Valium (diazepam) addiction: definition, symptoms, side effects, risk factors, and treatment
Table of content
- What is Valium (diazepam) addiction?
- What are the symptoms of Valium (diazepam) addiction?
- What are the side effects of Valium (diazepam) addiction?
- What are the causes of Valium addiction?
- What are the risk factors for Valium addiction?
- How is Valium addiction diagnosed?
- What are the available treatments for Valium addiction?
- How is Valium addiction prevented?

Valium (diazepam) addiction occurs when an individual develops a physical or psychological dependence on the medication, often used to treat anxiety or muscle spasms. Addiction presents as compulsive usage and cravings, despite adverse impacts on health or daily functioning.
The symptoms of Valium (diazepam) addiction include drowsiness, dry mouth, impaired coordination, rapid heartbeat, doctor shopping, paranoia, nervousness, and suicidal thoughts.
The side effects of Valium (diazepam) addiction are fatigue, dizziness, impaired coordination, confusion, aggressiveness, skin rash, and blurred vision.
The risk factors for Valium addiction include impulsive personality traits, young age at first use, medical prescription and tolerance, socioeconomic factors, and psychiatric comorbidities.
Treatment options for Valium addiction include detoxification, cognitive behavioral therapy (CBT), inpatient rehabilitation programs, outpatient care, and support groups.
What is Valium (diazepam) addiction?
Valium (diazepam) addiction is a condition where an individual repeatedly misuses the prescription drug Valium, commonly taken for anxiety, muscle spasms, or seizure disorders. This reliance leads to withdrawal symptoms when attempting to stop or reduce use.
The condition falls under benzodiazepine addiction because Valium belongs to the benzodiazepine class of drugs. As tolerance grows, larger and higher doses are required to produce the same soothing or relaxing effects.
Professional treatment is necessary for recovery since the compulsive nature of the addiction frequently leads people to abuse the drug in spite of the negative effects.
What is Valium (diazepam)?
Valium (diazepam) is a prescription medication classified as a benzodiazepine. Muscle spasms, seizures, anxiety disorders, and the symptoms of alcohol withdrawal are the conditions for which it is most frequently prescribed.
As a benzodiazepine, Valium functions by amplifying the effects of gamma-aminobutyric acid (GABA), a neurotransmitter in the brain that mitigates nerve activity. The drug has a wide variety of off-label uses, including sedation before and after surgery, insomnia, and restless leg syndrome, according to a 2014 paper by Nicholas E. Calcaterra and James C. Barrow titled, “Classics in Chemical Neuroscience: Diazepam (Valium).”
Is Valium a controlled substance?

Yes, Valium is a controlled substance. Under the Controlled Substances Act, it is categorized as a Schedule IV substance in the United States, therefore possessing a known medicinal use but carrying a danger of misuse and dependence.
A continuing education activity last updated in August 2023 titled, “Diazepam” by Dhaliwal et al., indicated that patients who are prone to addiction, are receiving long-term treatment, or are taking large doses are likely to develop tolerance and dependence. These people need to be closely monitored because withdrawal symptoms are more likely to occur once dependence takes place.
How addictive is Valium?
Valium tends to be quite addictive, especially when used regularly over extended periods. The medication functions by amplifying the actions of GABA in the brain, resulting in a tranquilizing effect.
However, with prolonged use, the body starts to rely on Valium to maintain this sense of calm, and tolerance builds up, requiring higher doses to achieve the same effect. Developing dependence makes it difficult for a person to give up the drug without going through withdrawal.
Valium is a drug with considerable addictive potential because of this cycle of dependence and withdrawal, particularly if taken without close medical monitoring.
Can you become addicted to Valium after one use?
No, you cannot become addicted to Valium after one use. Addiction usually develops over time and involves repeated, sustained use of a drug, leading to physical and psychological dependence.
With Valium, addiction stems from the cumulative effect of the drug on the brain’s chemistry, where ongoing use leads to tolerance and a need for higher doses to achieve the same calming effects.
However, even a single dose of Valium creates a sense of relaxation or euphoria, which encourages certain people to use it again. While this single-use experience tends to be pleasant, it typically doesn’t lead to immediate addiction.
Can you get addicted to diazepam (Valium) when used as prescribed by a doctor?
Yes, you can become addicted to diazepam (Valium) even when used as prescribed by a doctor. While following medical instructions lowers the risk, diazepam is inherently habit-forming because of its effect on the brain’s neurotransmitters, particularly GABA, which induces relaxation and reduces anxiety.
Over time, even at prescribed doses, the brain becomes accustomed to this external calming influence, leading to tolerance where the initial dose no longer has the same effect. However, risks of anxiolytic addiction such as Valium dependence are minimized when the medication is used for short periods or as part of a carefully managed treatment plan.
Regular medical supervision and adherence to the prescribed regimen help reduce the chance of developing an addiction.
What makes Valium so addictive?
What makes Valium so addictive is its capacity to enhance the effects of the neurotransmitter gamma-aminobutyric acid (GABA), which naturally reduces brain activity and encourages relaxation.
When someone takes Valium, the increased GABA activity slows down brain function. This leads to a soothing sense of calm and quickly becomes psychologically reinforcing, rendering the drug especially efficacious for alleviating anxiety; nonetheless, this mechanism of action results in the brain becoming progressively dependent on Valium for these benefits.
Over time, physical and psychological dependence forms as the brain adapts to the drug’s presence, creating a cycle of use that is often difficult to break. How drugs impact the brain is central to understanding this process—Valium essentially rewires the brain’s chemistry, diminishing its ability to manage anxiety and stress naturally.
How common is Valium addiction?
Valium addiction is relatively common, especially among individuals prescribed the drug for long-term use or in high doses. Even though the rates of Valium addiction in children are not distinctly reported in available data, a 2023 publication titled, “Key Substance Use and Mental Health Indicators in the United States: Results from the 2022 National Survey on Drug Use and Health” from the Substance Abuse and Mental Health Services Administration indicated that 137,000 teenagers between the ages of 12 and 17 (0.5 percent) abused benzodiazepine tranquilizers, which include diazepam products, during the previous 12 months.
The epidemiology of substance abuse reveals notable trends related to Valium addiction across demographics. While exact statistics on Valium addiction in men and women are scarce, women were more likely than men to have received a prescription for a benzodiazepine (58% of women versus 44% of men), according to a 2022 study by McHugh et al., titled, “Sex differences in benzodiazepine misuse among adults with substance use disorders.”
It is worth noting, however, that there was no discernible difference in the overall prevalence of benzodiazepine abuse between the sexes, despite the fact that both men and women reported high rates of usage (over 40% in each group).
Despite the acknowledged hazards for elderly people, prescription usage of benzodiazepines, such as Valium, rises gradually with age, as per a 2014 publication from the National Institutes of Health titled, “Despite risks, benzodiazepine use highest in older people.”
Moreover, data from 2008 showed that 31.4% of benzodiazepine users between the ages of 65 and 80 had prescriptions for longer than 120 days, which is regarded as long-term usage.
What are the symptoms of Valium (diazepam) addiction?
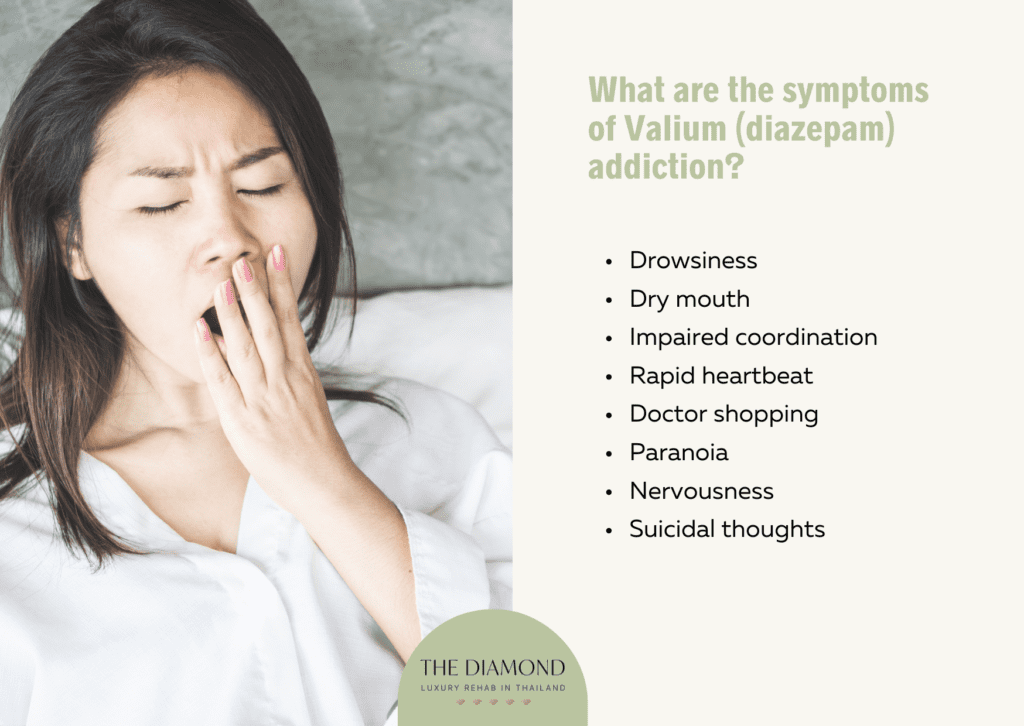
Symptoms of Valium (diazepam) addiction refer to the physical, behavioral, and psychological signs indicating a dependency on the drug. The symptoms of Valium (diazepam) addiction are listed below.
- Drowsiness: Individuals addicted to Valium often experience persistent drowsiness, as the drug’s sedative effects suppress normal energy levels. Drowsiness leads to reduced productivity and difficulties in maintaining focus on daily tasks. Constant fatigue disrupts personal and professional life, as individuals struggle to stay alert.
- Dry mouth: Chronic Valium use often results in a dry mouth, as the drug impacts salivary gland function. This uncomfortable symptom leads to bad breath and even dental issues, as saliva plays a critical role in protecting oral health. The sensation of dryness prompts frequent drinking of liquids, yet often remains persistent.
- Impaired coordination: Valium addiction frequently causes impaired coordination, as the drug slows down central nervous system activity. Individuals find themselves unsteady, increasing the risk of falls or accidents. Tasks requiring balance or precise movements, such as driving or operating machinery, become particularly dangerous.
- Rapid heartbeat: Valium addiction leads to cardiovascular symptoms, such as a pounding heart or palpitations, particularly when the drug is wearing off. These sudden heart sensations cause alarm, leading to increased anxiety and panic in certain individuals. Results of a 2017 paper by Costa et al., titled, “Effect of Diazepam on 24-Hour Blood Pressure and Heart Rate in Healthy Young Volunteers” revealed that in healthy young individuals, long-term nighttime diazepam (5 mg) treatment significantly raised 24-hour HR by about 5.2 beats per minute as compared to a placebo. People with cardiovascular concerns, such as elderly people or those with heart disease, must exercise caution in light of this finding.
- Doctor shopping: Doctor shopping, or visiting multiple doctors to obtain more prescriptions, is a common behavior among people addicted to Valium. Such practice lets people accumulate larger doses without drawing attention from one doctor. Doctor shopping strains the healthcare system and has ethical as well as legal consequences.
- Paranoia: People addicted to Valium experience paranoia, feeling excessively suspicious or fearful without clear reasons. A heightened sense of distrust causes individuals to distance themselves from others, complicating relationships. Paranoia additionally stems from the anxiety that withdrawal triggers, especially when doses are missed.
- Nervousness: Persistent nervousness, especially between doses, is common as the body craves Valium’s calming effect. Individuals feel restless, tense, or unable to relax, even in situations that don’t normally cause stress. The sense of unease often intensifies over time, making daily activities challenging.
- Suicidal thoughts: Addiction to Valium leads to intense feelings of hopelessness and despair, causing affected individuals to experience suicidal thoughts. The toll addiction takes on daily life, relationships, and health drives these thoughts. Withdrawal aggravates mental health issues, consequently amplifying feelings of worthlessness. For anyone experiencing such thoughts, immediate support is vital since they mirror the severe mental effect of addiction.
What are the side effects of Valium (diazepam) addiction?

Side effects of Valium (diazepam) addiction refer to the unintended reactions resulting from the prolonged misuse of the drug. The side effects of Valium (diazepam) addiction are listed below.
- Fatigue: The drug’s sedative effects suppress energy levels over time. Persistent fatigue often disrupts daily activities, resulting in difficulty concentrating or completing tasks. Fatigue additionally affects mood, resulting in withdrawal from social interactions or irritability.
- Dizziness: Regular Valium use causes dizziness, a side effect that worsens with continued misuse. Dizziness impairs balance and spatial awareness, increasing the risk of falls or accidents. Individuals feel disoriented or unable to focus, affecting performance at work or school. In severe cases, chronic dizziness limits mobility, leading to a more sedentary lifestyle.
- Impaired coordination: Long-term Valium use affects motor skills, causing clumsiness or poor coordination. Tasks requiring precision, such as driving or using machinery, become particularly challenging and potentially dangerous. Impaired coordination leads to injuries, affecting an individual’s independence and quality of life.
- Confusion: Confusion often arises as a cognitive side effect of long-term Valium use, leaving individuals feeling mentally foggy and disoriented. Difficulty in thinking clearly makes decision-making and everyday tasks challenging. Confusion tends to contribute to memory lapses as well, further compounding frustration.
- Aggressiveness: Valium addiction leads to episodes of aggressiveness, particularly as a result of mood swings and frustration when the drug’s effects wear off. Individuals often become more irritable, with a lower tolerance for stress or criticism, leading to unexpected outbursts. A 2004 paper by Mancuso et al., titled, “Paradoxical Reactions to Benzodiazepines: Literature Review and Treatment Options” included the case of a 28-year-old woman with a history of depression who displayed aggressive and abusive behavior towards her daughter following the administration of diazepam. The same patient, originally given diazepam for anxiety and mental distress, proceeded to experience aggressive fantasies and engaged in self-destructive conduct, including pounding her head against the wall.
- Skin rash: A skin rash develops in certain individuals addicted to Valium, potentially as an allergic reaction or side effect of prolonged use. Rashes appear as redness, itchiness, or small bumps on the skin, causing discomfort and irritation. The visible effects tend to impact self-esteem, especially if the rash appears in noticeable areas.
- Blurred vision: Valium addiction leads to blurred vision, making it difficult to see clearly or focus on objects. Suffering from blurred vision raises possible safety hazards by interfering with daily activities including reading, driving, or operating machinery. Affecting general quality of life, blurred vision often varies with dosage and gets worse with time.
How does Valium addiction impact mental health?
Valium addiction significantly impacts mental health, causing a number of mental problems that get worse over time. As the body grows dependent on the calming effects of Valium, prolonged abuse alters normal brain chemistry and causes mood swings, anxiety, and depressive symptoms.
Mental illness, such as heightened anxiety or depression, frequently arises as the brain struggles to function without the sedative influence of Valium, especially during periods of withdrawal.
This dependency makes individuals feel trapped, creating feelings of helplessness, irritability, and emotional instability. The toll on mental health often worsens the cycle of addiction, as individuals use Valium to temporarily escape the very distress it contributes to, making recovery even more challenging.
What are the causes of Valium addiction?

Causes of Valium addiction are the several elements and circumstances that allow people to become dependent on Valium. The causes of Valium addiction are listed below.
- Genetic predisposition: A genetic predisposition to addiction increases the likelihood of developing a dependency on Valium. Individuals with a family history of substance abuse are likely to inherit genetic traits that make them more vulnerable to addictive behaviors. Genetic predisposition influences brain chemistry, making certain people more susceptible to the calming effects of Valium and more likely to misuse it.
- Psychological factors: Psychological factors, such as chronic stress or anxiety, often drive individuals to misuse Valium to alleviate these feelings. The drug’s tranquilizing effects temporarily ease mental distress, creating a cycle where individuals rely on it to manage their emotions. Over time, the brain adapts to Valium’s presence, and without it, anxiety symptoms intensify, leading to further misuse.
- Environmental influences: Environmental influences, including family dynamics, peer pressure, or exposure to substance misuse, contribute to Valium addiction. Growing up in an environment where substance use is normalized shapes one’s attitude toward drugs like Valium, increasing the likelihood of misuse. Additionally, high-stress environments or lack of supportive relationships drive individuals to seek comfort in Valium’s calming effects.
- Long-term use: Long-term use of Valium, even when initially prescribed for legitimate medical reasons, leads to dependency as the body builds tolerance over time. Individuals usually find themselves needing higher doses to achieve the same relief, increasing the risk of addiction. Prolonged use disrupts natural coping mechanisms as well, creating a dependency that feels necessary to manage daily life.
- Self-medication: Self-medicating with Valium quickly leads to misuse, as individuals attempt to manage symptoms on their own, often without understanding the drug’s risks. Over time, the need for relief and lack of medical oversight increases the likelihood of addiction. Self-medication spirals into a dependency that makes it difficult to stop using the drug without professional help. A 2004 study by Divac et al., titled, “Benzodiazepines utilization and self-medication as correlates of stress in the population of Serbia” found that self-medication with benzodiazepines (BDZs) was evident, particularly during acute crises. The unrestricted sale of drugs in private pharmacies resulted in a significant number of individuals obtaining benzodiazepines over-the-counter. Diazepam has become the most frequently prescribed benzodiazepine, comprising 50-92% of all BDZ prescriptions and sales. This is likely due to the medication’s affordability and accessibility.
What are the risk factors for Valium addiction?
Risk factors for Valium addiction are attributes, traits, or influences raising a person’s probability of becoming dependent on Valium. The risk factors for Valium addiction are listed below.
- Impulsive personality traits: Individuals with impulsive personality traits are more likely to misuse Valium, as they are prone to making decisions without fully considering the consequences. A study titled, “Psychosocial characteristics of benzodiazepine addicts compared to not addicted benzodiazepine users” published in the January 2013 issue of the journal Progress in Neuro-Psychopharmacology & Biological Psychiatry revealed that compared to non-addicts, benzodiazepine addicts exhibited higher levels of neuroticism, introversion, and anxiety (both state and trait). Additionally, their conscientiousness scores were lower, suggesting a possible connection between these characteristics of personality and addiction susceptibility.
- Young age at first use: Starting Valium or other benzodiazepines at a young age increases the risk of addiction due to the ongoing development of the brain. Adolescents and young adults are especially vulnerable, as their brains are more impressionable and reactive to substances. Early exposure normalizes the use of prescription drugs to manage stress or anxiety, setting a pattern for future misuse.
- Medical prescription and tolerance: Individuals prescribed Valium for medical reasons, such as anxiety or muscle spasms, develop tolerance, leading to increased doses over time. This escalation results in dependence, as individuals feel they cannot function without the drug’s effects. Therefore, there is likelihood of a prescription evolving into an addiction if usage is not carefully monitored.
- Socioeconomic factors: Socioeconomic challenges, such as financial instability or lack of access to resources, increase the risk of Valium addiction as individuals seek relief from stress or hardship. A 2015 research article by Tvete et al., titled, “Risk factors for excessive benzodiazepine use in a working age population: a nationwide 5-year survey in Norway” indicated that those with lower household incomes and less education were more likely to use benzodiazepines excessively. The risk of excessive use was lower for individuals who worked in the public or private sectors than for those who did not have a registered job.
- Psychiatric comorbidities: Underlying mental health conditions, such as depression or post-traumatic stress disorder (PTSD), often increase the risk of Valium addiction. Individuals with these conditions tend to misuse Valium to manage symptoms that feel overwhelming, seeking temporary relief from persistent distress. This dependency complicates mental health further, as the drug disrupts natural emotional regulation over time.
How is Valium addiction diagnosed?
Valium addiction is diagnosed by utilizing a combination of diagnostic criteria for substance use disorders, behavioral assessments, and medical evaluation. A healthcare provider typically begins by assessing the patient’s medication history, including the dosage, frequency, and duration of Valium use.
Diagnostic criteria for sedative, hypnotic, or anxiolytic use disorder from the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) are often applied to identify an addiction to Valium. A thorough evaluation helps distinguish addiction from legitimate medical use and guides appropriate treatment.
What are the available treatments for Valium addiction?

Available treatments for Valium addiction are the several pharmacological, psychological, and support-based approaches meant to enable people to stop depending on Valium. The available treatments for Valium addiction are listed below.
- Detoxification: Detoxification, or detox, is often the first step in treating Valium addiction, aiming to eliminate the drug from the body under medical supervision. Gradual tapering is usually recommended, as abruptly stopping Valium leads to severe withdrawal symptoms, including seizures. Medical staff track the person during detox to manage symptoms and offer drugs to reduce discomfort. A supervised drug detoxification helps the person stabilize physically, therefore laying the groundwork for additional therapy.
- Cognitive behavioral therapy (CBT): Through addressing the underlying reasons for Valium misuse, cognitive behavioral therapy assists individuals in developing healthier coping mechanisms. Therapists assist patients in managing triggers, diminishing cravings, and enhancing resilience against relapse. CBT is frequently an effective instrument for sustained recovery, as it enables individuals to regulate addiction-related thoughts and actions.
- Inpatient rehabilitation programs: Inpatient rehab programs provide a structured environment for individuals to focus on recovery away from daily stressors and triggers. These programs provide intensive therapy and a supervised environment meant to limit access to drugs. Usually spanning a few weeks through several months, inpatient treatment offers a basis for long-term rehabilitation via diverse therapeutic activities.
- Outpatient care: Outpatient rehab programs allow individuals to receive treatment while continuing with their daily responsibilities, like work or school. These programs offer therapy sessions, group meetings, and medical support on a part-time basis, allowing flexibility in recovery. Outpatient rehab is often suitable for those with milder addiction or as a follow-up to inpatient treatment.
- Support groups: Support groups let people interact with others going through comparable challenges, therefore offering a community-based method of healing. Through providing a secure environment for experience sharing, accountability, and support, these groups lessen feelings of loneliness. In addition to offering perspectives from people who have effectively completed the recovery process, the group environment promotes a feeling of community.
When should you seek treatment for Valium addiction?
You should seek treatment for Valium addiction as soon as signs of dependency or misuse emerge, particularly if Valium use begins to interfere with daily life, responsibilities, or personal relationships.
Early signs, such as needing higher doses to achieve the same effect, experiencing cravings, or facing withdrawal symptoms when not using Valium, indicate that the body is likely already reliant on the drug.
If an individual finds it difficult to cut back on their own or feels anxious or distressed without Valium, professional support is able to provide the tools needed to regain control. Furthermore, indications that Valium use is causing one to overlook personal, professional, or educational commitments point to the negative effects of addiction on one’s mental and physical well-being.
Addressing Valium addiction promptly prevents it from worsening, making treatment more effective and enhancing the chances for long-term recovery.
Can Valium addiction be treated without medication?
Yes, Valium addiction can be treated without medication, though such an approach often depends on the individual’s specific needs and severity of addiction. This method is additionally more challenging and requires strong support systems.
Non-medication treatments include gradual tapering of Valium doses, where the amount is reduced over time to lessen withdrawal symptoms. This process, when combined with psychological therapies such as cognitive behavioral therapy (CBT), assists in the resolution of underlying issues that contribute to dependence.
People in recovery likewise benefit from other non-pharmaceutical methods that foster emotional stability and resilience, like support groups and lifestyle adjustments. Although addiction treatment medications ease withdrawal symptoms and reduce cravings for certain people, non-medicated treatments are viable and effective alternatives, especially for individuals with milder dependencies or those who prefer a drug-free approach.
However, for individuals with severe dependence or withdrawal risks, such as seizures, medical supervision is highly recommended, as it allows for close monitoring and intervention if needed.
Can alternative therapies prevent the need for Valium use?
Yes, alternative therapies can occasionally eliminate the need for Valium by offering safe, natural alternatives to treat anxiety, stress, and other issues that Valium usually treats. Without the use of drugs, people are able to manage their anxiety, lower their stress levels, and create coping mechanisms with the aid of practices like mindfulness meditation and cognitive behavioral therapy (CBT).
Through generating endorphins, which are naturally occurring stress relievers, physical activities like yoga and exercise are likewise beneficial for fostering relaxation and elevating mood. Additionally, lifestyle changes—such as establishing a regular sleep routine, practicing good nutrition, and avoiding stimulants like caffeine—reduce the need for sleep aids like Valium.
While these therapies do not fully replace Valium in all cases, especially for severe anxiety or other acute conditions, they are seen by certain individuals as valuable first-line options to address symptoms before considering medication.
How is Valium addiction prevented?
Valium addiction is prevented through cautious medical supervision, appropriate usage, and knowledge of the drug’s addictive qualities. Doctors typically prescribe Valium for short-term relief of acute symptoms, minimizing the risk of dependency through limited doses and duration.
It is possible for patients to play a role in prevention by following their doctor’s instructions precisely, avoiding dose increases or extended use without consultation. Informing individuals about the potential for tolerance and dependence serves to emphasize the significance of adhering to prescribed guidelines.
For those with anxiety or similar conditions, non-drug alternatives like therapy or relaxation techniques reduce reliance on Valium and lessen addiction risk. Along with regular assessments, good communication with healthcare professionals guarantees safe, efficient treatment and helps avoid misuse.
Can healthcare providers limit Valium prescriptions to prevent addiction?

Yes, healthcare providers can limit Valium prescriptions to prevent addiction by carefully managing dosage, duration, and patient education. According to a 2015 study by Jonathan Brett and Bridin Murnion titled, “Management of benzodiazepine misuse and dependence,” the abrupt cessation of a benzodiazepine is likely to result in withdrawal symptoms for any patient who has been taking it for more than 3–4 weeks.
Limiting prescriptions to a supply of 1–2 weeks helps minimize the risk of dependence. Before writing a prescription for Valium, doctors frequently consider a patient’s past substance use, mental health, and other risk factors.
In order to prevent long-term dependence on benzodiazepines, they are likely to recommend alternative therapies for treating anxiety or insomnia. Providers are able to keep an eye out for any indications of tolerance or abuse by providing clear instructions on how to take Valium properly and scheduling follow-up visits. Healthcare practitioners significantly lower the risk of addiction by restricting the prescription of Valium and offering advice on safe usage.

