Food addiction: definition, symptoms, signs, causes, and treatment
Table of content
- What is food addiction?
- Why is food addictive?
- What are the symptoms of food addiction?
- What are the signs of food addiction?
- What are the causes of food addiction?
- What are the effects of overeating?
- What are the treatments for food addiction?
- What are the differences between food addiction and binge eating?

Food addiction is a behavioral condition defined by compulsive eating of appetizing meals, especially those heavy in fat, sugar and salt, even when doing so has a detrimental impact on one’s health and general well-being.
The symptoms of food addiction include intense cravings, withdrawal-like symptoms, secrecy and guilt, overindulging to the point of feeling sick, sleep problems, digestive disorders and decreased energy.
The signs of food addiction are frequently failing to establish rules, coming up with excuses, loss of interest in other activities, going out of the way to obtain unavailable foods, eating larger amounts than intended and inability to cut down.
The causes of food addiction include biological factors, psychological factors, social and environmental influences, food industry practices and cultural norms.
Treatment options for food addiction include cognitive behavioral therapy (CBT), 12-step programs, medications, nutritional counseling and lifestyle modifications.
What is food addiction?
Food addiction describes an obsessive and uncontrolled urge to eat, frequently motivated by pleasure rather than hunger. People with the condition have cravings, loss of control and ongoing intake despite negative effects, similar to the indicators of substance use disorders.
Highly palatable foods, rich in carbohydrates, sugar, fat and salt, are big contributors to the reinforcement of addictive eating behaviors. Persistent urges reflect an inability to manage eating once exposure to flavor-dense food begins.
Processed options loaded with carbohydrates create quick sensory pleasure and drive repeated consumption. Heavy sugar content boosts interest in every bite due to rapid shifts inside reward circuits.
Rich fat profiles extend fullness for a short span yet spark stronger interest once the feeling fades. High salt content enhances flavor intensity and keeps attention fixed on preferred food choices.
Even in the absence of actual hunger, individuals reach for highly tempting food for comfort or enjoyment. Ongoing exposure reshapes brain chemistry, creating tougher conditions for control over eating patterns along with stronger urges.
Why is food addictive?
Food is addictive because the reward system reacts strongly to certain ingredients. The brain registers a surge of excitement once a person consumes items engineered for strong sensory pull.
Formulas loaded with refined carbohydrates deliver quick energy shifts, triggering rapid reinforcement. Such reactions light up key pleasure centers, prompting repeated interest in the same types of food.
A 2021 review by Ashley N. Gearhardt and Erica M. Schulte titled “Is Food Addictive? A Review of the Science” explained how the “dietary evolutionary mismatch” idea proposes an inherited drive for dense fuel sources during scarcity, with early humans relying on nuts or meats while reward circuits such as the mesolimbic dopamine pathway pushed motivation.
Protective signals limiting intake worked slowly, as seen with leptin responses. Modern ultraprocessed products exploit that vulnerability through heavy refinement, rapid absorption, minimal fiber and flavor-boosting additives, creating intake levels far beyond normal energy requirements and promoting weight gain.
Parallels with addictive drugs appear as both involve turning natural materials into highly potent forms, such as fermenting fruit for wine or refining corn for high-fructose syrup. Faster delivery intensifies reinforcing effects, evident when comparing smoking nicotine to chewing tobacco leaves or consuming soft foods engineered to dissolve instantly. Neither category supports survival needs, and excessive use harms health.
Repeated exposure to artificially stimulating foods leads to dopamine addiction, though the dependence stems more from the act of consuming rewarding foods than from dopamine itself. The brain seeks pleasurable experiences linked to appetizing meals, reinforcing compulsive eating and overriding natural hunger cues.
What are the symptoms of food addiction?

Symptoms of food addiction include noticeable indicators seen in individuals overindulging in highly appetizing foods despite harmful effects. The symptoms of food addiction are listed below.
- Intense cravings: Individuals with food addiction often feel intense urges to eat specific foods. Cravings arise even without physical hunger and typically focus on highly palatable options. A key finding of a 2020 study by Adrian Meule titled “The Psychology of Food Cravings: the Role of Food Deprivation” distinguished cravings from hunger: hunger signals a general need for nourishment satisfied by any food, whereas cravings are intense, specific urges unrelated to fullness. In a laboratory study on chocolate, craving intensity linked to hunger but not deprivation duration, and only craving predicted greater salivation and intake during exposure. The findings highlighted how cravings emerge independently of physiological need, supporting psychological explanations.
- Withdrawal-like symptoms: Reducing or eliminating certain foods triggers withdrawal-like symptoms. The likelihood of relapse is increased by such effects associated with avoiding addictive foods. A qualitative study cited in a review by Parnarouskis et al., titled “Withdrawal: A key consideration in evaluating whether highly processed foods are addictive” published in November 2022 highlighted parents’ perceived obstacles to lowering children and adolescents’ sugar-sweetened beverage consumption. Parents reported withdrawal-like reactions in children, such as headaches, increased moodiness, and social withdrawal, when attempts were made to limit consumption.
- Secrecy and guilt: Affected individuals eat in secret to conceal the unhealthy relationship with food from others, feeling ashamed or guilty about eating habits. Keeping meals hidden fosters isolation and intensifies emotional distress. The guilt associated with overeating perpetuates the cycle of addiction, as individuals tend to eat more to cope with negative emotions.
- Overindulging to the point of feeling sick: Individuals addicted to food consume large quantities, leading to physical discomfort. Excessive consumption harms overall health, triggering digestive problems and significant bodily stress. Compulsive eating continues despite negative effects, reflecting a loss of control. The cycle reinforces as cravings intensify after periods of restriction.
- Sleep problems: Sleep problems emerge as a symptom of food addiction when excessive amounts of sugar and refined carbohydrates disrupt natural energy cycles. Irregular eating patterns and nighttime cravings interfere with falling asleep and maintaining restorative rest. As per a 2021 study by Vernia et al., titled “Sleep disorders related to nutrition and digestive diseases: a neglected clinical condition,” stimulants such as coffee, cola, tea, chocolate and spices disrupt sleep. Alcohol, a strong depressant, interferes with the circadian clock and reduces sleep quality. Spicy or hot foods are linked to insomnia. Irregular meal timing and frequent snacking desynchronize circadian rhythms, impair metabolism and promote weight gain.
- Digestive disorders: Bloating, flatulence, abdominal pain and irregular bowel movements are among the digestive issues resulting from the condition. Consuming highly processed and refined foods lacking fiber and essential nutrients contributes to gastrointestinal discomfort and dysfunction. Overeating during episodes of compulsion further strains the digestive system, slowing transit and increasing inflammation.
- Decreased energy: Food addicts experience energy fluctuations during the day, marked by periods of lethargy and fatigue. Nutritional deficiencies from a diet high in processed foods and low in essential nutrients, along with unstable blood sugar levels from frequent sugar intake, contribute to shifts in one’s energy level. Overeating of high-calorie, low-nutrient foods forces the body to expend extra energy on digestion, leaving less available for daily activities.
What are the signs of food addiction?

Signs of food addiction are outward manifestations indicating an individual is grappling with a compulsive and obsessive attachment to eating. The signs of food addiction are listed below.
- Frequently failing to establish rules: People with food addiction struggle to follow self-imposed rules regarding eating habits. Setting boundaries or guidelines becomes challenging, leading to repeated setbacks. An inability to maintain control fosters feelings of helplessness. Even with strong intentions, individuals repeatedly ignore limits on portion sizes or certain foods, strengthening habitual overconsumption. Such repeated breaches erode confidence in self-control and intensify reliance on immediate gratification.
- Coming up with excuses: Affected individuals make excuses to justify eating behaviors. Rationalizations enable one to steer clear of guilt and maintain the cycle of addiction. Excuses involve blaming external factors, such as stress, social events or lack of time, for overindulgence. The justifications allow repeated consumption of high-calorie or processed foods without accountability.
- Loss of interest in other activities: As addiction worsens, individuals lose interest in previously enjoyable activities, choosing instead to eat or constantly think about food. Diverting attention from significant experiences adversely affects personal relationships, impairs professional performance and decreases general quality of life. Over time, social isolation and declining productivity reinforce dependence on food for comfort.
- Seeking hard-to-find foods: Individuals take significant measures to obtain preferred items even when unavailable. The intense drive leads to visiting multiple stores, overspending or bending rules to secure high-reward foods. Extensive efforts highlight the compulsive nature of the addiction and the prioritization of cravings over practical considerations. Persistent focus on acquiring foods disrupts routines and social responsibilities, reflecting the strong hold of the condition.
- Eating larger amounts than intended: A hallmark of food addiction is consuming much more than initially planned. Despite setting limits or resolving to eat smaller portions, individuals exceed boundaries. Overeating occurs even when already full, driven by strong cravings or irresistible food cues.
- Inability to cut down: Individuals with food addiction cannot control consumption, even after recognizing its harmful effects. Efforts to reduce portions or avoid specific foods repeatedly fall short. The strong drive to eat certain items overrides intentions and rational decision-making. An ongoing conflict between desire and intention keeps individuals trapped in unhealthy eating practices.
How is food addiction diagnosed?
Food addiction is diagnosed by observing core diagnostic criteria primarily derived from the Yale Food Addiction Scale (YFAS) and are largely extrapolated from substance use disorders (SUDs) in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5).
Core criteria for diagnosing food addiction include eating larger quantities or for longer than intended, persistent preoccupation with food, cravings for specific items like high-fat or sugary foods and continued consumption despite negative health or social consequences.
A diagnosis requires meeting at least three criteria along with evidence of significant impairment or distress within the past year, similar to standards used for SUDs, according to a 2022 paper by Octavian Vasiliu titled “Current Status of Evidence for a New Diagnosis: Food Addiction-A Literature Review.”
A mental health professional or healthcare provider frequently conducts a comprehensive evaluation of an individual’s dietary practices, behaviors and psychological symptoms as part of the diagnostic process.
The evaluation comprises clinical observations, interviews and self-reported questionnaires to ascertain the presence and severity of addictive feeding patterns. Clinicians additionally take into account things like the person’s level of distress, functional impairment and how much eating interferes with day-to-day activities.
What are the causes of food addiction?
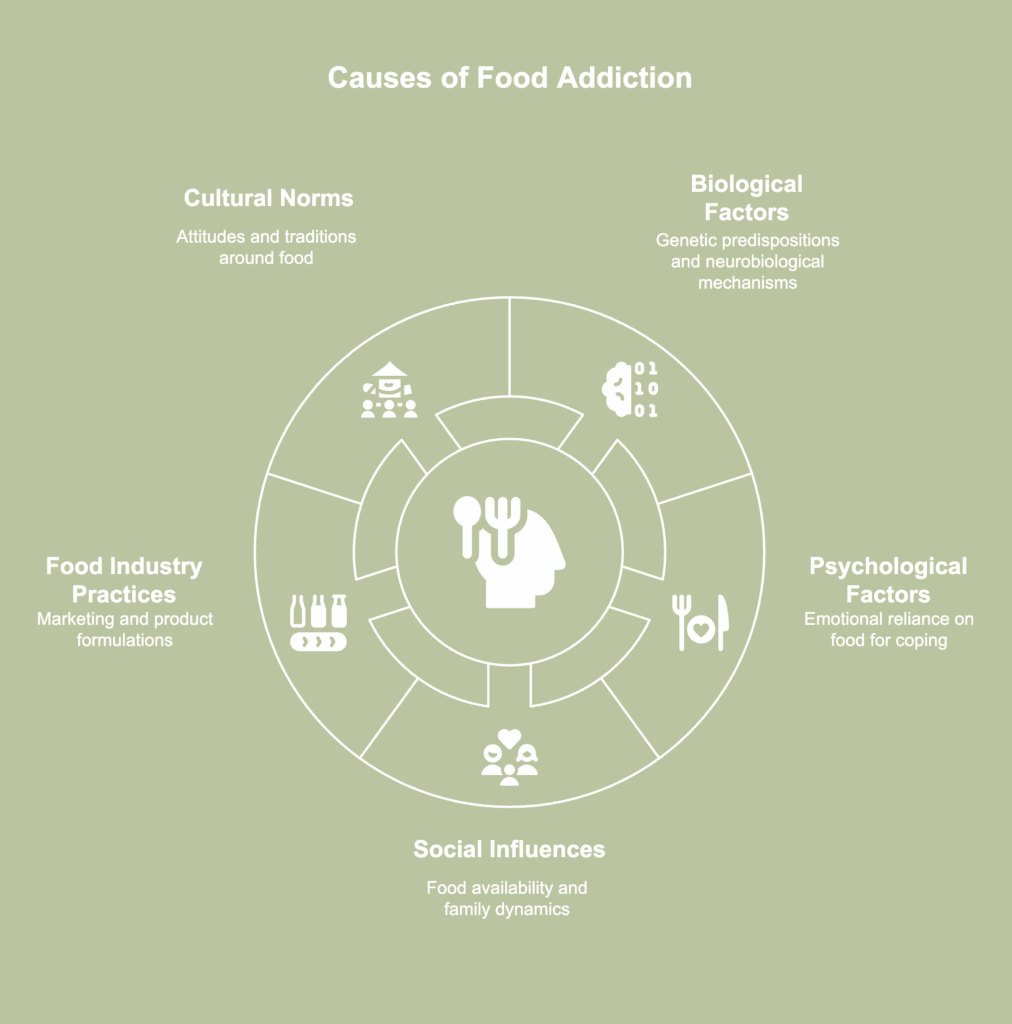
Causes of food addiction describe the fundamental elements leading to compulsive overeating and reliance on extremely appetizing meals. The causes of food addiction are listed below.
- Biological factors: Genetic predispositions and neurobiological mechanisms contribute to food addiction. As per a 2020 review by Wiss et al., called “Food Addiction and Psychosocial Adversity: Biological Embedding, Contextual Factors, and Public Health Implications,” adolescents exposed to early life adversity (ELA) often have larger pituitary glands and exhibit a lower cortisol response upon waking, suggesting reduced efficiency of the hypothalamic-pituitary-adrenal (HPA) axis due to chronic stress. Variations in corticotrophin-releasing hormone (CRH) contribute to increased vulnerability to stress. Individual differences in inflammatory responses help explain why stress affects people differently, sometimes causing neuroinflammation through pro-inflammatory cytokines. Diets high in pro-inflammatory foods, such as those rich in saturated fats, further increase neuroinflammation in brain regions associated with reward, leading to unhealthy eating/obesity.
- Psychological factors: Psychological factors contribute to food addiction by linking eating with coping mechanisms for stress, anxiety or negative emotions, creating a pattern of emotional reliance on food. Findings of a 2020 paper by Kircaburun et al., titled “Measurement, prevalence, and psychological risk factors associated with addictive food consumption: Development of a new food addiction scale and evidence from a national largescale sample” showed psychological conditions such as psychiatric symptoms, difficulty identifying emotions (alexithymia), strong negative or positive emotions and anxious attachment contribute to addictive eating behaviors, independently of sociodemographic factors. Additionally, males, younger individuals, those with lower education levels and people who consume alcohol face a higher risk of developing food addiction.
- Social and environmental influences: Social and environmental factors, including food availability, family dynamics and peer influences, play an important role in shaping eating behavior and eventual food addiction. The availability of highly processed and highly palatable meals is one of the societal elements contributing to the normalization of overeating and compulsive eating behavior. An individual’s relationship with food is additionally affected by family upbringing and dynamics, including parental feeding practices and modeling of eating behaviors.
- Food industry practices: Marketing strategies, product formulations and manufacturing practices employed by the food industry all contribute to the addictive properties of specific foods. Ultra-processed and processed foods are designed to be highly palatable by incorporating specific flavors, textures and additives to increase appeal and addictive potential. The consumption of unhealthy meals is further encouraged by marketing strategies like product placement and targeted advertising.
- Cultural norms: Cultural attitudes surrounding food consumption influence individuals’ perceptions, behaviors and susceptibility to food addiction. Cultures emphasizing food during social gatherings and celebrations tend to normalize overeating, fostering addictive eating habits. Shared rituals and traditions around indulgent meals sometimes make moderation feel unusual or even socially uncomfortable. Family or community expectations around finishing large portions override natural hunger signals.
How do genetics affect food addiction?
Genetics affect food addiction by influencing how the brain responds to food stimuli. Differences in genes regulating hormones involved in appetite and reward, such as leptin and ghrelin, alter feelings of hunger and satiety.
Certain individuals inherit heightened sensitivity to rewarding foods, increasing the likelihood of overeating. Variations in taste receptor genes additionally shape preferences for high-fat, high-sugar or salty foods, guiding eating behaviors from an early age.
An August 2025 study by Carbone et al., called “Understanding food addiction in obesity: a genetic perspective” examined whether genetic differences in the MC4R gene, which regulates eating behaviors and food reward, are associated with food addiction (FA) in individuals with obesity.
Among patients with FA, C allele carriers additionally exhibited increased anxiety and depression relative to T allele carriers. In summary, the MC4R gene variant rs17782313 (C allele) is linked to food addiction and worsened mental health outcomes in people with obesity.
Are there demographic differences for food addiction?
Yes, there are demographic differences for food addiction, and a 2024 paper by Bozkurt et al., titled “Factors affecting food addiction: emotional eating, palatable eating motivations, and BMI” documented a 3.18-fold increase in FA risk for women. Multiple investigations cited in the study reported higher prevalence in women as well.
In a 2021 study by Güngör et al., titled “The Relationship of Food Addiction With Other Eating Pathologies and Impulsivity: A Case-Control Study,” FA appeared 6.7 times more prevalent in women than in men. The report proposed several contributing factors.
Stronger tendencies toward comfort-driven intake played a role, along with intense pressure linked to diet trends and body ideals. Another factor involved a greater willingness among women to report FA indicators during assessments.
Moreover, a 2021 study by Carr et al., titled “Examining Impairment and Distress from Food Addiction across Demographic and Weight groups” reported a greater likelihood of FA-related distress or functional disruption in individuals living with obesity compared to people in normal-weight or overweight ranges. Findings pointed to stronger psychological strain linked to internalized stigma along with persistent weight-related bias.
Can depression cause food addiction?
Yes, depression can cause food addiction. Depressive symptoms often push individuals toward highly palatable food as a form of self-soothing, activating reward pathways and offering brief relief from inner strain. Comfort-driven eating gradually turns into a habitual response, reinforcing compulsive use of sugary or fatty products.
A 2020 study by Mills et al., titled “Overeating and food addiction in Major Depressive Disorder: Links to peripheral dopamine” assessed 140 participants and reported nearly 29% of individuals with major depressive disorder (MDD) met food-addiction criteria based on the Yale Food Addiction Scale (YFAS).
The figure surpassed estimates observed in wider community samples. Compared to control groups and participants without FA, individuals dealing with both conditions displayed stronger urges to eat for comfort, stricter dietary restraint and heavier depressive symptom loads.
What are the foods that can trigger food addiction?

Foods that can trigger food addiction refer to specific types of foods with the potential to cause compulsive and uncontrollable eating behaviors. The most common foods that can trigger food addiction are listed below.
- Chocolate: Chocolates with high sugar and milk content promote food addiction and chocolate addiction through a potent mix of sweetness and fat. Compared to various other snacks, chocolate triggers a distinctive pattern of brain activity, activating neural circuits tied to strong pleasure responses, as noted in a study by Casperson et al., titled “Increasing Chocolate’s Sugar Content Enhances Its Psychoactive Effects and Intake” published in March 2019.
- Potato chips: Potato chips create strong cravings due to high fat and salt levels. Overconsumption is more likely to occur due to the increased allure caused by the crunch and flavor enhancers. Widespread availability and ease of access perpetuate compulsive eating by encouraging habitual consumption.
- Ice cream: The combination of sugar and fat in ice cream produces an intense sensory pull overwhelming normal satiety signals. The cold, creamy texture strengthens reward responses toward food stimuli, creating a strong drive for repeated eating. In a 2023 paper by Leung et al., called “Food Insecurity and Food Addiction in a Large, National Sample of Lower-Income Adults,” ice cream ranked fifth among adults experiencing food insecurity, with 29.6% identifying it as a problematic item. In contrast, ice cream held the top position among adults with food security, with 24.7% reporting it as the most difficult item to manage.
- Pizza: Pizza triggers strong cravings because the combination of fat, salt and carbohydrates produces highly rewarding sensory effects. The melted cheese and flavorful toppings produce a comforting and indulgent eating experience. Pizza’s appealing texture and intense flavor make it easy to consume in large amounts, contributing to overconsumption.
- French fries: French fries remain widely available in fast food chains and restaurants, making access effortless. Consumption on a consistent basis intensifies cravings, promoting an overindulgence and an increasing preference for fatty, salty dishes. As per a 2018 article from Joel Fuhrman titled “The Hidden Dangers of Fast and Processed Food,” fried foods from fast food restaurants are typically prepared in oil heated and reused multiple times. A single serving of French fries from such outlets contains aldehyde levels 100 times higher than the limit considered safe by the World Health Organization (WHO).
- Cookies: Cookies contain a concentrated combination of sugar, fat and soft textures encouraging repeated bites. The sweet aroma and crunchy or chewy consistency enhance the overall eating experience, reinforcing habitual consumption. Continual indulgence causes reliance on cookies for comfort or reward. Small portions and convenient packaging allow consumption of large amounts without noticing.
- Soda: Sugary drinks such as soda contain high levels of refined sugar and caffeine, promoting food addiction and sugar addiction. Rapid absorption of sugar causes blood glucose to spike and then drop, creating repeated cycles of cravings. Carbonation adds a sensory appeal to soda.
What are the effects of overeating?

Effects of overeating describe the range of adverse outcomes resulting from eating past the point of fullness and in excess of the body’s nutritional and caloric requirements. The effects of overeating are listed below.
- Weight gain and obesity: Consistently consuming more calories than the body requires leads to excess energy stored as fat, causing weight gain. Fat builds up over time and eventually develops into obesity, a disorder characterized by an unhealthful rise in body weight. Numerous health issues, including diabetes, metabolic problems and heart disease, are made more likely by obesity.
- Digestive discomfort: Fast eating delays the sensation of fullness, leading to increased food consumption and a higher likelihood of overeating. Hedonic eating showed a strong link with recurring digestive discomfort across several symptoms, as noted in a 2023 paper by Ghusn et al., titled “Association Between Food Intake and Gastrointestinal Symptoms in Patients With Obesity.” Individuals who relied on food for pleasure experienced frequent abdominal pain, shifts in stool patterns and repeated bloating episodes. Meal-related upper abdominal pain appeared more often, and many reported a persistent sense of fullness after eating. Regular nausea additionally emerged as a common complaint among persons with pronounced hedonic eating tendencies.
- Type 2 diabetes: Overeating, particularly foods rich in sugar and carbohydrates, contributes to insulin resistance, reducing the body’s ability to respond effectively to insulin. As a result, blood sugar levels remain elevated, increasing the likelihood of developing type 2 diabetes. Persistent insulin resistance forces the pancreas to produce more insulin, eventually leading to pancreatic strain and a decline in insulin production. Without intervention, long-term effects include cardiovascular complications and nerve damage.
- Mental health issues: Overindulging impairs mental health by resulting in feelings of shame, remorse and low self-esteem. Distress sets off a vicious cycle where individuals keep eating to deal with emotional problems, deteriorating psychological health. Furthermore, physical repercussions like weight gain exacerbate issues with body image and raise the likelihood of anxiety and depression. Making the decision to stop compulsive eating is made more difficult by emotional suffering associated with unhealthy eating practices.
- Heart disease: Chronic overeating, particularly of foods high in saturated fats, trans fats and cholesterol, increases the risk of developing heart disease. According to a 2022 article by Basdeki et al., titled “Late-Night Overeating or Low-Quality Food Choices Late at Night Are Associated with Subclinical Vascular Damage in Patients at Increased Cardiovascular Risk,” more than 40% of daily calorie intake after 19:00 hours was associated with an increased risk of carotid plaques, a sign of vascular impairment. Arterial stiffness was higher among late-night eaters who ate unhealthy meals like wine, red meat and refined grains.
- Impaired brain function: Overconsumption of food, particularly foods high in fat and sugar, causes inflammation in the brain, affecting cognitive abilities. When calorie consumption is excessive, blood sugar levels rise and fall, impairing mental clarity and memory. As a result, decision-making skills deteriorate and the brain’s capacity to comprehend information is reduced.
What are the treatments for food addiction?
Treatments for food addiction refer to interventions employed with the goal of assisting patients in developing healthier relationships with food. The treatments for food addiction are listed below.
- Cognitive behavioral therapy (CBT): The primary objective of CBT is to identify and modify maladaptive beliefs and behaviors associated with food and eating. According to a 2024 review by Glenn Waller and Jessica Beard, “Recent Advances in Cognitive‑Behavioural Therapy for Eating Disorders (CBT‑ED),” evidence supports the effectiveness of cognitive-behavior therapy for eating disorders (CBT-ED) across individual sessions, group programs and guided self-help formats. Core strategies involve helping patients revise inaccurate emotional and cognitive reactions to food along with addressing body-image concerns. Guided self-help has shown strong outcomes for binge-eating disorder. Digital delivery has gained momentum with solid support for guided and unguided formats, and online access expands treatment reach in underserved regions or during pandemics.
- 12-step programs: 12-step programs, such as Overeaters Anonymous (OA), create a community of individuals experiencing food addiction. With the help of others who have conquered addiction, group members talk about difficulties without worrying about being judged. Support groups often adhere to a structured framework, like the 12-step model, designed to guide recovery.
- Medications: Certain medications are prescribed to help manage food addiction by regulating appetite and addressing co-occurring mental health issues. Drugs like naltrexone and bupropion have been used to reduce cravings and compulsive eating behaviors. A 2021 paper by Leary et al., titled “Current Intervention Treatments for Food Addiction: A Systematic Review” reported several medication-based approaches in adults that produced notable drops in FA symptoms or a shift in diagnosis, including a regimen combining naltrexone with bupropion. One study showed naltrexone paired with bupropion reduced FA severity and altered diagnostic outcomes in adults with obesity and comorbid binge eating disorder.
- Nutritional counseling: Working with a certified dietitian or nutritionist helps people create a balanced and nutritious eating plan customized to particular needs. Nutritional counseling imparts knowledge on portion control, nutrient-rich meals and meal planning, hence diminishing dependence on addictive foods.
- Lifestyle modifications: Managing food addiction is best accomplished by making all-encompassing lifestyle modifications. Healthy changes include developing regular sleeping routines, reducing stress by means of yoga or meditation and building social networks for emotional support. Breaking the cycle of FA calls for a balanced living including exercise and a diet.
How to overcome food addiction?
Overcoming food addiction starts with careful tracking of daily eating habits to reveal patterns linked to mood, timing and quantity. Stress management through grounding techniques or brief relaxation routines reduces impulsive eating driven by tension.
A quick internal check before reaching for food helps distinguish genuine hunger from habit or discomfort. Support from trusted individuals or structured programs strengthens accountability. Purposeful activities such as short walks or creative tasks redirect attention away from urges tied to monotony.
Removal of highly tempting items from one’s immediate surroundings reduces impulsivity and supports steadier decision-making. Balanced eating including satisfying options prevents rebound cravings fueled by strict restriction. Nutritious snacks stored within easy access points encourage healthier eating practices and support long-term control.
Is food addiction hard to break?
Yes, food addiction is hard to break. Unlike alcohol or drugs, food is essential for survival, making complete avoidance impossible. Cutting back on highly palatable foods is not as straightforward as eliminating substances like alcohol, since food remains a constant presence in daily life.
Feelings of depression, anxiety or stress further complicate recovery, as negative emotions lead to overeating. Various processed foods are designed to trigger cravings, reinforcing compulsive eating and making moderation challenging.
Shifting attention toward unprocessed foods supports better appetite control because flavors remain less engineered for overstimulation. Consistent inclusion of healthier foods provides a more predictable eating rhythm and reduces reliance on hyper-sweet or heavily seasoned items.
How long does it take to break food addiction?
The time it takes to break food addiction varies greatly among individuals and depends on the severity of the addiction, the presence of underlying emotional or psychological issues and the individual’s commitment to change.
For certain people, notable improvement becomes evident within a few months of dedicated effort, especially when guided by healthcare professionals and structured treatment plans. Others require a year or more to completely break free from the addiction and develop sustainable, healthier eating habits.
For food cravings, the first week brings pronounced discomfort as the body adjusts to new routines and eating foods with fewer stimulants. Within roughly four weeks, urges tend to soften, giving individuals room to follow new routines with less internal pushback.
Is food addiction treated in a rehab?
Yes, food addiction is treated in a rehab. Numerous treatment centers recognize addiction to food as a serious issue and offer specialized programs similar to those designed for behavioral addictions.
The majority of programs treat addiction holistically, emphasizing both the psychological and physiological components of the condition. Therapy, nutritional counseling and structured meal planning help individuals regain control over eating habits and develop healthier relationships with food.
Individuals in a food addiction rehab receive expert medical and psychological assistance, as well as regulated meal plans, nutritional advice and therapy sessions. A treatment facility provides a safe environment where patients develop beneficial routines without exposure to triggers.
What are the over-the-counter medications for food addiction?
There are currently no over-the-counter medications specifically approved for treating food addiction. However, certain supplements and over-the-counter (OTC) products aid in managing symptoms of food addiction or promote overall health during recovery. Examples include 5-HTP (5-Hydroxytryptophan) and chromium picolinate.
As per a 2024 review by Krupa et al., titled “Food Addiction,” serotonin (5-hydroxytryptamine; 5-HT) plays a key role in regulating appetite and curbing excessive food consumption. Lower serotonin levels have been linked to compulsive behaviors and mood disturbances, such as depression, which contribute to addictive eating.
Supplements like 5-HTP, an OTC precursor to serotonin, help restore serotonin balance, supporting appetite regulation and potentially reducing urges associated with food addiction.
Another supplement thought to help with weight loss and enhance nutrient metabolism is chromium picolinate. Chromium is an essential micronutrient involved in carbohydrate metabolism and plays a key role in insulin function, according to a 2015 study by Brownley et al., called “Dietary Chromium Supplementation for Targeted Treatment of Diabetes Patients with Comorbid Depression and Binge Eating.”
Its ability to influence insulin, dopamine and serotonin pathways makes chromium a potential therapy for individuals with type 2 diabetes who additionally struggle with depression and binge eating.
What are the symptoms of food withdrawal?

Symptoms of food withdrawal are the physical and psychological reactions experienced when an individual reduces or eliminates consumption of foods showing addictive effects. The symptoms of food withdrawal are listed below.
- Intense cravings: Intense cravings characterize food withdrawal, driven by the body’s strong desire for familiar addictive foods. Visual cues, aromas or stressful situations frequently spark urges, making resistance challenging. Recurrent cravings are important to the study of food addiction due to a link with compulsive eating, higher body mass index (BMI) and increased food intake, as noted in a 2019 study by Adams et al., titled “Food Addiction: Implications for the Diagnosis and Treatment of Overeating.”
- Irritability: When withdrawing from addictive foods, numerous people experience irritability and mood swings due to the sudden lack of comforting effects appetizing foods provide. The body’s stress response becomes heightened, leading to increased feelings of frustration and anger. Developing structured meal plans and incorporating balanced, nutrient-rich options help stabilize mood and reduce the intensity of withdrawal symptoms.
- Headaches: Headaches frequently occur during food withdrawal, especially when eliminating foods high in sugar or caffeine. Withdrawal symptoms, including headaches, emerge as the body adapts to changes in diet and reduced portions of addictive foods. Staying well-hydrated helps ease headache severity and support the body’s adjustment.
- Fatigue: Fatigue becomes overwhelming when adjusting to a new diet, making daily tasks and responsibilities harder to manage. Energy levels drop as the body adapts to the absence of quick sources like sugar, leading to persistent exhaustion. Sluggishness, diminished focus and decreased productivity are all consequences of withdrawals from addictive food items. The combination of physical tiredness and mental fog makes maintaining motivation especially challenging.
- Difficulty concentrating: Difficulty concentrating affects individuals struggling with FA as the brain adjusts to the absence of stimulant foods. Cognitive functions become impaired, creating challenges with focus, decision-making and memory recall. Changes in blood sugar levels and the brain’s longing for the dopamine surge once triggered by highly palatable meals contribute to such struggles.
- Depression: Depression intensifies during nutritional adjustment as the body and brain adapt to the absence of familiar sources of comfort and pleasure. The reduction in certain foods triggers a temporary drop in serotonin levels, impacting mood and emotional stability. Emotional responses during the withdrawal period reveal the strong psychological component of food addiction, highlighting how deeply eating habits intertwine with coping mechanisms and mental health.
What are the differences between food addiction and binge eating?
Differences between food addiction and binge eating refer to the unique traits and behaviors distinguishing each, despite shared characteristics. The differences between food addiction and binge eating are presented in the table below.
| Differences Between Food Addiction and Binge Eating | ||
| Aspect | Food Addiction | Binge Eating |
| Definition | Compulsive consumption of certain foods, often high in sugar, fat, and salt, despite negative consequences. | Recurrent episodes of eating large quantities of food quickly and to the point of discomfort. |
| Behavioral patterns* | Individuals with food addiction (FA) tend to display a consistent pattern of disrupted behavior. | People diagnosed with binge eating disorder (BED) commonly have episodes of disrupted behavior. |
| Motivation and purpose of eating* | Patients with FA overconsume specific foods to satisfy cravings and experience a sense of satisfaction. | Patients with BED tend to consume huge amounts of food to alleviate psychological distress, as succumbing to the desire provides a short-term sensation of pleasure and emotional relaxation. |
| Self-awareness* | Affected people lack self-awareness regarding eating patterns and use denial or projection as psychological defense mechanisms. | BED sufferers generally feel guilty about eating behaviors and are obsessed with body weight and shape, frequently demonstrating heightened awareness of body proportions and food portion sizes. |
| Behavioral response to eating restrictions* | The inability to get or eat the addictive foods causes patients with FA to act aggressively or anxiously. | BED patients typically prefer situations limiting the ability to binge. |
| Presence of classic addiction symptoms* | Common addiction signs like tolerance and withdrawal show up, along with behaviors like avoiding social interactions and giving up on other activities. | Typical signs of addiction do not appear. |
| Emotional response after eating* | After overindulging, no feelings of guilt or shame arise. | After binging, remorse or shame is felt. |
The major distinctions between food addiction and compulsive eating disorder are outlined in the table above. Successful treatment and support rely on understanding how the two conditions vary in symptoms and underlying mechanisms.