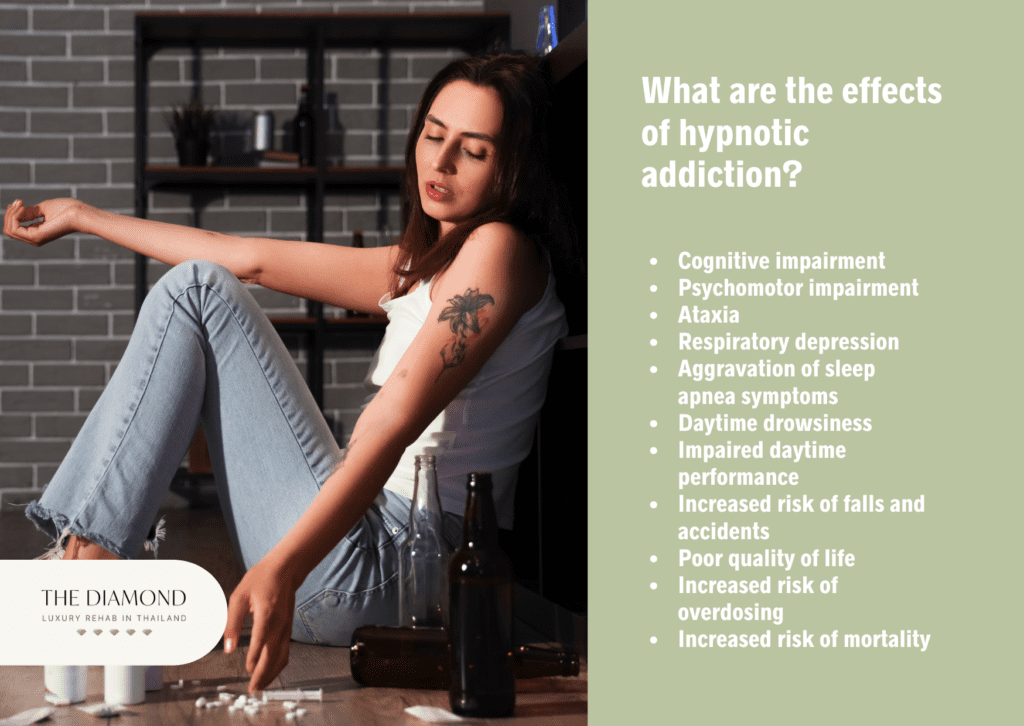
The effects of hypnotic addiction are listed below.
- Cognitive impairment: Cognitive decline manifests as impaired judgment and poor memory. Benzodiazepines are known to cause anterograde amnesia, a condition that diminishes an individual’s ability to learn new information.
- Psychomotor impairment: Chronic hypnotic use is associated with impaired motor skills, according to a 2014 article by Chelsie B. Heesch published in the journal Mental Health Clinician, titled “The long-term use of sedative hypnotics in chronic insomnia.” This is more so in the case of benzodiazepines than non-benzodiazepine drugs. Diminished motor abilities reduce dexterity and make it difficult and dangerous for the individual to drive a vehicle and operate machinery. Decreased reflexes are also associated with the chronic use of benzodiazepines.
- Ataxia: Ataxia is characterized by loss of balance, coordination, and speech. Chronic benzo use increases the likelihood of an individual developing ataxia that manifests as slurred speech, unsteady gait, and difficulty walking.
- Respiratory depression: Taking high doses of hypnotics like barbiturates is associated with respiratory distress and even coma due to the steep dose-response curve of these substances. However, a majority of cases involving respiratory distress or coma are caused when individuals mix hypnotics with other CNS depressants.
- Aggravation of sleep apnea symptoms: In a percentage of users, chronic hypnotic use is associated with an aggravation of sleep apnea symptoms. Sleep apnea is likely to lead to chronic hypertension and cardiac ischemia.
- Daytime drowsiness: Hypnotics like benzodiazepines are associated with increased next-day sedation. Non-benzodiazepine hypnotic drugs have less likelihood of causing excessive daytime sleepiness (Heesch, 2014).
- Impaired daytime performance: Excessive next-day sleepiness, impaired motor skills, and reduced cognitive efficiency possibly contribute to impaired daytime performance. Persistent hypnotics like flurazepam and quazepam significantly impact daytime performance and the negative effects magnify with continuous daily use.
- Increased risk of falls and accidents: There is overwhelming evidence to support the view that chronic hypnotic use increases the risks of falls and vehicle accidents, according to a 2000 article by Daniel F. Kripke published in the journal Sleep Medicine Reviews, titled “Chronic hypnotic use: deadly risks, doubtful benefit: REVIEW ARTICLE.” It is possible that next-day sedation, compromised psychomotor skills, decreased reflexes, ataxia, and/or impaired judgment cause these incidents.
- Poor quality of life: Increased morbidity caused by the medical effects of chronic hypnotic use, possible impairments caused by falls and/or accidents, decreased daytime performance that increases the likelihood of poor workplace performance, and worsening interpersonal and social relationships contribute to poor quality of life in individuals with hypnotic addiction.
- Increased risk of overdosing: The risk of overdosing on hypnotics like benzodiazepines is greater when the drug is mixed with other CNS depressants like alcohol and opioids and in the elderly who have diminished drug clearance or are on multiple medications that possibly cause adverse drug-drug interactions.
- Increased risk of mortality: Large-scale studies have shown that chronic hypnotic use, especially using it 30 times a month, is associated with an increased risk of premature death (Kripke, 2000).
What are the treatments for hypnotic addiction?
The treatments for hypnotic addiction are listed below.
- Detoxification: Hypnotic withdrawal symptoms are distressful and potentially life-threatening for vulnerable patients. So, it is recommended that detoxification from hypnotics is carried out under medical supervision to ensure patient safety and ease the transition to the next level of treatment. This process typically involves a gradual tapering off from the drug being abused to prevent the development of severe symptoms like delirium tremens and seizures. In cases where the patient is unable to cope with mild withdrawal symptoms, a hypnotic with a long half-life is administered to reduce the severity of symptoms during the tapering-off process.
- Inpatient care: Patients with hypnotic addiction admitted to an inpatient drug rehab receive 24-hour medical monitoring and intensive medical care. This level of care is recommended for individuals with severe addiction, co-occurring psychiatric disorders, and complex medical conditions that are likely to make withdrawal challenging.
- Outpatient care: A majority of patients with hypnotic addiction are stable and require minimal medical management. They are thus, typically treated in an outpatient setting.It has been found that detoxification of patients with hypnotic addiction is safe to be carried out at an outpatient facility if appropriate patient selection and management practices are followed. Outpatient centers deliver addiction treatment at varying levels of intensity depending on the medical and psychological needs of the patient and their convenience. These facilities offer specialized support to treat complex medical and psychiatric problems; one-on-one, group, and family psychotherapy sessions to promote behavioral modifications; educational sessions to impart instructions on relapse prevention; and occupational or recreational therapy.
- Psychotherapy: It has been found that cognitive behavioral therapy (CBT) brings about a reduction in hypnotic use and an improvement in sleep quality when delivered alongside medically managed withdrawal in older adults with hypnotic dependence and insomnia, according to a 2013 article by Lichstein et al., published in the journal Behaviour Research and Therapy, titled “Psychological Treatment of Hypnotic-Dependent Insomnia in a Primarily Older Adult Sample.”
- Aftercare: Taking part in aftercare services after completing formal treatment and/or psychotherapy ensures sustained sobriety and prevents a relapse. Staying in sober living houses, undergoing individual counseling, and becoming a member of addiction recovery support groups, such as Pills Anonymous that is modeled on the 12-Step program, are some addiction aftercare recovery strategies that help patients build on the benefits reaped from their stint in formal drug rehab.
How can you overcome hypnotic addiction?
You can overcome hypnotic addiction by undergoing treatment that is grounded in evidence-based methodologies. Do not try to quit drugs on your own because withdrawal symptoms are not only distressful but also potentially life-threatening. Seek the help of a therapist or a counselor if you have a mental health issue that compels you to misuse hypnotic drugs. Learn about alternate ways, such as aromatherapy, to improve sleep quality so that you are able to reduce your dependence on hypnotics. Practice good sleep hygiene, exercise regularly, and eat a healthy diet. Practice relaxation techniques like yoga and mindfulness meditation to bring on a state of calmness that is conducive to sleep.
What are the symptoms of hypnotic addiction withdrawal?
The symptoms of hypnotic addiction withdrawal are listed below.
- Insomnia: Rebound insomnia after discontinuing hypnotic use is characterized by worsened quality of sleep and reduced daytime well-being. It has been found that this symptom tends to persist in sections of individuals but varies significantly from one night to another. Rebound insomnia is typically associated with hypnotics with shorter half-lives.
- Anxiety and depression: Anxiety is likely a rebound symptom of hypnotic withdrawal. Specific patient populations also manifest depressive symptoms during hypnotic withdrawal. In individuals with a co-occurring depressive disorder, these symptoms are exaggerated. However, it has also been found that patients with no history of a depressive disorder manifest depressive symptoms during hypnotic withdrawal, according to a 1994 article by Malcolm Lader published in the Journal of Psychosomatic Research, titled “Anxiety or depression during withdrawal of hypnotic treatments.”
- Autonomic hyperactivity: Autonomic hyperactivity is a cardinal symptom of hypnotic drug withdrawal and presents as a cluster of signs like a pulse rate greater than 100, elevated blood pressure, high body temperature, and profuse sweating.
- Nausea and vomiting: Nausea and vomiting are common symptoms of drug withdrawal. They are uncomfortable but not life-threatening.
- Psychomotor agitation: Psychomotor agitation is a cardinal symptom of hypnotic withdrawal and manifests as symptoms that include muscle tension, sudden and inexplicable movements, and restlessness. Patients experiencing hypnotic withdrawal also exhibit hand tremors.
- Hallucinations: Hallucinations are a serious symptom of hypnotic withdrawal. However, visual, auditory, or tactile hallucinations are typically associated with the manifestation of delirium.
- Delirium: Delirium is a severe symptom of hypnotic withdrawal and is fatal, if not treated immediately and aggressively. It must be noted that delirium associated with hypnotic withdrawal also manifests in the absence of the cardinal symptoms of withdrawal.
- Grand mal seizures: Grand mal seizures are severe symptoms that occur in 20-30% of patients who undergo hypnotic withdrawal without medical supervision.


