Psychotic depression: definition, causes, symptoms, and treatments
Table of content
- What is psychotic depression?
- What are the causes of psychotic depression?
- What are the symptoms of psychotic depression?
- How is psychotic depression diagnosed?
- How to deal with psychotic depression?
- What are the available treatments for psychotic depression?
- What is the difference between psychotic depression and major depression?
- What is the difference between psychotic depression and schizophrenia?
Psychotic depression is a severe subtype of major depressive disorder distinguished by delusional thinking and hallucinations. Individuals experience intense sadness along with false beliefs, often reflecting feelings of guilt, worthlessness, or fear.
The causes of psychotic depression are genetic predisposition, neurochemical imbalances, hormonal fluctuations, psychological stress, and pre-existing mental health conditions.
The symptoms of psychotic depression include psychotic symptoms, mood disturbances, behavioral changes, cognitive impairment, physical symptoms, and social withdrawal.
The available treatments for psychotic depression are combination pharmacotherapy, electroconvulsive therapy (ECT), cognitive behavioral therapy (CBT), and immediate medical intervention.
What is psychotic depression?
Psychotic depression is a serious form of major depressive disorder (MDD) characterized by the presence of psychotic symptoms (hallucinations or delusions) occurring during a major depressive episode (otherwise known as depressive psychosis or major depression with psychotic features).
Major depressive disorder with psychotic features combines symptoms of severe depression with a disconnection from reality. Psychotic symptoms manifest as hallucinations (seeing, hearing, or feeling things that aren’t real) and delusions (false beliefs about what is happening or who one is). Delusions in psychotic depression often align with themes of guilt, worthlessness, and persecution.
Psychotic depression remains frequently underdiagnosed and undertreated despite its severity. The condition causes significant morbidity and mortality, requiring prompt medical intervention.
How common is psychotic depression?
Psychotic depression is relatively rare, as epidemiological investigations into the prevalence of psychotic depression in the community suggest the condition affects approximately four per 1,000 individuals in the general population, according to a 2013 paper by Anthony J. Rothschild, titled “Challenges in the Treatment of Major Depressive Disorder With Psychotic Features.”
The report additionally revealed psychotic depression has varying prevalence rates across different populations and settings. Among patients hospitalized for depression, approximately 25% (one in four) have psychotic features. The frequency is particularly high in older adults, with rates ranging from 24% to 53% in inpatient settings for people over age 60.
What are the causes of psychotic depression?
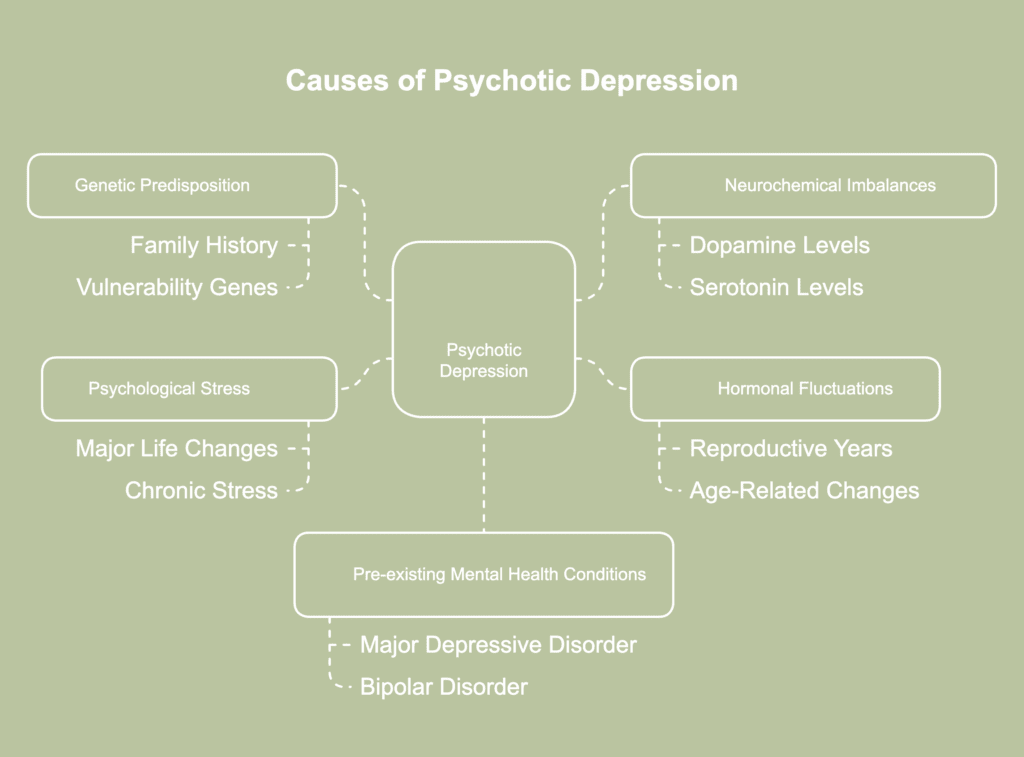
The causes of psychotic depression are a complex combination of various factors triggering severe depression with psychotic features. The causes of psychotic depression are listed below.
- Genetic predisposition: Family history plays a significant role in psychotic depression development. Specific vulnerability genes (BDNF, DBH, DTNBP1, DRD2, DRD4) increase the risk of psychotic symptoms, according to a 2013 study by Katharina Domschke, titled “Clinical and Molecular Genetics of Psychotic Depression.” Having a close relative with depressive psychosis or mental illness substantially raises an individual’s susceptibility.
- Neurochemical imbalances: Brain chemistry alterations, particularly in dopamine and serotonin levels, contribute to psychotic depression. Neurotransmitter imbalances affect mood regulation and reality perception. High cortisol levels have been specifically linked to the development of psychotic symptoms during severe depression.
- Hormonal fluctuations: Hormonal changes tend to trigger psychotic depression episodes. As per a 2021 review by Mazza et al., titled “Psychosis in Women: Time for Personalized Treatment,” changes in hormones during the reproductive years have an impact on dopamine systems. Due to protective hormonal influences (such as estrogens) during the reproductive years, women typically experience psychosis later than men. Age-related hormonal changes, particularly in older adults, contribute to vulnerability for psychotic depression.
- Psychological stress: Periods of extreme stress or trauma precipitate psychotic depression. Major life changes, disaster-related trauma, and chronic stress situations trigger the condition. Stress response affects brain chemistry and activates underlying genetic vulnerabilities.
- Pre-existing mental health conditions: Personal history of major depressive disorder or bipolar disorder increases psychotic depression risk. Previous psychotic illnesses or episodes create vulnerability for future psychotic depression. Schizoaffective disorder shares overlapping risk factors with psychotic depression.
Who is at risk for psychotic depression?
People at risk for psychotic depression include those who have a family history of psychosis, live alone, are unemployed, don’t regularly engage with friends, don’t have close confidants, or have a family history of mental illness and neurological abnormalities, as revealed in the findings of a 2016 paper by Heslin et al., titled “Biological and psychosocial risk factors for psychotic major depression.”
The study additionally found such social risk factors were more common in people with psychotic major depression (PMD) and schizophrenia, but had less of an impact on people with bipolar illness.
How to prevent having a psychotic depression?
To prevent psychotic depression, individuals must implement multiple evidence-based strategies. Psychotic depression prevention requires early recognition of warning signs and prompt medical intervention.
Mental health professionals recommend regular sleep patterns to maintain psychological stability. Medication adherence plays a crucial role in preventing psychotic depression recurrence. Social support systems help individuals maintain emotional stability and recognize early warning signs.
A 2010 research by Amminger et al., titled “Long-Chain -3 Fatty Acids for Indicated Prevention of Psychotic Disorders: A Randomized, Placebo-Controlled Trial” mentioned lω-3 polyunsaturated fatty acids (PUFAs) have potential as a safe and efficacious preventive measure for young people at ultra-high risk of psychosis.
This is attributable to the study findings demonstrating ω-3 PUFAs substantially minimized the risk of progression to full psychosis and enhanced symptoms and functioning in individuals with subthreshold psychosis.
Psychotic depression prevention connects directly to symptom recognition and management. Prevention strategies focus on maintaining mental wellness through multiple approaches, from medication adherence to lifestyle modifications.
What are the symptoms of psychotic depression?
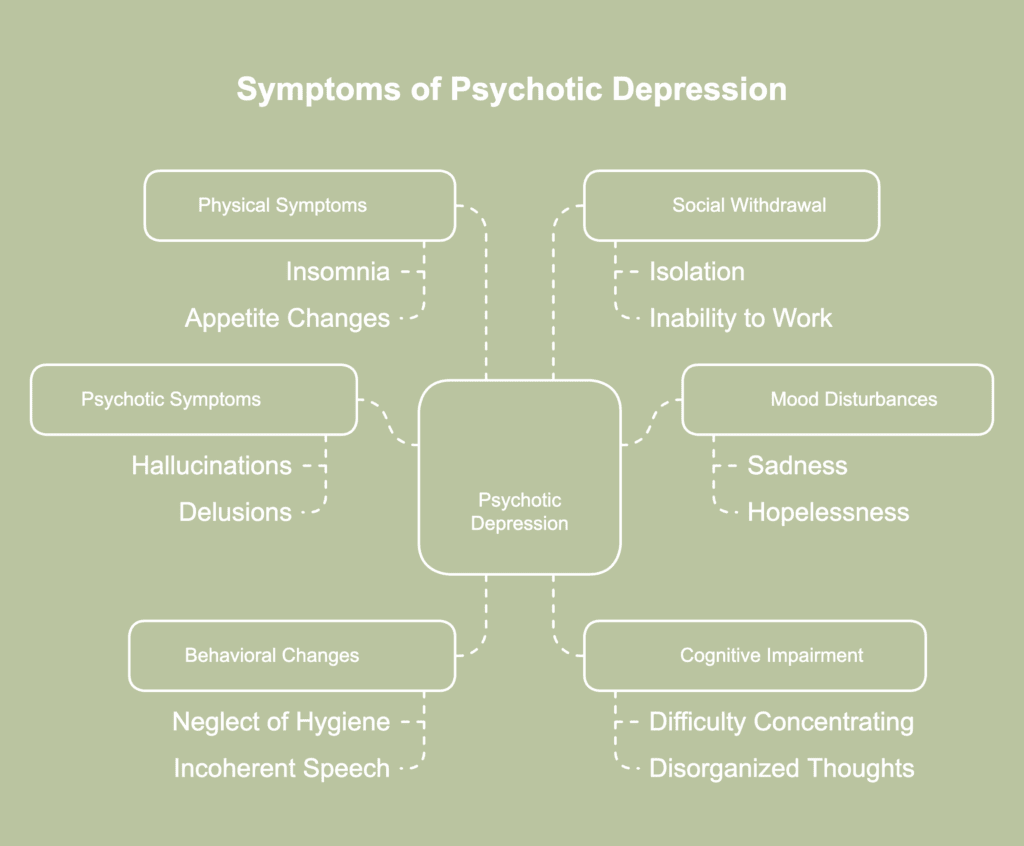
The symptoms of psychotic depression are a combination of severe depression symptoms and psychotic features including hallucinations and delusions. The symptoms of psychotic depression are listed below.
- Psychotic symptoms: Hallucination is a sensation, sight, or sound experienced without an external source or physical existence, while delusion manifests as false beliefs about reality. Common examples include hearing derogatory voices or having intense beliefs about personal worthlessness or guilt.
- Mood disturbances: Persistent feelings of sadness, hopelessness, and emptiness characterize the depressive component. Patients experience severe guilt, worthlessness, and complete loss of interest in previously enjoyed activities.
- Behavioral changes: Physical manifestations include staying in bed for extended periods, neglecting personal hygiene, and displaying unprovoked mood changes. Affected individuals often exhibit incoherent speech patterns and inappropriate situational responses.
- Cognitive impairment: Intellectual functioning becomes compromised, with patients showing difficulty concentrating and making decisions. The condition causes disorganized thoughts and inability to perform routine mental tasks.
- Physical symptoms: Physical symptoms include severe insomnia, agitation, anxiety, and constipation. Individuals frequently develop hypochondria and undergo notable shifts in appetite and weight.
- Social withdrawal: Complete disconnection from reality leads to severe social isolation. Sufferers withdraw from family and friends, often unable to maintain basic social interactions or work responsibilities.
How is psychotic depression diagnosed?
Psychotic depression is diagnosed through a comprehensive medical and psychological assessment performed by mental health professionals. The diagnostic process involves multiple sequential evaluation steps performed by qualified healthcare providers.
The mental health professional conducts an extensive patient interview to identify both depressive and psychotic symptoms. The diagnostic assessment examines the presence of persistent low mood, loss of interest in activities, and psychotic features like hallucinations or delusions.
A complete physical examination, including neurological testing, is conducted to rule out other medical conditions. Reviewing the individual’s full medical history, psychiatric background, and any family history of mental illness follows.
Symptom duration and severity are assessed using standardized tools by a mental health professional. For a diagnosis, symptoms must cause significant disruption to daily functioning and interpersonal relationships. The healthcare team distinguishes psychotic depression from other disorders like schizophrenia or bipolar disorder through differential diagnosis.
The diagnostic process for psychotic depression establishes the foundation for effective treatment planning. Mental health professionals use a comprehensive diagnostic approach to determine appropriate interventions.
How to deal with psychotic depression?
To deal with psychotic depression, patients require immediate professional medical intervention and structured treatment. Psychotic depression treatment combines antidepressant medication with antipsychotic drugs or electroconvulsive therapy.
Patients receive specialized care in hospital settings due to the condition’s severity. Psychotic depression management involves continuous medical monitoring and adjustment of treatment protocols.
The treatment process requires regular assessment of both depressive and psychotic symptoms. Professional healthcare providers monitor patients for potential side effects and treatment effectiveness.
When it comes to preventing recurrence following electroconvulsive therapy (ECT), pharmacotherapy—such as antidepressants or maintenance ECT—is more effective than a placebo, according to a 2021 study by Park et al., titled “Recent Updates on Electro-Convulsive Therapy in Patients with Depression.”
What can I expect from psychotic depression?
You can expect psychotic depression to bring intense feelings of sadness along with hallucinations or delusions distorting reality. Daily functioning often becomes difficult due to overwhelming emotional and psychological distress.
Patients are likely to struggle with severe guilt, paranoia, or irrational beliefs appearing entirely real. Appetite and sleep patterns often shift drastically, sometimes leading to weight loss or insomnia.
Social withdrawal is common, as connecting with others becomes increasingly challenging. Suicidal thoughts or behaviors potentially occur, requiring immediate medical attention.
What are the available treatments for psychotic depression?
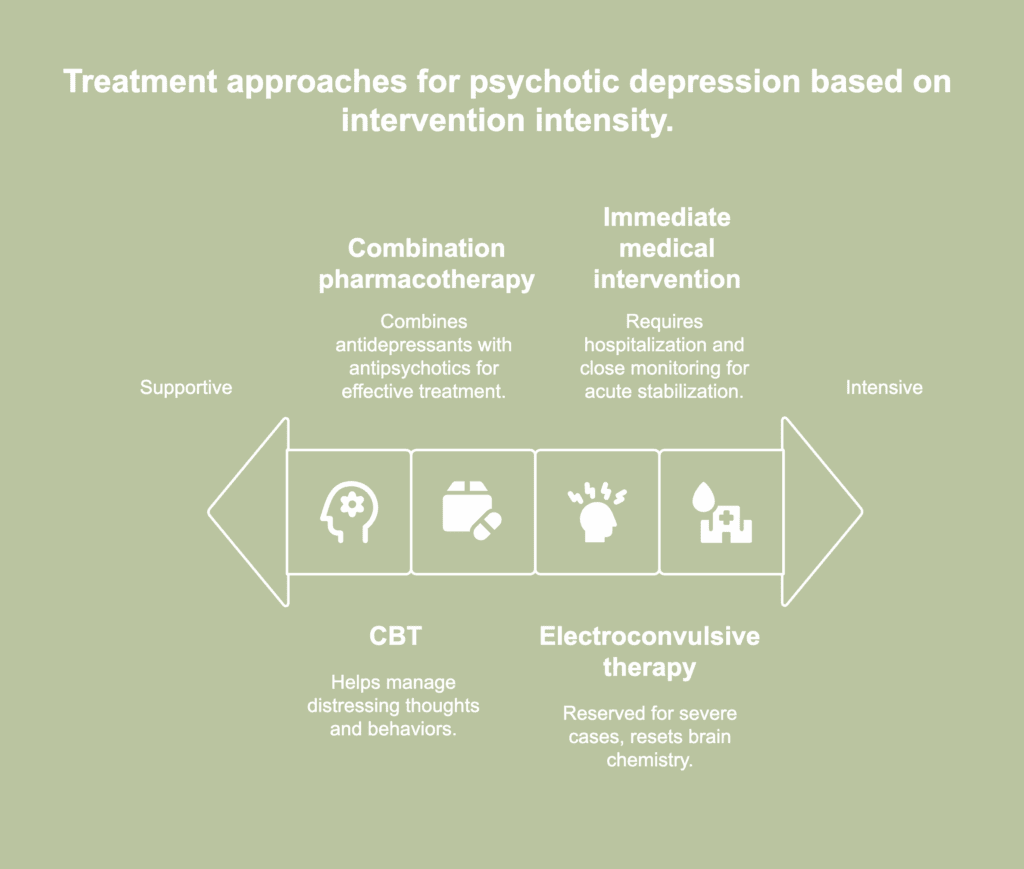
Available treatments for psychotic depression are medical and therapeutic methods meant to address the psychotic aspects of the disorder as well as its depressive symptoms. The available treatments for psychotic depression are listed below.
- Combination pharmacotherapy: First-line treatment combines antidepressants with antipsychotics. Specific medications for psychotic depression include sertraline and combinations of antidepressants with antipsychotics such as olanzapine or quetiapine. The most compelling evidence indicates the combination of an antidepressant and an antipsychotic is more effective than either medication alone or placebo in the treatment of psychotic depression, according to a 2021 review by Kruizinga et al., titled “Pharmacological treatment for psychotic depression.”
- Electroconvulsive therapy (ECT): ECT serves as a treatment option considered for severe cases or when other treatments are ineffective. The procedure involves delivering controlled electrical currents to the brain, triggering brief seizures believed to reset brain chemistry. As per a 2016 report by Anthony J. Rothschild, titled “Treatment for Major Depression With Psychotic Features (Psychotic Depression),” The American Psychiatric Association (APA) practice guidelines strongly endorse, with the highest level of clinical confidence, the treatment of psychotic depression with a combination of an antidepressant and an antipsychotic or electroconvulsive therapy.
- Cognitive behavioral therapy (CBT): CBT is used as a supportive treatment for psychotic depression. While medication remains the primary approach, CBT helps individuals manage distressing thoughts and behaviors that contribute to emotional instability. The approach teaches practical skills for challenging delusional beliefs and reducing the impact of negative thinking.
- Immediate medical intervention: Acute treatment requires hospitalization and close monitoring. The approach combines rapid medication administration with continuous assessment. Medical teams provide 24-hour supervision during initial treatment phases.
What are the complications of psychotic depression treatment?
The complications of psychotic depression treatment include an increased risk of suicide, medication side effects (particularly extrapyramidal symptoms and tardive dyskinesia from antipsychotics), treatment resistance, and potential medical emergencies requiring immediate intervention.
Treatment-resistant psychotic depression presents challenges in clinical management. First-generation antipsychotics pose particularly high risks for movement disorders and neurological complications.
Combination therapy with antidepressants and antipsychotics increases the potential for drug interactions and adverse effects. Such physical health complications often lead to treatment discontinuation and poor outcomes.
The risk of suicide remains elevated during treatment, especially in the early phases before medications take full effect. Hospitalization becomes necessary when patients experience severe symptoms or present immediate danger to themselves.
Electroconvulsive therapy (ECT), while effective, carries risks of memory problems and cognitive side effects. Chronic course and frequent relapses characterize various cases despite appropriate treatment.
Medical comorbidities complicate medication choices and treatment response. The extended duration of episodes and high recurrence rates lead to significant disability and mortality risk even with intervention.
What is the difference between psychotic depression and major depression?
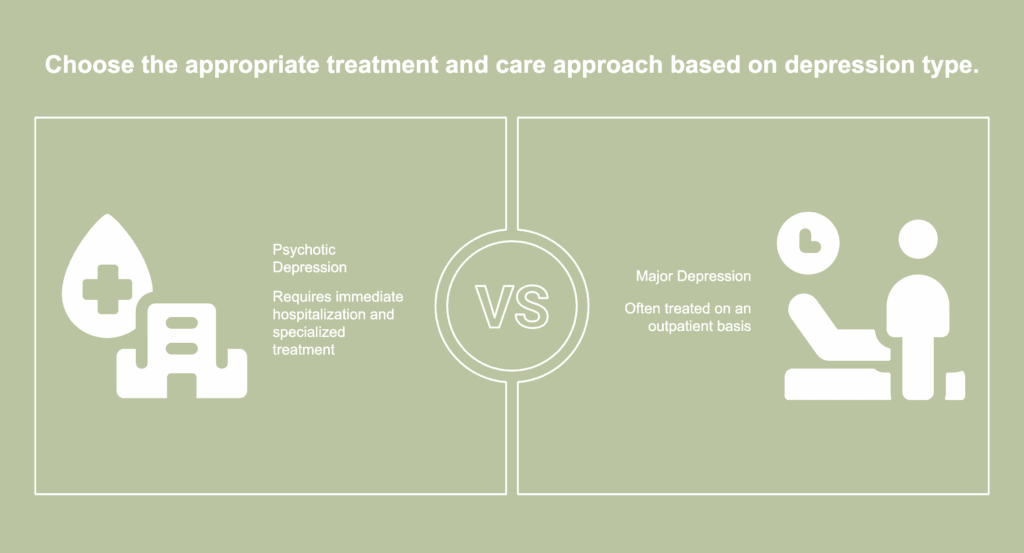
The difference between psychotic depression and major depression lies in the presence of psychotic features. The differences between psychotic depression and major depression are listed below.
- Severity and treatment setting: Psychotic depression requires immediate hospitalization due to the extreme severity of the condition, while major depression is often treated on an outpatient basis.
- Symptom presentation: Psychotic depression includes hallucinations and delusions during depressive episodes (like hearing voices or believing false realities), while major depression primarily involves mood symptoms without loss of reality testing.
- Clinical classification: Psychotic depression represents a distinct diagnostic subtype within major depressive disorder (MDD) according to the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5).
- Mortality risk: Psychotic depression carries remarkably higher morbidity and mortality rates compared to non-psychotic major depression, with increased suicide risk and more severe functional impairment.
- Treatment response: Psychotic depression shows greater treatment resistance and chronicity than standard major depression, requiring specialized interventions and longer recovery periods. The condition is frequently underdiagnosed and undertreated.
- Cognitive impact: Psychotic depression causes more severe cognitive disruption than major depression, affecting reality testing and requiring specialized cognitive function measurements through standardized assessments.
What is the difference between psychotic depression and schizophrenia?

The difference between psychotic depression and schizophrenia centers on the classification, symptoms, onset patterns, and treatment approaches. The differences between psychotic depression and schizophrenia are listed below.
- Classification and nature: Psychotic depression is a subtype of major depressive disorder (mood disorder) with psychotic features, while schizophrenia is a standalone psychotic disorder requiring six months of symptoms and functional decline for diagnosis.
- Symptom duration and pattern: Psychotic depression symptoms occur during depressive episodes and are episodic, while schizophrenia’s hallucinations and delusions tend to be relatively constant and persist for at least six months.
- Emotional expression: Patients with psychotic depression maintain the ability to show feelings and emotional expression, while schizophrenia results in diminished emotional expression and an inability to show feelings effectively.
- Biological markers: Patients with psychotic depression show distinct hypothalamic-pituitary-adrenal axis activity and unique all-night sleep electroencephalogram readings compared to schizophrenia patients.
- Functional impact: Psychotic depression requires hospitalization and has high morbidity but can be episodic, while schizophrenia causes persistent functional decline and requires long-term management.
- Treatment response: Psychotic depression responds to specific treatments for both depression and psychosis, while schizophrenia requires dedicated antipsychotic medication protocols and comprehensive psychiatric care.

