Conduct disorder (CD)
Table of content
- What is Conduct disorder?
- What are the categories of Conduct disorder (CD)?
- What are the symptoms of Conduct disorder?
- What are the causes of Conduct disorder?
- What are the risk factors for Conduct disorder?
- How is Conduct disorder (CD) diagnosed?
- When does Conduct disorder (CD) begin?
- What is the prevalence of Conduct disorder (CD)?
- Which children are at risk for Conduct disorder (CD)?
- What is the treatment for Conduct disorder (CD) in children?

Conduct disorder (CD) is a disorder indicated by aggressive, violent, destructive, and deceptive behaviors. The condition is diagnosed primarily in children and adolescents. Patients with (CD) don’t feel guilt or remorse for their actions. There are several types of CD such as childhood-onset, adolescence onset, and unknown onset conduct disorder.
Conduct disorder symptoms involve hurting people and animals, theft, lack of emotions, and destroying something intentionally, among others. Sometimes patients with CD can express emotions with the sole purpose to manipulate others.
Pinpointing a specific cause of CD would be difficult. The condition can be caused by biological, social, cognitive, or genetic factors. Boys are at a higher risk of conduct disorder than girls. Growing up in a dysfunctional home and family history of CD, substance abuse, and other mental health disorders increases the risk of conduct disorder.
Effects of conduct disorder range from problems at school or work to legal problems and substance abuse.
Fortunately, conduct disorder is treatable. The cornerstone of treatment is psychotherapy, but the doctors may prescribe medications to manage other problems such as ADHD.
What is Conduct disorder?
Conduct disorder is a type of behavior disorder characterized by emotional and behavioral problems in children and adolescents. Patients with conduct disorder experience difficulties following the rules and they behave in a socially unacceptable manner.
The origins of conduct disorders lie within the social and legal problem of delinquency back in 1880. Over the following decades, there was increased research on the conduct problems of children and teenagers. In 1968, conduct disorder became an established medical diagnosis.
However, it will take a few decades for conduct disorder definition to appear in the American Psychiatric Association’s Diagnostic and Statistical Manual of Mental Disorders. More precisely, the disorder appeared for the first time in the fourth edition i.e. DSM-4 in 1994. The condition is also present in DSM-5.
What are the categories of Conduct disorder (CD)?
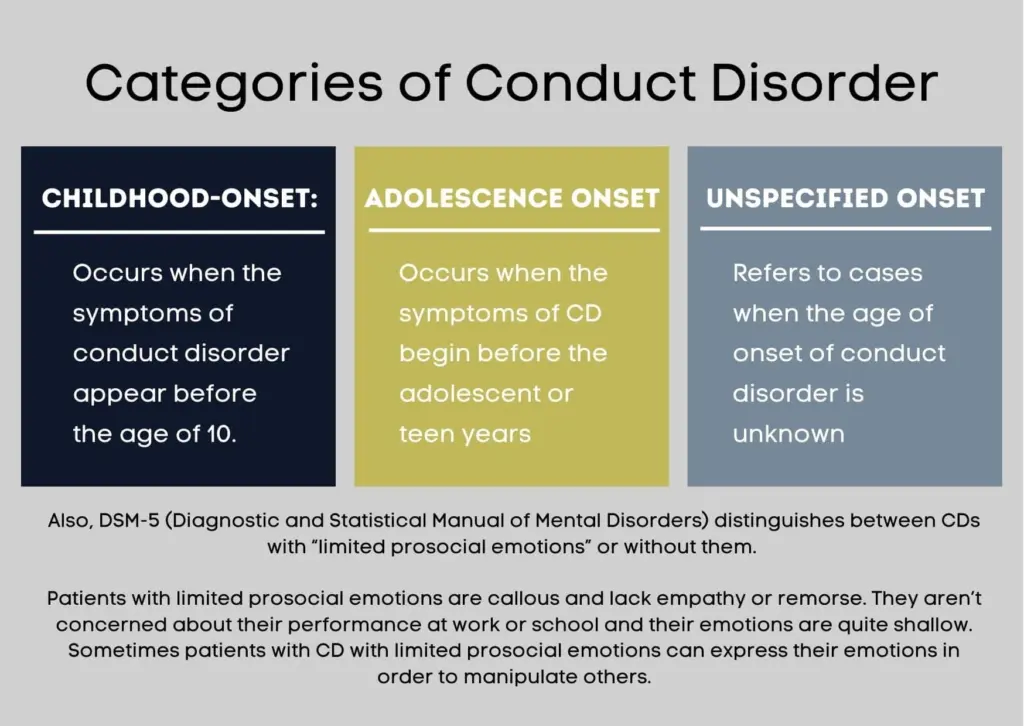
The categories of conduct disorder represent the basic types of the condition based on the age of onset. The categories of conduct disorder are listed below.
- Childhood-onset: occurs when the symptoms of conduct disorder appear before the age of 10
- Adolescence onset: occurs when the symptoms of CD begin before the adolescent or teen years
- Unspecified onset: refers to cases when the age of onset of conduct disorder is unknown
Also, DSM-5 distinguishes between CDs with “limited prosocial emotions” or without them. Patients with limited prosocial emotions are callous and lack empathy or remorse. They aren’t concerned about their performance at work or school and their emotions are quite shallow. Sometimes patients with CD with limited prosocial emotions can express their emotions in order to manipulate others.
What are the symptoms of Conduct disorder?
The causes of conduct disorder range from genetics to brain abnormalities, cognitive deficits, and social issues. Children with CD may have abnormalities in some regions of the brain. For example, their limbic system (involved in emotional responses) and prefrontal cortex (regulates judgment) could be impaired.
Some cognitive deficits can make children more vulnerable to conduct disorders. These include poor verbal skills, low IQ, and impaired executive functioning.
Additionally, a 2013 study by Catherine Tuvblad and Kevin M. Beaver published in the Journal of Criminal Justice confirmed that antisocial behavior is strongly associated with inherited genes. A lot more research on this subject is necessary to determine just how genes play a role in the development of CD.
Social issues associated with conduct disorder include poverty, family breakdown, poor schools, harsh parenting, lack of parental supervision, parental mental illness, and others. Trauma is also among the major conduct disorder causes. Children who experienced trauma may develop depression and behavioral problems. Mood disorders and conditions such as attention deficit hyperactivity disorder (ADHD) are also associated with the development of conduct disorder, according to an article titled, “Other Concerns and Conditions with ADHD” from the Centers for Disease Control and Prevention (CDC).

What are the causes of Conduct disorder?
The causes of conduct disorder range from genetics to brain abnormalities, cognitive deficits, and social issues. Children with CD may have abnormalities in some regions of the brain. For example, their limbic system (involved in emotional responses) and prefrontal cortex (regulates judgment) could be impaired.
Some cognitive deficits can make children more vulnerable to conduct disorders. These include poor verbal skills, low IQ, and impaired executive functioning.
Additionally, a study from the Journal of Criminal Justice confirmed that antisocial behavior is strongly associated with inherited genes. A lot more research on this subject is necessary to determine just how genes play a role in the development of CD.
Social issues associated with conduct disorder include poverty, family breakdown, poor schools, harsh parenting, lack of parental supervision, parental mental illness, and others. Trauma is also among the major conduct disorder causes. Children who experienced trauma may develop depression and behavioral problems.
Mood disorders and conditions such as attention deficit hyperactivity disorder (ADHD) are also associated with the development of conduct disorder, according to CDC.

What are the risk factors for Conduct disorder?
The risk factors for conduct disorder are listed below.
- Gender: Boys are more likely to develop conduct disorder than girls
- Family history: Having a parent or sibling with conduct disorder, substance abuse, or mental illness increases the risk of developing this condition
- Presence of other psychiatric disorders: Children and adolescents with other mental health problems are also more likely to have CD. Other mental health problems include mood or anxiety disorders, learning problems, ADHD, substance abuse, and PTSD
- Temperament: Having a difficult temperament puts a child or adolescent at a greater risk of CD
- Home environment: Children or adolescents who live in dysfunctional households are more likely to have CD. This is particularly the case for children or teens who are abused or neglected.
- Trauma: Experiencing trauma, at home or in any other environment, increases the risk of CD. The affected child or teen may choose violence and aggression to cope with the trauma they don’t know to resolve in other manners.
Generally speaking, any child or teen can develop a conduct disorder. Some of them are a higher risk, though. The most common conduct disorder risk factors include:
- Being a male
- Family history and negative home environment
- Having other mental health problems
- Living in poverty
- Being bullied or socializing with people who engage in or encourage violence and aggressive behaviors
- Living in an urban environment
How is Conduct disorder (CD) diagnosed?
Conduct disorder is diagnosed by a physician or mental health professional. The condition is diagnosed when a patient meets criteria from DSM-5 i.e. meets at least three behaviors such as aggression, vandalism, lying, violation of rules, and theft for at least six months.
Parents should schedule an appointment as soon as the child shows symptoms of CD. The healthcare professional asks parents and children questions about behavioral patterns. The doctor may perform a physical exam and order blood tests if they suspect physical problems cause behavioral issues.
Behavioral problems must strongly impair a child socially and at school, in order to be diagnosed with conduct disorder.
The process of diagnosis involves interviewing a child, reviewing records, and asking that teachers and parents complete questionnaires regarding the child’s behavior. Sometimes psychological testing and other evaluation tools are necessary for this purpose.

When does Conduct disorder (CD) begin?
Conduct disorder (CD) begins early, before the age of 10, according to chapter one of the book Child Psychopathology published by the Guilford Publications in 2014. The condition is generally diagnosed when a child is between 10 and 16 years old. The average age of diagnosis is 11. In most cases, boys are diagnosed with CD at an earlier age than girls.
What is the prevalence of Conduct disorder (CD)?
The estimated prevalence of conduct disorder in the world is 51.1 million as of 2013, according to a 2015 analysis for the Global Burden of Disease published in The Lancet. The prevalence of CD among children ranges from 1% to 10%. The 2006 juvenile justice bulletin from the Office of Juvenile Justice and Delinquency Prevention of the U.S. Department of Justice shows rates of CD among incarcerated youth or youth in juvenile detention facilities go from 23% to 87%.
There is no official nation- or population-wide statistics on this disorder. That’s why the prevalence of CD may vary from one research to another based on their sample size, location, and other effects.
A 2018 study by Patel et al., from the Behavioral Sciences found the estimated prevalence of conduct disorder was 9.5% with an average age of onset being 11.6 years. The study also showed the worldwide prevalence of CD among children aged 6 to 18 is 3.2%. About 70% of children with CD in this study were males.
According to a 2001 article titled, “Conduct Disorder: Diagnosis and Treatment in Primary Care” from the American Family Physician, about 6% to 16% of boys and 2% to 9% of girls in the U.S. meet the diagnostic criteria for CD.
Which children are at risk for Conduct disorder (CD)?

Conduct disorder is more common in boys, particularly if they also have other mental health problems. These problems include anxiety disorders, ADHD, PTSD, and others.
According to an article on conduct disorder from Johns Hopkins Medicine, children are more likely to develop conduct disorder if they live in homes that are disorganized, dysfunctional, and disadvantaged. Having a bad or difficult temperament also increases the risk of conduct disorder in children.
What is the treatment for Conduct disorder (CD) in children?
Treatment for conduct disorder in children depends on the severity of the condition, age, general health, and symptoms a child is experiencing. The treatment options for conduct disorder (CD) are listed below.
- Cognitive-behavioral therapy (CBT): this type of psychotherapy helps patients identify negative thoughts and behavior patterns in order to improve their communication skills, problem-solving, and coping with stressful situations. In other words, CBT helps patients control their anger and impulses. A paper by Riise et al., published in the February 2021 issue of Clinical Psychology Review confirmed that CBD is effective for children with externalizing disorders i.e. behavioral disorders
- Medications: While there is no medication for CD specifically, a doctor may prescribe medications to manage symptoms of other disorders such as ADHD
- Peer group therapy: helps children with conduct disorder develop better social and interpersonal skills
- Family therapy: Emphasizes improving family interactions and communication between children with conduct disorder and their parents.
Conduct disorder requires a proactive approach; it’s not wise to ignore it.
Proper treatment is necessary to prevent the detrimental effects of CD on a patient, family, and society. With treatment, a patient with CD can manage their emotions and reactions more effectively and thereby improve relationships with family, friends, and others.

