Barbiturates addiction: symptoms, effects, causes, and treatment
Barbiturates addiction refers to the compulsive and uncontrollable use of barbiturates–a class of sedative-hypnotic medications or central nervous system depressants–despite significant adverse health, social, and financial outcomes. According to the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), barbiturates addiction is a form of sedative, hypnotic, or anxiolytic use disorder.
The symptoms of barbiturates addiction are loss of control over drug use, cravings, and persistent use despite facing adverse consequences and under hazardous conditions. Other symptoms include spending increasing amounts of time on drug-related activities, neglecting personal and professional responsibilities to engage in drug use, and developing tolerance and dependence.
The effects of barbiturates addiction include respiratory issues; insomnia; damage to organs like the heart, kidneys, liver, and brain; cognitive impairment; sexual disorders; impaired balance and motor control; and manifestation of psychotic behaviors like hallucinations and delusions.
The causes of barbiturates addiction are misusing, self-medicating, developing increasing tolerance and dependence, and manifesting withdrawal syndrome.
The treatments available for barbiturate addiction include detoxification, inpatient therapy, outpatient therapy, cognitive-behavioral therapy, and contingency management.
What is barbiturates addiction?
Barbiturates addiction refers to the chronic condition where an individual engages in compulsive and uncontrollable use of barbiturates–a class of sedative-hypnotic medications or central nervous system depressants–despite the adverse physical, psychological, socio-economic, and financial effects stemming from their drug use. The condition is marked by physiological symptoms like the development of physical tolerance and psychological dependence.
Per the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), an addiction to barbiturates is a form of sedative, hypnotic, or anxiolytic use disorder. Typically, there are two usage scenarios where individuals develop an addiction to sedative-hypnotic drugs: taking the drug for a neurologic or psychiatric ailment and using it to self-medicate or derive an euphoric “high.”
How common is barbiturates addiction?
Barbiturates addiction is not as common when compared to its widespread prevalence before the 1970s when federal regulations were imposed in the US to restrict the dispersion of the drug. The Substance Abuse and Mental Health Services Administration (SAMHSA) classifies barbiturates under prescription sedatives and provides cumulative data on prescription tranquilizer and sedative misuse across diverse demographics in its September 2020 report titled “Key Substance Use and Mental Health Indicators in the United States: Results from the 2019 National Survey on Drug Use and Health.”
According to this report, the percentage of individuals in the US aged 12 years or more who reported misusing prescription tranquilizers and sedatives in the previous year decreased from 2.6 (or 7.0 million people) in 2015 to 2.1 (or 5.9 million people) in 2019. The proportion of individuals aged 26 years or older who reported misusing prescription tranquilizers and sedatives in the past year decreased from 2.2% in 2015 to 1.9% in 2019.
What are barbiturates?
Barbiturates are central nervous system (CNS) depressants that belong to a class of drugs known as sedative-hypnotics. They slow down the functions of the CNS and induce drowsiness and feelings of relaxation. They have historically been used to treat conditions like insomnia, seizures, and migraines. However, they are less commonly prescribed today owing to their addictive potential and low safety profile. Barbiturates comprise multiple drugs with varied formulations, which are classified as Schedule II, III, or IV controlled substances. This classification indicates that although these substances have abuse potential, they still have therapeutic uses.
The US Food and Drug Administration (FDA) approves barbiturates to be used to manage insomnia, seizure disorders, pre-surgical anxiety, neonatal withdrawal, and for anesthesia and medically-induced coma.
Which drugs are barbiturates?
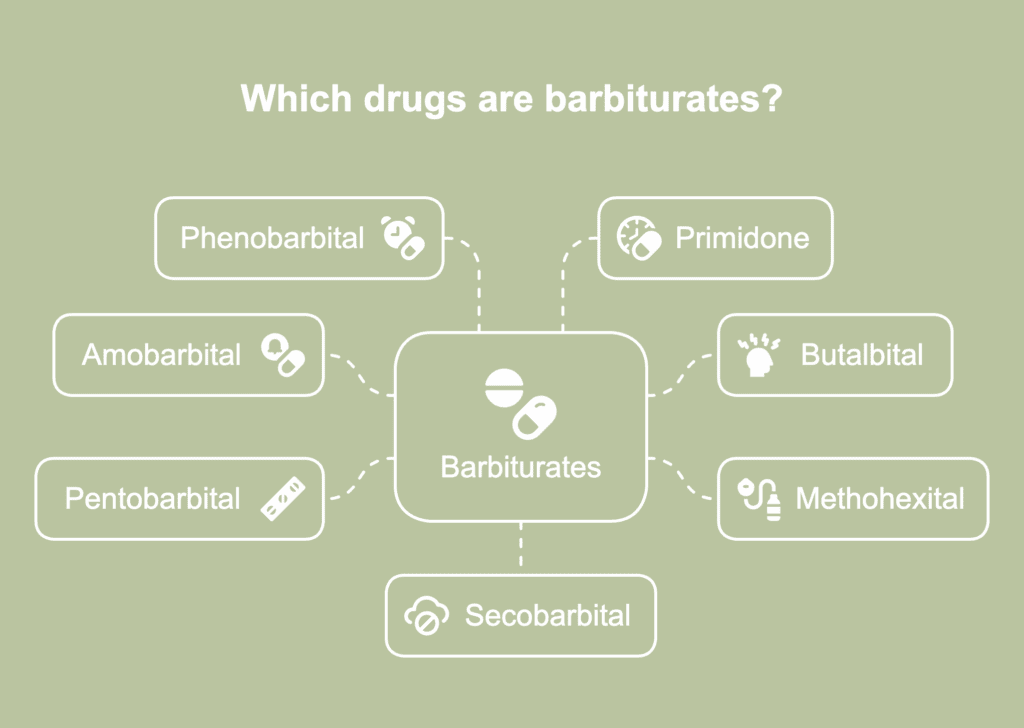
The drugs which are barbiturates are listed below.
- Amobarbital: Amobarbital is an intermediate-acting form of barbiturate whose effects last between 2 and 6 hours. It is a sedative-hypnotic drug prescribed only for short-term usage to treat insomnia. It is also used during multiple neurological tests.
- Butalbital: It is an intermediate-acting form of barbiturate whose effects last for about 4 hours. It is used as a component in multiple medicinal formulations for tension headaches and migraines.
- Methohexital: Methohexital is an ultra-short-acting form of barbiturate. It is used as an anesthetic agent in cardioversion and pediatric outpatient surgery settings. It is extremely effective in electroconvulsive therapy.
- Pentobarbital: This short-acting barbiturate is a hypnotic drug whose effects manifest within 10-15 minutes of administration but last only 3-4 hours. It is used as a pre-anesthetic medicine for status epilepticus and also to halt ongoing seizures.
- Phenobarbital: It is a long-acting form of barbiturate whose effects take about an hour to manifest and last longer than 6 hours, sometimes up to 12 hours. Physicians prescribe it to manage barbiturate withdrawal symptoms. It is used to prevent the onset of or stop ongoing seizures. It has extensive usage as an antiepileptic medicine for neonates, children, and adults.
- Primidone: This long-acting barbiturate is used to control specific types of seizures.
- Secobarbital: This short-acting barbiturate is used for treating insomnia and to ease anxiety in patients about to undergo surgery.
What are the common street names for barbiturates?
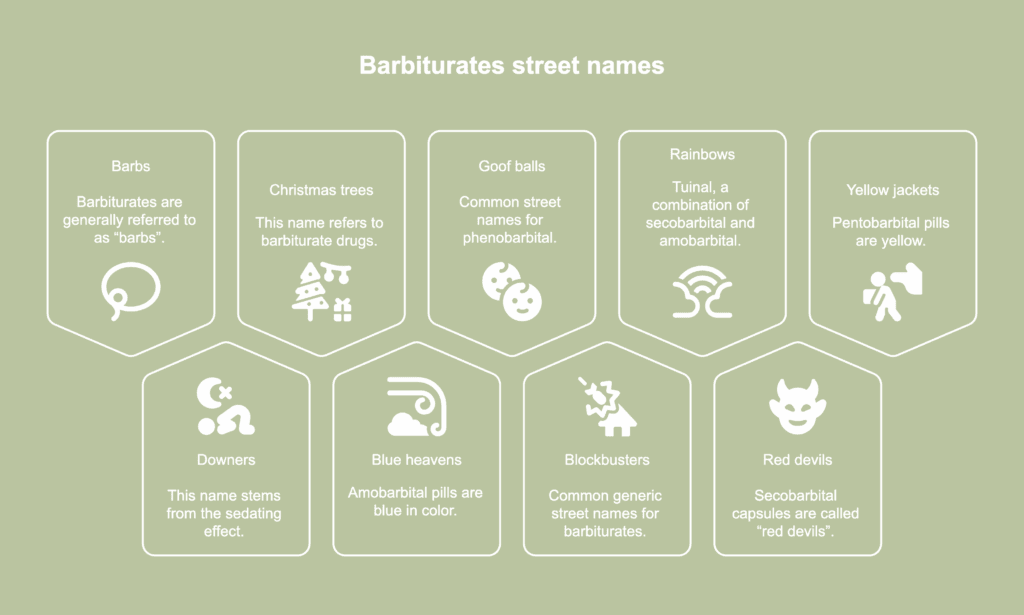
The common street names for barbiturates are listed below.
- Barbs: Barbiturates, in general, are referred to as “barbs,” an abbreviated form of the word.
- Downers: This name stems from the sedating effect of barbiturates. However, “downers” is generally used to refer to all drugs that induce sleep and relaxation.
- Christmas trees: This name refers to barbiturate drugs in general.
- Blue heavens: Barbiturates users refer to amobarbital as “blue heavens,” “blue velvets,” or “blue devils” because its pills are blue in color.
- Goof balls: “Goof balls” and “purple heart” are common street names for phenobarbital.
- Blockbusters: “Blockbusters” and “sleepers” are common generic street names for barbiturates.
- Rainbows: Drug users refer to Tuinal, a combination of secobarbital and amobarbital, as “rainbows” or “double trouble” for its powerful effects. Other common street names for Tuinal are “F-66s,” “reds and blues,” “gorilla pills,” and “tooies.”
- Red devils: Drug dealers commonly use the names “red devils” or “red” to refer to secobarbital. Secobarbital capsules are called “red dillies” or “red birds” for their characteristic red color. Other common street names for this drug are “F-40s,” “pink ladies,” “pinks,” and “seggy.”
- Yellow jackets: Barbiturates users refer to pentobarbital as “yellow jackets” because its pills are yellow. Alternatively, pentobarbital pills are called “nembies,” “abbots,” or “Mexican yellows.”
Are barbiturates still commonly prescribed?
No, barbiturates are not commonly prescribed now because of their high toxicity and abuse potential. They are no longer routinely prescribed for managing conditions like anxiety, insomnia, and headaches. They have been replaced by safer alternatives like benzodiazepines. However, barbiturates are prescribed in a limited manner to prevent or manage symptoms of epileptic or non-epileptic seizures when first-line treatments fail or to sedate patients before medical procedures.They are also prescribed as last-resort treatment for treating insomnia in adults and children. In emergency medical settings, barbiturates are used to induce coma in patients with brain trauma. They have been shown to decrease intracranial pressure by reducing the buildup of cerebrospinal fluid inside the skull.
What makes barbiturates addictive?
The ability of barbiturates to induce feelings of calmness and euphoria makes them addictive. They initially produce psychological dependence that later progresses to physical dependence with continued use. Barbiturates drugs with varied formulations are classified as controlled substances under the US Controlled Substances Act due to their high addictive potential.
Author P. T. Orbán in a 1976 paper titled “Barbiturate abuse” published in the Journal of Medical Ethics explains how abuse of barbiturates progresses to addiction. A section of the population who abuse barbiturates are initially prescribed the drug for a medical condition. They start using the drug in increased amounts or more frequently when they become psychologically dependent on the euphoric high that it produces. Even a single dose of a barbiturate drug is known to produce tolerance, a development that leads to increased or more frequent usage. Sustained usage of barbiturates produces physical dependence on the drug. The development of dependence is associated with unpleasant and distressful withdrawal symptoms. Individuals are then compelled to continue taking the drug to escape the discomfort of withdrawal.
Rapidly-acting barbiturates tend to be more addictive than the longer-acting ones. Short-acting barbiturates tend to produce intoxication and mood changes, the latter phenomenon associated with the “high” that users desire. This makes these kinds of barbiturates more likely to produce dependence.
What are the effects of barbiturates on the brain?

The effects of barbiturates on the brain are listed below.
- Increasing the concentration of GABA: Barbiturates increase the concentration of gamma-aminobutyric acid (GABA), according to a StatPearls [Internet] release by Skibiski et al., titled “Barbiturates” last updated on 29 January 2024. GABA is an inhibitory neurotransmitter. The enhanced effects of GABA result in a slowing down of the activities of the CNS, inducing effects like sleepiness and impaired muscle control that affect walking, balance, eye movements, speech, and swallowing.
- Decreasing glutamate activity: Barbiturates dampen the activity of the CNS by decreasing response to glutamate, an excitatory neurotransmitter, according to a StatPearls [Internet] release by Suddock et al., titled “Barbiturate Toxicity” last updated on 28 February 2024.
- Decreasing cerebral metabolic rate and blood flow: Barbiturates decrease cerebral metabolic rate and cerebral blood flow. The drug impact on the brain is evident from signs like reduced mental consciousness, ranging from confusion to coma.
- Depressing the respiratory medullary centers: Barbiturates affect the brain’s respiratory control centers that regulate breathing. Respiratory depression manifests as slow and/or shallow breathing that leads to a buildup of carbon dioxide in the blood. Other signs are frequent yawns and a fast heart rate.
What is the difference between barbiturates and stimulants?
The difference between barbiturates and stimulants stems from their effects on the central nervous system and their usage scenarios. The differences are described in the table below.
| Barbiturates | Stimulants |
|---|---|
| Barbiturates are sedative-hypnotic drugs or depressants that dampen the activity of the central nervous system. | Stimulants excite the central nervous system and heighten its activity. |
| They produce effects like sedation, reduced anxiety and a sense of calmness, and improved sleep, depending on dosage. | They produce effects like elevated heart rate and blood pressure and increased levels of energy and mental alertness. |
| Common barbiturates include approved medications like phenobarbital, butalbital, pentobarbital, amobarbital, methohexital, and primidone. | Common stimulants include nicotine, caffeine, cocaine, amphetamines, methamphetamine, and methylphenidate. |
| Historically, they were used as anti-anxiety and sleep medications and at present, they are typically used as anesthetics and anticonvulsants in clinical settings and for self-medicating anxiety and stress. | Although they are prescribed as medications for conditions like attention-deficit hyperactivity disorder, stimulants are more commonly used as recreational drugs. |
| Barbiturates are prescribed in limited settings and have either been discontinued or replaced with benzodiazepines. | Stimulants are available widely and legally as substances like caffeine and prescribed medications like Ritalin and Concerta. |
What are the symptoms of barbiturates addiction?
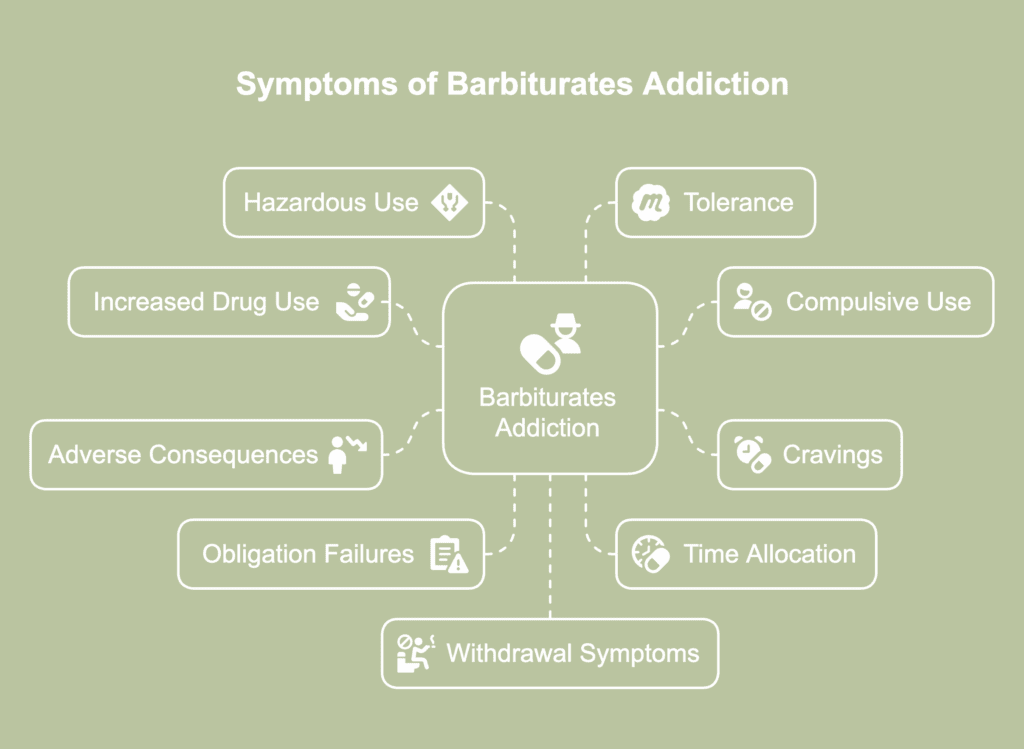
The symptoms of barbiturates addiction are listed below.
- Taking more of the drug than intended or prescribed: Individuals who are addicted to barbiturates tend to take the drug in increasing amounts or more frequently than intended or prescribed originally. It is not unlikely for them to go doctor shopping, a prevalent form of prescription medication diversion, to obtain the drugs.
- Being unable to control usage despite wanting to: Compulsive drug use is a hallmark of addiction. Individuals who are addicted to barbiturates feel compelled to take the drug, daily and often several times a day.
- Experiencing cravings: Individuals with an addiction to barbiturates experience frequent and powerful cravings to use the drug in the presence of internal and external stimuli, which include drug-related cues in the environment, mental stress, and powerful emotional states. These intense urges to take the drug are intrusive and block out all other thoughts.
- Persisting in use despite adverse consequences: Individuals addicted to barbiturates develop tendencies like persisting in taking the drug despite facing adverse health, personal, social, financial, and professional consequences that their drug-use habits have triggered or aggravated.
- Failing to fulfill personal, social, and professional obligations: Increasing preoccupation with drug-related activities and barbiturates-induced physical, cognitive, and/psychological impairments are the reasons addicted individuals fail to fulfill their personal, professional, and social responsibilities.
- Spending increasing amounts of time on drug-related activities: As drug use intensifies, barbiturates users tend to spend increasing amounts of time thinking about, procuring, consuming, and recovering from the effects of the substance. They tend to forego or reduce meaningful social, recreational, and professional activities in favor of drug-related ones.
- Using the drug in hazardous situations: There is a tendency to use the drug under physically hazardous situations or in ways that are likely to cause harm to oneself or others.
- Developing tolerance: Chronic barbiturates abuse leads to tolerance where the individual needs more of the drug to experience the same or the desired effect.
- Manifesting withdrawal symptoms: Experiencing withdrawal symptoms after reducing use or quitting barbiturates indicates physical dependence. Dependence and withdrawal result from prolonged barbiturates use and are characteristic features of addiction.
What are the effects of barbiturates addiction?
The effects of barbiturates addiction are listed below.
- Short-term effects: The common short-term effects are respiratory distress, insomnia, heightened sensitivity to sounds or physical pain, and trouble forming memories. Abnormal menstrual cycles in women and impotence in men, and in rare instances, psychotic behaviors like hallucinating or being delusional are the other short-term effects of barbiturates addiction.
- Long-term effects: The long-term effects include respiratory issues like bronchitis or pneumonia that stem from chronic drug-induced breathing troubles; uncoordinated bodily movements that manifest as twitching and impaired balance and motor coordination; anxiety and depression; liver and/or kidney damage; cardiac problems; and sexual disorders. Chronic barbiturate abuse is linked to brain damage with symptoms like impaired learning, memory, and problem-solving abilities and shortened attention span.
What are the complications of barbiturates addiction?
The complications of barbiturates addiction are listed below.
- Development of tolerance and/or dependence: Barbiturates are highly addictive. Repeated use of the drug has been shown to produce rapid tolerance to its mood-altering properties. Long-term and excessive use of barbiturates is linked to the development of physical dependence, a phenomenon where reducing usage or quitting produces uncomfortable withdrawal symptoms.
- Misuse leading to cardiac and breathing complications: Barbiturates lower blood pressure and heart rate. Taking the drug more frequently or in amounts greater than what has been prescribed increases the risk of an individual developing life-threatening breathing issues.
- Adverse drug-drug interactions: Barbiturates affect the liver causing the organ to metabolize other drugs too rapidly and thus reducing their efficacy. For instance, taking phenobarbital with other medications like warfarin, immunosuppressants, steroids, hormonal contraceptives, antiepileptic drugs, and hepatitis C drugs reduces their efficacy, as noted in a StatPearls [Internet] release by Skibiski et al., titled “Barbiturates” last updated on 29 January 2024. Polysubstance users who tend to mix barbiturates with other CNS depressants like alcohol, benzodiazepines, and opioids have an increased risk of developing severe respiratory distress and exhibiting oversedation.
- Hepatotoxicity: Phenobarbital has been implicated in drug-induced liver damage in specific populations of barbiturates users. Liver injury associated with barbiturates use is known to cause allergic reactions and rashes on the skin.
- Fetal and newborn abnormalities: Barbiturates taken during pregnancy increase the risk of prolonged labor, birth defects, and neonatal barbiturate withdrawal syndrome, according to a 2012 article by Sunil Kumar Pandey and Deepanjana Dass published in the Journal of Applied Pharmaceutical Science, titled “Drugs of Physical Harm in Pregnancy: Nature Vs Nurture-A Silent Battle.” Infants of mothers who used barbiturates during pregnancy have an increased risk of being born with a cleft lip or cleft palate, exhibiting cardiac abnormalities and defects of the spinal cord, having hypertelorism or very wide-spaced eyes, and possessing a high risk of developing brain tumors. These infants are born addicted to barbiturates and show symptoms like trouble breathing and sleeping, fever, irritability, inability to feed adequately, and failure to thrive. Nursing mothers who take barbiturates pass on the drug to their infants who are then likely to develop complications like slowed heartbeat, breathing problems, and increased drowsiness.
What happens if you overdose on barbiturates?
Overdosing on barbiturates leads to severe adverse effects that are likely to cause considerable morbidity and even mortality if prompt medical intervention is not initiated, according to a StatPearls [Internet] release by Suddock et al., titled “Barbiturate Toxicity” last updated on 28 February 2024. Barbiturates have a narrow therapeutic index, meaning that there is only a slim margin of difference between a therapeutic dose and one that is toxic. Overdosing on barbiturates manifests as symptoms like breathing trouble, an abnormal pulse rate which is either slow or fast but weak, mental confusion, low body temperature, drop in blood pressure, nausea and vomiting, excessive thirst, dizziness, and muscle weakness. Abnormal eye movement, dilated pupils, a bluish tint to the lips and/or fingernails, and fainting are other signs of barbiturates overdose. Cerebral edema, pulmonary edema, myocardial infarction, and aspiration pneumonia are some severe complications caused by barbiturates toxicity. It is possible for acute barbiturate toxicity to result in coma and even death.
Barbiturates users with comorbid conditions are more vulnerable to a drug overdose and the drug’s toxic effects than healthy individuals. For instance, barbiturate-induced respiratory depression is likely to be more severe in individuals with chronic pulmonary obstructive disorder, even at therapeutic doses, than in those who do not have a lung disorder. Barbiturate users who tend to mix the drug with other substances of abuse, such as alcohol or opioids, to increase the potency of the latter, are vulnerable to an overdose. Aged individuals have an increased risk of overdosing on the drug, even at low doses.
What are the causes of barbiturates addiction?
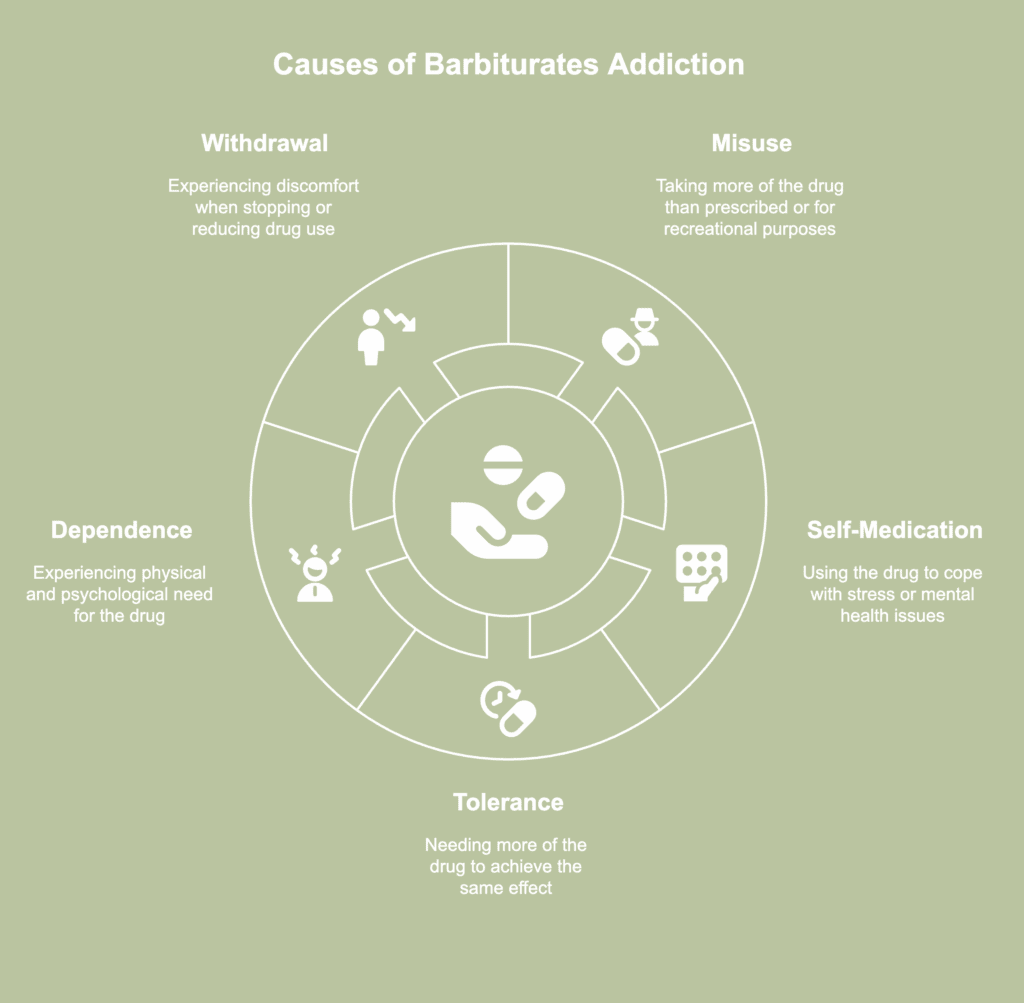
The causes of barbiturates addiction are listed below.
- Misuse: CNS depressants are one of the most abused classes of drugs among prescription medications, reports the National Institute on Drug Abuse in its research report titled “Prescription Drug Abuse” last revised in October 2011.Those who misuse barbiturates tend to take more of the substance, for longer than what was originally prescribed, or more frequently. A percentage of users use the drug recreationally to derive a “high.” These individuals obtain these drugs legally using prescriptions or illegally, such as by using the drugs prescribed to another individual or buying from a street dealer.
- Self-medication: Misuse of barbiturates has been observed among users who tend to self-medicate to cope with psychological stress or the symptoms of a mental health issue like anxiety. Self-medication, over time, has been shown to be one of the most potent causes of addiction.
- Development of increasing tolerance: Tolerance to the mood-altering properties of barbiturates tends to develop rapidly. In a section of the drug-using population, tolerance triggers an addiction to the substance.
- Development of dependence: Short-acting hypnotic barbiturates that induce intoxication and mood alterations tend to be abused and are known to cause dependence. It has been observed that taking 450 mg of a hypnotic barbiturate every day for 8 weeks leads to the development of physical and psychological dependence on the drug, according to P. T. Orbán in a 1976 paper titled “Barbiturate abuse” published in the Journal of Medical Ethics.
- Manifestation of withdrawal syndrome: The development of physical dependence on a substance manifests as distressful physical and psychological withdrawal symptoms when the drug is stopped or its usage reduced. The transition from intermittent drug misuse to compulsive drug taking is often the result of the individual’s attempts to escape the discomfort of withdrawal.
What are the risk factors for barbiturates addiction?
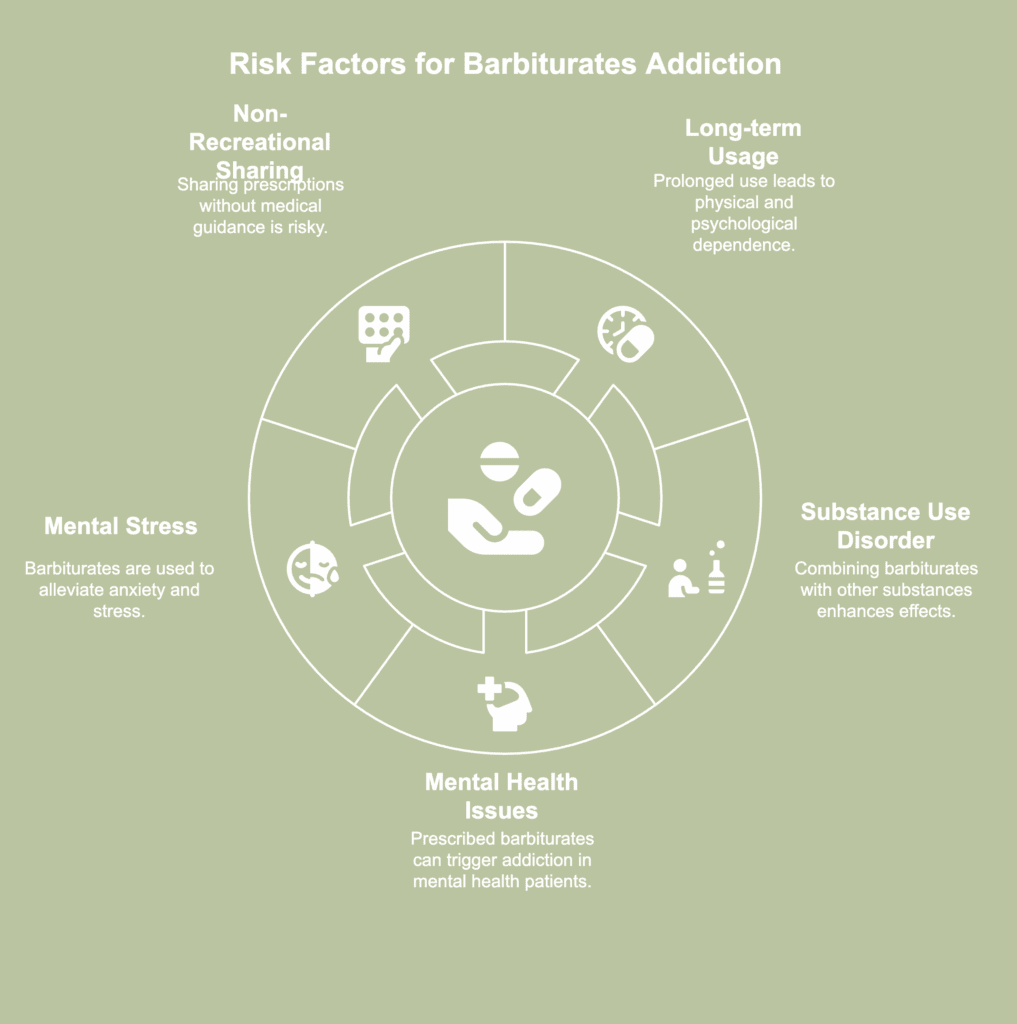
The risk factors for barbiturates addiction are listed below.
- Long-term or excessive usage: Long-term or excessive use of barbiturates is associated with the development of physical and psychological dependence on the substance. Physical dependence triggers withdrawal syndrome, which is one of the most potent risk factors for addiction.
- Presence of a substance use disorder (SUD): Individuals who abuse substances like alcohol and opioids are known to take barbiturates to magnify the effects of the former. For instance, those on opiate maintenance therapy take barbiturates to derive a more intense euphoric rush. Individuals abusing stimulants like amphetamines take barbiturates to induce sleep. It has also been noted that the sedating properties of barbiturates are desired and thus sought after by individuals with a history of substance abuse.
- Presence of mental health issues: Barbiturates prescribed for specific mental health issues like insomnia and anxiety carry the risk of triggering the development of addiction. This is true for barbiturate drugs like phenobarbital when they are prescribed for insomnia, according to a StatPearls [Internet] release by Lewis et al., titled “Phenobarbital” last updated on 28 February 2024.
- M ental stress: Barbiturates reduce anxiety and are thus desirable to a section of individuals experiencing psychological stress and seeking ways to alleviate their symptoms.
- Non-recreational prescription medication sharing: Barbiturates misuse is prevalent among young people who are likely to obtain it from an individual who has been prescribed the drug. It is possible that the individual who has a prescription for the drug shares their medications with an acquaintance or a loved one with similar symptoms. This is a risky practice because the end user is not guided by dosage instructions from a physician that are suited to their unique medical needs.
What treatments are available for barbiturate addiction?
The treatments available for barbiturate addiction are listed below.
- Detoxification: It is possible for barbiturate withdrawal symptoms to rapidly aggravate and become life-threatening. So, detoxification should be carried out under round-the-clock medical supervision, preferably at a specialized inpatient facility, to ensure patient safety. The drug detoxification process typically involves tapering the dosage.
- Inpatient treatment: Inpatient addiction treatment facilities provide 24×7 care at varying levels and tailored to the unique medical and psychological needs of individual patients. The therapeutic interventions include group and individual therapies, behavioral counseling, psychoeducation, and pharmacotherapy, which are delivered at a residential facility and in a structured and supervised environment.
- Outpatient treatment: Outpatient facilities allow barbiturate users seeking recovery to access therapeutic services without having to stay at the facility and while carrying on with their daily lives. Addiction treatment services at outpatient facilities are delivered via intensive outpatient programs, partial hospitalization programs, and standard outpatient programs. These modalities differ according to the level of care they provide.
- Cognitive-behavioral therapy (CBT): There is substantial scientific literature that points to the efficacy of CBT in treating SUDs and promoting long-lasting addiction recovery. CBT focuses on identifying maladaptive thinking and behavioral patterns and replacing these with healthy and positive ones.
- Contingency management (CM): CM is a behavioral modification approach where reinforcers are delivered when a patient exhibits verifiable abstinence behavior. It is an evidence-based and standardized practice that has been shown to be effective in treating SUDs and promoting long-lasting abstinence.
What are the symptoms of barbiturates withdrawal?

The symptoms of barbiturates withdrawal are listed below.
- Restlessness: Symptoms like restlessness and agitation resemble those observed during alcohol withdrawal and typically manifest during the initial stage of withdrawal.
- Elevated pulse rate and body temperature: Symptoms like excessive sweating resulting from high core body temperature, changes in heart rate, and elevated blood pressure are observed during the initial stage of withdrawal and peak around 72 hours of stopping drug use.
- Depression: This is a mild symptom but has been observed to persist in chronic abusers of barbiturates.
- Tremors: Tremors or shaking are typically noticed in the hands.
- Nausea and vomiting: Symptoms like nausea, vomiting, and abdominal cramps peak between the second and third day of drug withdrawal.
- Anxiety: This is typically a rebound effect.
- Insomnia: The symptom typically manifests around the fourth day of withdrawal and starts to subside from about the seventh day.
- Psychosis: The symptoms include delirium or confusion marked by spatial and temporal disorientation and hallucinations that are typically visual in nature. It has been seen that about 66% of the individuals experience delirium that persists for several days. Suicidal ideations have been observed in individuals experiencing severe psychosis.
- Seizures: Grand mal seizures are a severe symptom. These occur between 24 and 115 hours of drug withdrawal. On average, about 75% of the individuals who exhibit this symptom experience more than one seizure.


