Benadryl addiction: definition, symptoms, effects, withdrawal, and treatment
Benadryl addiction involves the compulsive misuse of the antihistamine medication diphenhydramine, leading to increased tolerance, psychological dependence, and withdrawal symptoms upon attempting to reduce or cease use, driven by the drug’s psychoactive effects.
The symptoms and signs of Benadryl addiction are increased tolerance, cravings for the drug, repeated use despite consequences, memory problems or cognitive decline, mood swings, hallucinations, physical symptoms like dry mouth or dizziness, deceptive and secretive behavior, and withdrawal symptoms after stopping.
The effects of Benadryl addiction are categorized into short- and long-term effects. The short-term effects of Benadryl addiction include drowsiness, blurred vision, headache, loss of appetite, nausea and vomiting, and constipation. The long-term effects of Benadryl addiction are increased risk of dementia, poor coordination, liver or kidney strain, dependency and withdrawal, and psychosis.
The Benadryl withdrawal symptoms are insomnia, restlessness, irritability, confusion, tremors, tachycardia, sweating, and increased allergy symptoms.
The available treatments for Benadryl addiction are medical detox, cognitive behavioral therapy (CBT), counseling, support groups (e.g. 12-step programs), dual diagnosis treatment, lifestyle and sleep habit changes, and education and relapse prevention planning.
What is Benadryl addiction?
Benadryl addiction refers to the repeated and compulsive misuse of diphenhydramine (DPH), the active ingredient in Benadryl, often beyond recommended doses to achieve sedative, euphoric, or hallucinogenic effects.
While originally intended as an antihistamine for allergies, DPH is sometimes taken recreationally due to the drug’s psychoactive properties, leading to tolerance, dependence, and harmful side effects.
Individuals addicted to Benadryl experience cravings, withdrawal symptoms, and an inability to stop using despite negative consequences. Over time, high-dose DPH use impairs memory, disrupts cognitive function, and increases the risk of serious health issues, including heart problems and psychosis.
Why is using Benadryl addictive?
Using Benadryl becomes addictive because diphenhydramine affects the brain’s neurotransmitters, particularly by blocking histamine and acetylcholine. In high doses, the antihistamine produces feelings of relaxation, mild euphoria, or even hallucinations—something individuals begin to seek repeatedly.
Eventually, the body develops a tolerance, requiring larger amounts to achieve the same effects. Such a pattern of behavior leads to antihistamine abuse, where Benadryl is taken not for medical reasons but for the medication’s mind-altering properties.
What is the other name for Benadryl addiction?
The other name for Benadryl addiction is diphenhydramine abuse. The term describes the abuse of the medication diphenhydramine (DPH), frequently at dosages far greater than advised by doctors.
Often used over-the-counter for allergies, colds, and sleep problems, diphenhydramine is an antihistamine. However, when taken in excessive doses, DPH produces psychoactive effects certain people find desirable. DPH abuse, a type of substance misuse posing major health hazards, results from repeated usage for such effects.
Given the unrestricted availability of diphenhydramine, understanding the prevalence of Benadryl addiction helps grasp the scope of the issue and consider appropriate measures for addiction prevention.
How common is Benadryl addiction?
Benadryl addiction is relatively uncommon, but instances of misuse and dependence have been reported, with a 63% increase in intentional diphenhydramine exposures, including Benadryl, within 12 years, as reported in a 2021 study by Nemanich et al., titled “Increased rates of diphenhydramine overdose, abuse, and misuse in the United States, 2005-2016.”
According to the study’s analysis of data from the United States National Poison Data System, drug misuse among older persons aged 55–64 and ≥65 increased by roughly 126–143% and 230%, respectively.
Diphenhydramine (DPH)-related suicide cases rose, especially among children aged 10–14 (263%). The figures additionally revealed a 3.6% increase in reported deaths linked to diphenhydramine and a 91% increase in significant adverse clinical effects.
What are the symptoms and signs of Benadryl addiction?
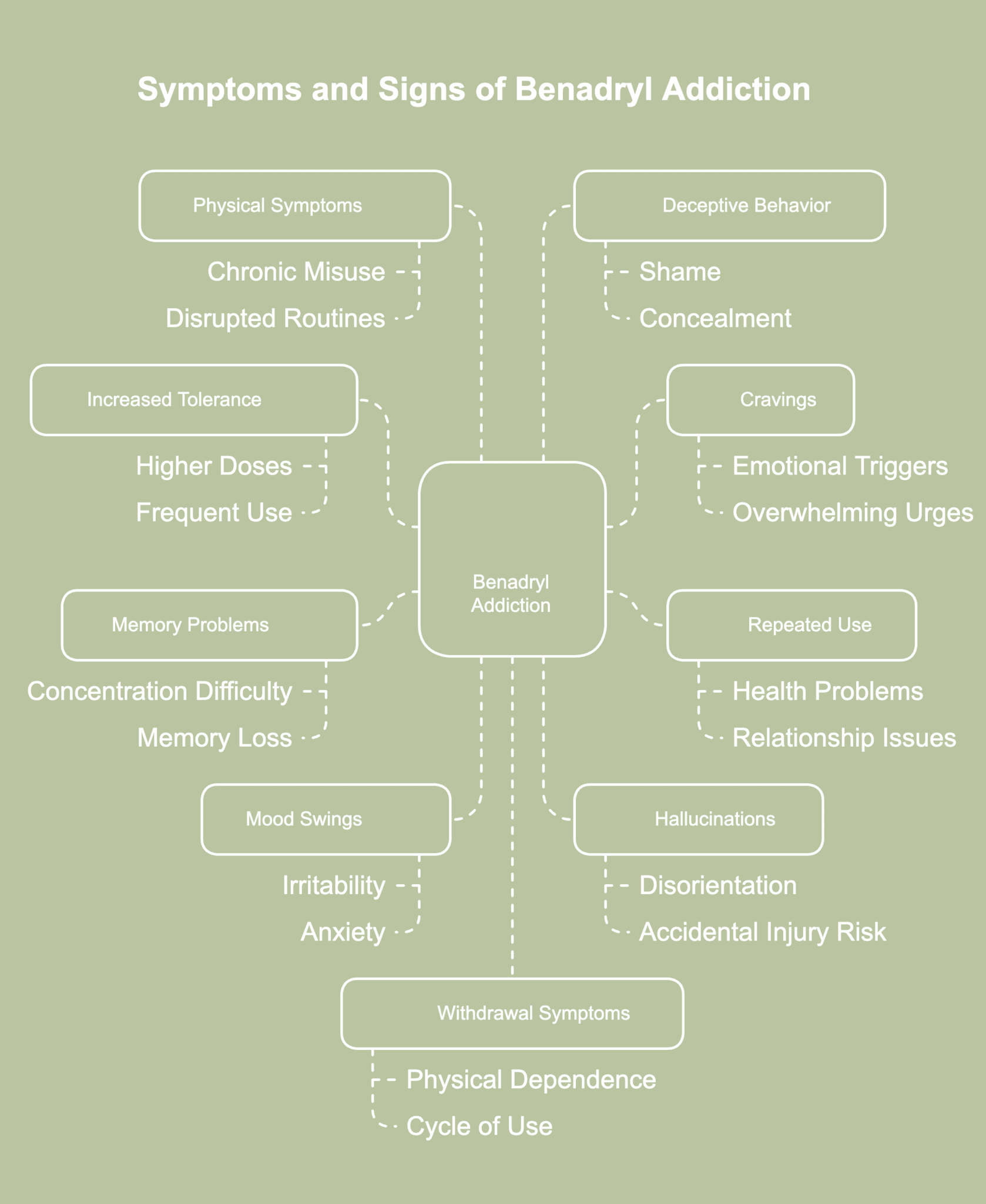
Symptoms and signs of Benadryl addiction refer to the physical, behavioral, and psychological indicators suggesting a person is misusing diphenhydramine. The symptoms and signs of Benadryl addiction are listed below.
- Increased tolerance: As the body adjusts to frequent use of diphenhydramine, a person begins needing higher doses to achieve the same sedative or euphoric effects. Tolerance develops quickly, especially when Benadryl is used recreationally rather than for allergies or sleep. Increased tolerance often marks the early stage of dependence, encouraging more frequent and risky usage. Without noticing, the person starts doubling or tripling doses just to feel something.
- Cravings for the drug: Cravings often manifest as an intense, persistent urge to take Benadryl, even when there’s no medical reason to do so. Such urges tend to take over thoughts, making focusing on daily tasks or responsibilities difficult. Emotional triggers such as stress or boredom heighten the desire to misuse the drug. The mental pull toward diphenhydramine often feels overwhelming, driving repeated use despite known risks.
- Repeated use despite consequences: Even when faced with health problems, strained relationships, or reduced performance at work or school, the person continues taking the drug. The behavior reflects a loss of control, where the need to consume Benadryl outweighs rational decision-making. Aware of the damage being caused, the individual still feels unable to stop.
- Memory problems or cognitive decline: Benadryl abuse interferes with the brain’s ability to store and process information, resulting in difficulty concentrating or recalling recent events. According to a 2021 study by Robbins et al., titled “Sleep medication use and incident dementia in a nationally representative sample of older adults in the US,” the use of sleep medication, such as diphenhydramine, is prevalent among older adults in the United States (15%, or 4.6 million individuals), and is linked to a 30% increased risk of incident dementia over the course of eight years.
- Mood swings: Sudden shifts in mood, such as irritability, anxiety, or unexplained sadness, become noticeable as the body and brain respond to diphenhydramine misuse. Emotional changes often occur without connection to external events, resulting in reactions seeming to be unpredictable or extreme. Friends and family are likely to notice a change in behavior long before the individual recognizes a problem.
- Hallucinations: At high doses, DPH produces vivid hallucinations, leading the person to see or hear things that are not real. Episodes often feel real and disorienting, blurring the line between imagination and perception. The symptom not just signals dangerous levels of misuse but increases the risk of accidental injury as well.
- Physical symptoms like dry mouth or dizziness: Although often overlooked, physical side effects such as dry mouth or dizziness point to chronic misuse. Such symptoms often appear even without recent use, suggesting a more serious issue. People sometimes dismiss the discomfort or assume another cause, yet persistent issues often disrupt normal routines.
- Deceptive and secretive behavior: Engaging in deceptive and secretive behavior, such as hiding or downplaying Benadryl use, is a common response among individuals struggling with addiction. Such behavior reflects a sense of shame or an attempt to conceal the extent of the problem.
- Withdrawal symptoms after stopping: When Benadryl use is suddenly reduced or stopped, the body reacts with symptoms such as anxiety, restlessness, nausea, or trouble sleeping. Withdrawal symptoms often indicate a physical dependence has developed. Rather than feeling better without the drug, the person experiences a temporary decline in mental or physical well-being. The distress caused by withdrawal frequently pushes the individual to return to using, creating a cycle nearly impossible to break.
What are the causes of Benadryl addiction?
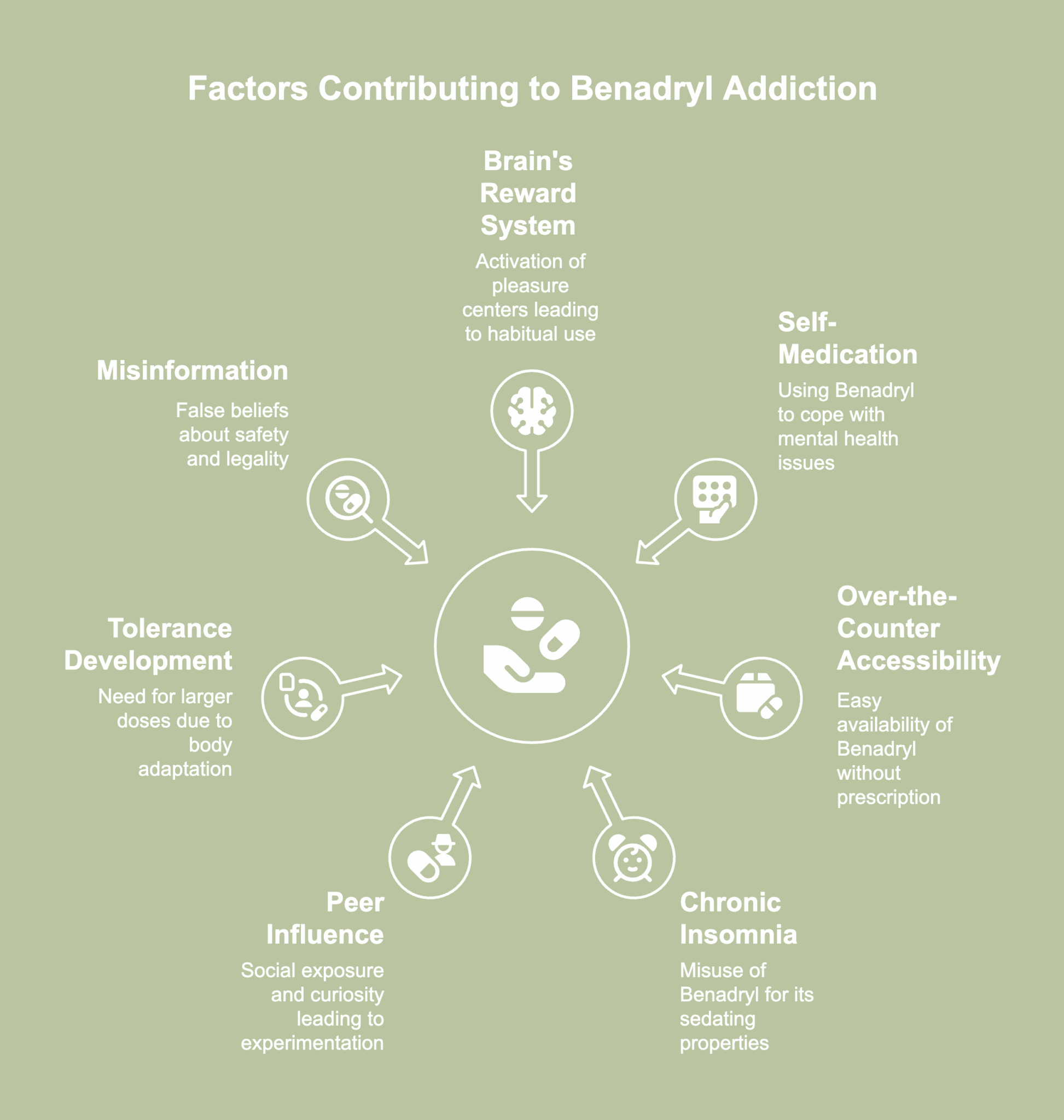
Causes of Benadryl addiction refer to the various factors leading individuals to misuse diphenhydramine repeatedly and compulsively. The causes of Benadryl addiction are listed below.
- Stimulation of the brain’s reward system: Substances like diphenhydramine trigger chemical changes in the brain, activating areas linked to pleasure and reinforcement. According to a 2017 report by Saran et al., titled “Chronic diphenhydramine abuse and withdrawal,” the euphoric sensations and drug-seeking behavior connected with antihistamine addiction are thought to be caused by elevated dopamine activity in a section of the brain known as the mesolimbic pathway. It promotes habitual engagement by fostering a sense of gratification. However, the precise mechanism underlying addiction is still unclear.
- Attempt to self-medicate mental health issues: People struggling with anxiety, depression, or chronic stress sometimes turn to Benadryl as a quick way to numb emotional discomfort. Without professional guidance or access to proper treatment, diphenhydramine becomes a substitute coping mechanism. Using the drug to quiet the mind or escape from negative feelings gradually turns into a habit. Dependence grows as the brain begins to rely on the addictive substance for emotional relief.
- Over-the-counter accessibility: Benadryl is easy to buy at pharmacies, supermarkets, and convenience stores without needing a prescription, lowering the barrier to misuse. Sold next to common household remedies, numerous people assume large doses are harmless. Discreet and repeated purchases often go unnoticed, allowing misuse to grow gradually. Easy access increases the temptation for individuals seeking quick relief or a legal high.
- Chronic insomnia: Certain individuals misuse Benadryl for its sedating properties when experiencing frequent sleeplessness or poor-quality rest. Findings of a 2024 study titled “Factors Associated With the Use of Over-theCounter Sleep Aids Among Jazan University Students” by Alfarhan et al., revealed a significant percentage of university students—56.3%—had used over-the-counter sleep aids, especially diphenhydramine hydrochloride, and 9.4% had used the drug for an extended period of time. Significant drivers of this use include sleep difficulties, such as a 13.7% insomnia diagnosis rate and a 78.7% prevalence of pain-related sleep disturbances, as well as other indications like colds and headaches.
- Peer influence and social exposure: Hearing friends talk about using high doses of Benadryl recreationally or watching videos promoting its effects often sparks curiosity to try the drug. Social media platforms, online forums, or peer circles sometimes downplay the risks, creating a false sense of safety. In an attempt to fit in or satisfy curiosity, individuals mimic the behavior.
- Tolerance development after prolonged use: Frequent use of Benadryl causes the body to adapt, leading to a need for larger doses to achieve the same calming or drowsy results. Such a change marks the start of physical dependence, though many fail to notice the pattern early on. Gradually, what used to work no longer feels effective, encouraging increased intake. With time, chasing the original effect leads to habitual use and eventual addiction.
- Misinformation about safety and legality: Since Benadryl is sold over the counter and widely used for allergies or colds, certain people assume high doses carry no real danger. False beliefs often lead to casual misuse, with no awareness of the potential consequences. The legal status of diphenhydramine creates a misleading sense of security, masking the risk of addiction. Without proper education, users underestimate both short- and long-term effects.
What are the effects of Benadryl addiction?
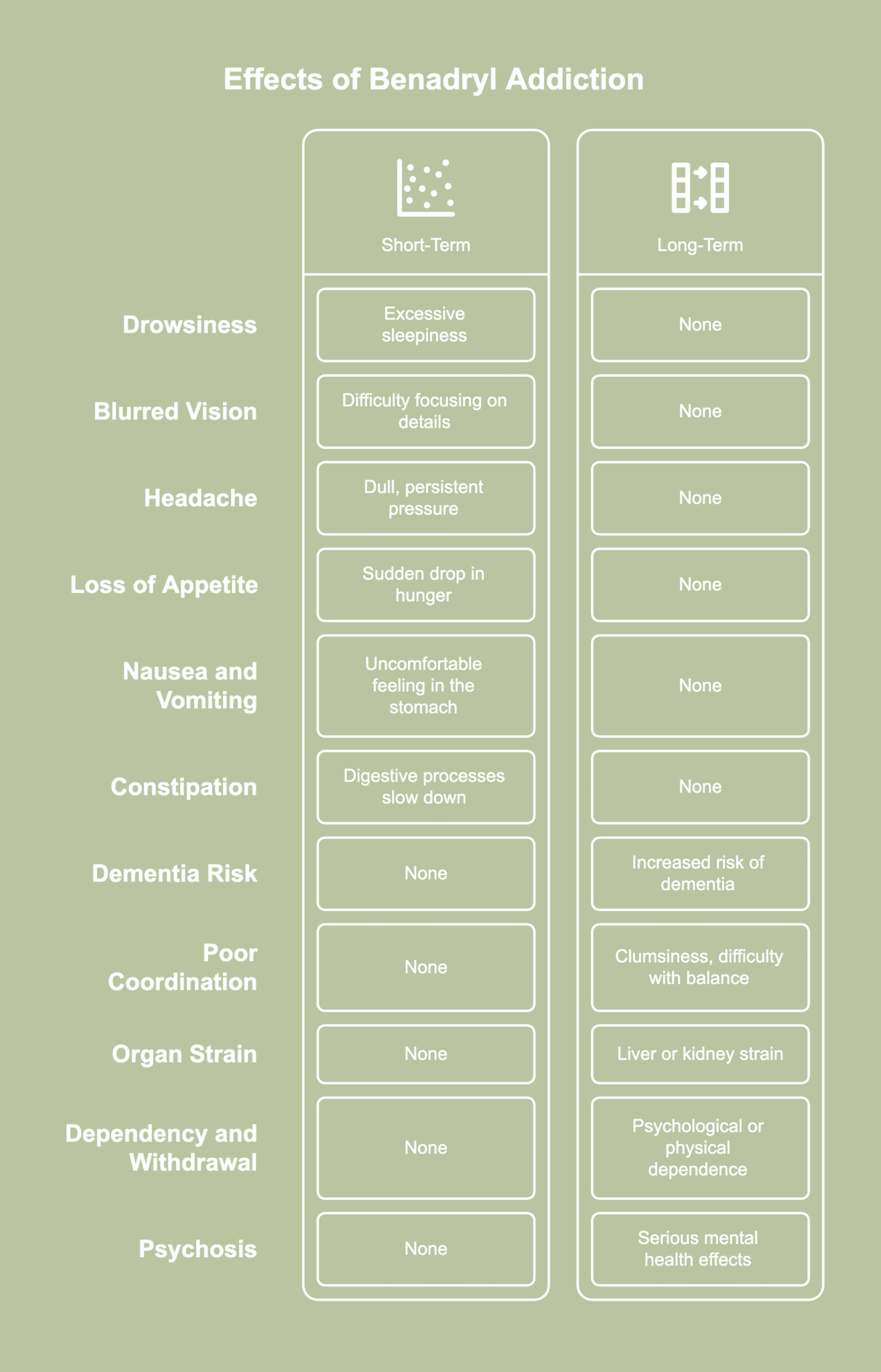
Effects of Benadryl addiction describe the short-term and long-term repercussions of chronic diphenhydramine abuse. The effects of Benadryl addiction are listed below.
Short-term effects
- Drowsiness: Excessive drowsiness often occurs as diphenhydramine slows down the central nervous system, leaving the user feeling unusually sluggish or sleepy. Staying alert becomes challenging, even during activities normally requiring full attention. Napping throughout the day or struggling to stay awake in quiet environments become a regular occurrence.
- Blurred vision: Blurred vision creates difficulty when focusing on details or reading text, often leading to discomfort or eye strain. Objects appear out of focus or doubled, even in well-lit environments. The experience remains disorienting throughout the period of impaired sight.
- Headache: Headaches frequently develop shortly after taking large doses of Benadryl, often described as a dull, persistent pressure around the forehead or temples. The discomfort sometimes builds gradually, interfering with concentration and increasing irritability. Bright lights or loud noises make the pain feel more intense. Even after the sedative effects fade, the lingering headache continues to affect mood and focus.
- Loss of appetite: A sudden drop in hunger often follows Benadryl misuse, making meals feel less appealing or even unappetizing. Disinterest in food leads to skipped meals or smaller portions, reducing nutritional intake. Over time, noticeable weight loss or weakness develops from consistently eating less. Many users fail to notice the pattern until physical health begins to suffer.
- Nausea and vomiting: Nausea starts with an uncomfortable feeling in the stomach, gradually growing stronger and occasionally resulting in vomiting. The unpleasant taste, stomach cramps, and physical strain make daily routines difficult to manage. The reaction is especially common when the drug is taken on an empty stomach or in higher-than-recommended amounts. Repeated episodes lead to dehydration or reluctance to take in food or fluids.
- Constipation: Constipation tends to develop when diphenhydramine slows down the body’s digestive processes, making bowel movements less frequent. The buildup often causes bloating, discomfort, or a heavy sensation in the abdomen. Affected individuals feel frustrated or sluggish due to the ongoing difficulty in passing stool.
Long-term effects
- Increased risk of dementia: Repeated exposure to anticholinergic drugs like Benadryl interferes with brain chemicals important for memory and awareness. According to a 2023 study by Poonawalla et al., titled “Anticholinergic exposure and its association with dementia/Alzheimer’s disease and mortality in older adults,” taking more anticholinergic drugs like diphenhydramine and using such drugs for a longer time markedly increased mortality and dementia/Alzheimer’s disease risks in older persons.
- Poor coordination: Poor coordination becomes evident through clumsiness, difficulty with balance, or trouble performing fine motor tasks. Actions like walking in a straight line, holding utensils, or typing on a keyboard start to feel awkward or imprecise. The symptom increases the risk of accidents, especially when combined with dizziness or blurred vision. Over time, repeated coordination issues signal deeper impairment of the nervous system.
- Liver or kidney strain: Processing high doses of Benadryl repeatedly over time places added stress on the liver and kidneys. The organs work hard to filter the drug, increasing the chance of long-term damage. Warning signs like fatigue, swelling, or changes in urination sometimes appear too late. Without medical support, organ function continues to decline gradually.
- Dependency and withdrawal: Long-term use often leads to psychological or physical dependence, where stopping the drug becomes difficult. Skipping doses trigger uncomfortable symptoms, pulling the person back into a cycle of use. Withdrawal symptoms vary, but the discomfort usually makes quitting feel overwhelming. Recovery becomes harder the longer the pattern continues.
- Psychosis: Serious mental health effects sometimes develop after long-term Benadryl misuse, with psychosis being one of the most extreme outcomes. Key findings of a February 2025 study by Mosca et al., titled “Over-the-counter Psychosis: A Systematic Review of the Misuse of Antihistamines, Cough Medicines, and Decongestants and the Risk of Developing Psychosis” revealed the abuse of antihistamines, such as DPH, results in psychotic symptoms, including hallucinations, paranoia, and thought disorders.
What happens if you take a lot of Benadryl?
If you take a lot of Benadryl, the risk of a serious medical emergency becomes dangerously high, often resulting in what is known as a Benadryl overdose. The body begins to react in unpredictable and harmful ways, disrupting normal brain function and overwhelming internal systems.
In certain cases, individuals lose touch with reality or lose consciousness altogether, prompting the need for urgent care. A risky social media trend known as the “Benadryl challenge” has pushed users—particularly teenagers—to take large amounts of the drug in the hopes of having hallucinations, which has resulted in hospitalizations and even death.
Such a form of drug abuse is potentially fatal since it puts a great deal of strain on the heart, brain, and other organs. Recovery is not always quick or guaranteed, and the long-term consequences are serious. Misusing Benadryl in large amounts is never safe, regardless of intent.
Can you overdose on Benadryl?
Yes, you can overdose on Benadryl. Diphenhydramine overdose or intoxication occurs either accidentally or deliberately, according to a publication by Huynh et al., titled “Diphenhydramine Toxicity,” last updated in April 2023.
Although purposeful diphenhydramine overdose or intoxication occurs in individuals seeking self-harm or suicide, there is documentation of individuals utilizing diphenhydramine to attain euphoric and pleasurable effects.
The article added that a study conducted in 2016 revealed diphenhydramine overdoses accounted for 3.2% of drug overdose fatalities in the United States. Diphenhydramine was included as one of the top 15 substances that caused drug overdose deaths in the United States in the same survey. Children six years of age or under account for the majority of diphenhydramine overdose and intoxication incidents.
A drug overdose involving Benadryl affects the body in complex ways often requiring emergency medical intervention. The severity of the outcome depends on how much was taken, how quickly treatment is received, and the person’s overall health.
What is considered long-term use of Benadryl?
Taking the drug for more than two weeks—especially without medical supervision—is generally considered as long-term use of Benadryl. Though intended for short-term relief, many people begin using the medication regularly to manage sleep problems, anxiety, or chronic allergy symptoms.
Constant use over such a period lowers the efficacy of the medicine and raises the possibility of physical dependency. As tolerance builds, individuals often start taking higher doses to achieve the same sedating effects.
Particularly in elderly persons, long usage of diphenhydramine has been related to an increased incidence of dementia. The medicine gradually reduces cognitive ability by interfering with acetylcholine, a brain neurotransmitter vital for memory.
Even when used for common issues like sleeplessness, taking Benadryl for more than 14 days without guidance poses health concerns. What initially seems like a harmless over-the-counter solution eventually leads to long-lasting side effects if not addressed properly.
What are Benadryl withdrawal symptoms?
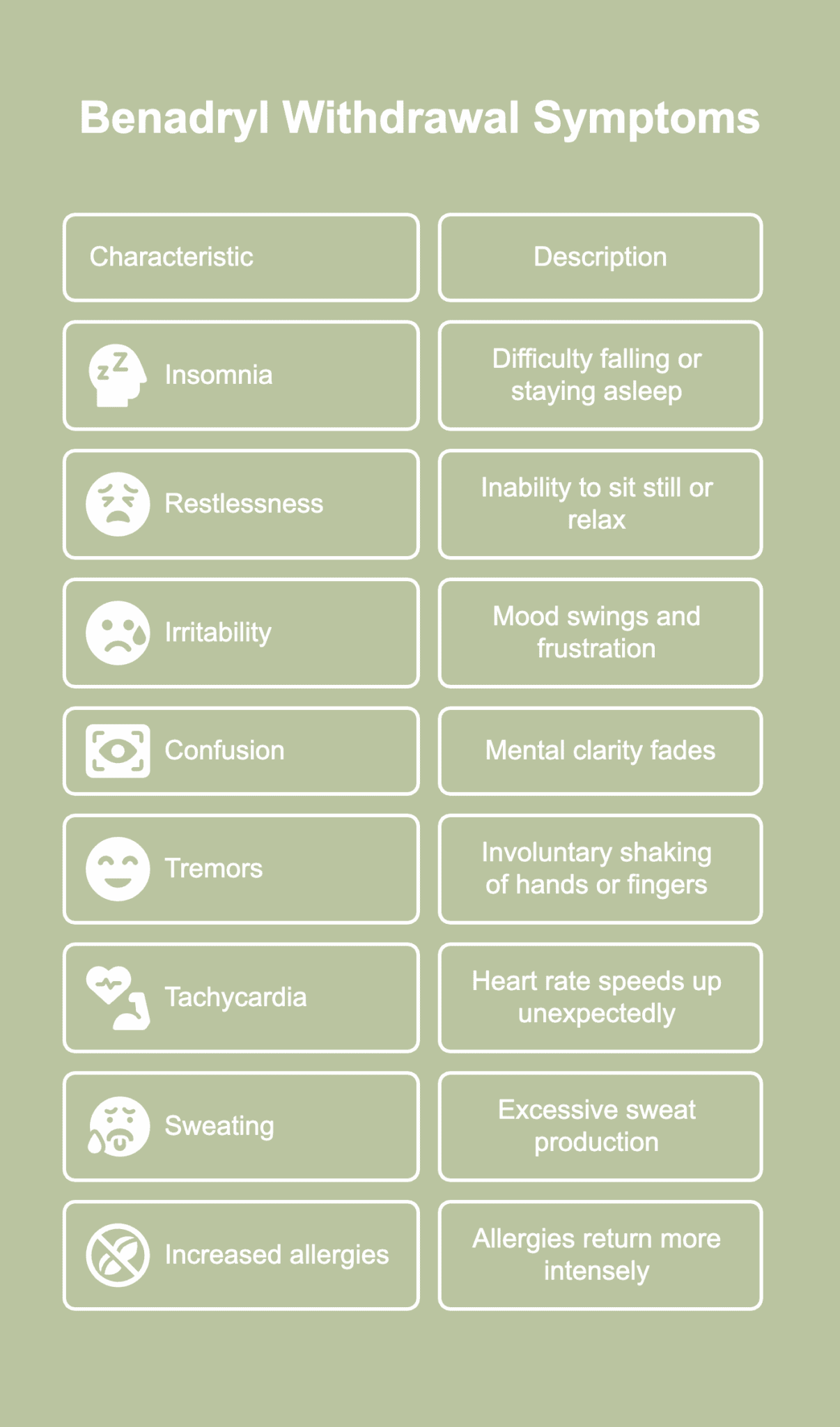
Benadryl withdrawal symptoms refer to the reactions occurring when a person who has been using diphenhydramine regularly or in large amounts suddenly reduces or stops taking the drug. The Benadryl withdrawal symptoms are listed below.
- Insomnia: Sleep becomes elusive after stopping DPH, especially for people who used the medication regularly as a sleep aid. Nights feel longer as the body struggles to fall or stay asleep without chemical support. Sleep disruption often leads to fatigue and mood changes during the day.
- Restlessness: A person experiences restlessness as an inability to sit still, relax, or focus, often paired with nervous energy or discomfort. Instead of feeling calm, the body remains tense, and the mind races with unease. The symptom grows worse at night, disrupting sleep and heightening frustration. Even in quiet settings, the need to pace, fidget, or move constantly becomes difficult to ignore.
- Irritability: Mood swings often surface, with minor inconveniences triggering disproportionate reactions. Emotional regulation weakens, leaving individuals more prone to frustration or anger. The sudden lack of sedation from the drug tends to make everyday stressors feel more overwhelming. Patience becomes harder to maintain during withdrawal.
- Confusion: Mental clarity sometimes fades, making routine decisions harder to navigate. Simple tasks require more effort, leading to frequent pauses or second-guessing. Foggy thinking reflects the brain’s attempt to recalibrate without the drug’s influence. The disorientation is usually temporary but noticeably disruptive.
- Tremors: Hands or fingers start shaking involuntarily, especially during moments of stress or restlessness. The physical reaction often feels alarming to individuals unfamiliar with withdrawal effects. Although not dangerous, tremors create discomfort and interfere with tasks like writing or holding objects.
- Tachycardia: Heart rate speeds up unexpectedly, even during rest, creating a sense of unease or panic. A 2017 report by Saran et al., titled “Chronic diphenhydramine abuse and withdrawal: A diagnostic challenge” presented a complex case of DPH withdrawal in a 21-year-old male who had been chronically abusing DPH. The individual presented with tremors, psychosis, and autonomic dysfunction. The withdrawal syndrome was characterized by tachycardia, determined to be the result of sympathetic hyperactivity or rebound cholinergic activity after the abrupt cessation of DPH activity.
- Sweating: Even in cool environments, the body produces excessive sweat during withdrawal. The response comes from an overstimulated nervous system adjusting to the absence of diphenhydramine. Damp clothes and skin contribute to physical discomfort and self-consciousness. The sweating often lessens after the initial withdrawal period ends.
- Increased allergy symptoms: Without Benadryl’s antihistamine effects, allergies once suppressed return more intensely. Sneezing, itchy eyes, or nasal congestion suddenly flare up. The body must now manage allergic reactions without artificial support. For chronic allergy sufferers, rebound feels especially frustrating.
What are the available treatments for Benadryl addiction?
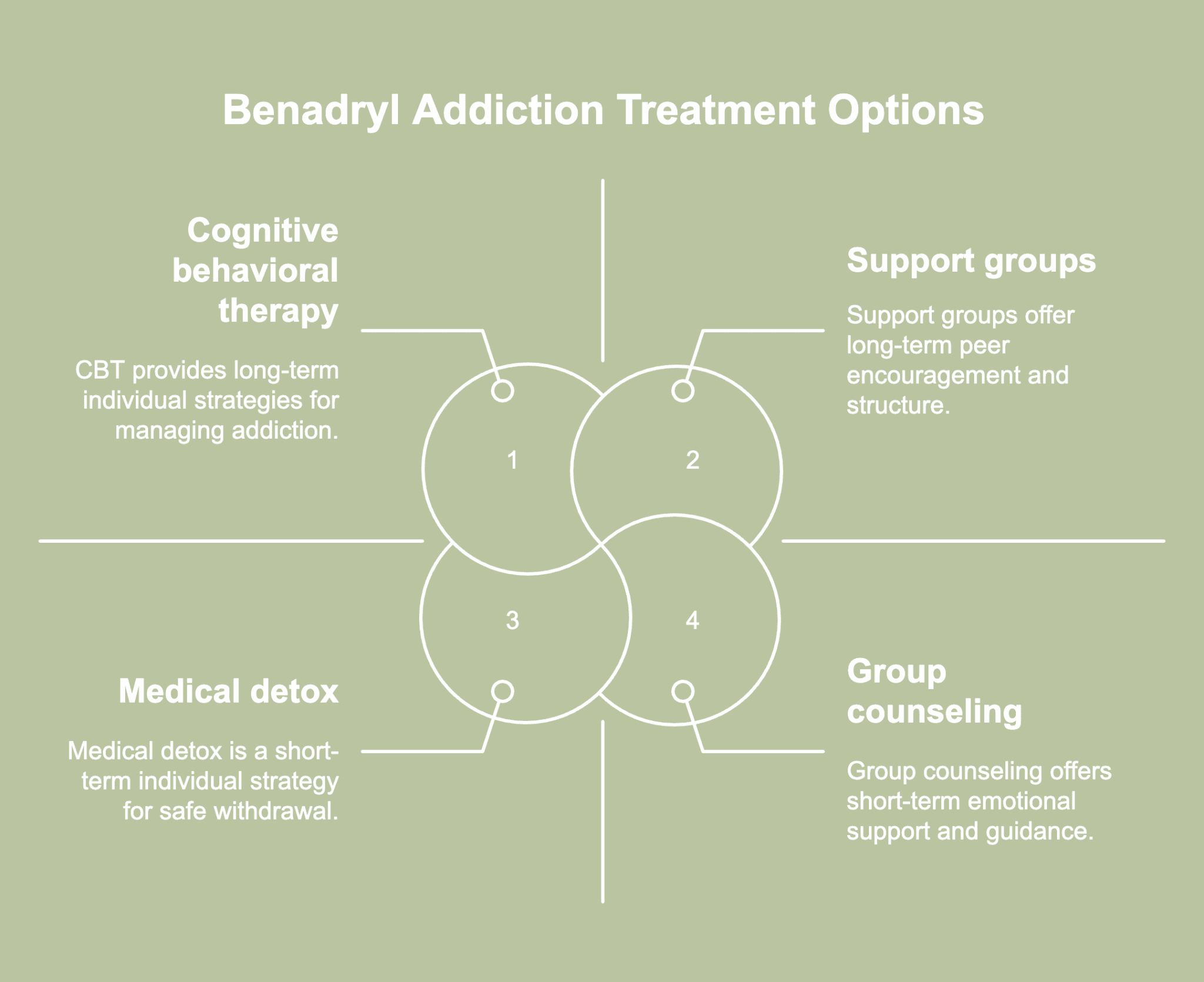
Available treatments for Benadryl addiction refer to the methods used to keep individuals from misusing the antihistamine medication. The available treatments for Benadryl addiction are listed below.
- Medical detox: Supervised detox provides a safe environment for gradually tapering off Benadryl under professional care. Health experts monitor withdrawal symptoms and step in when complications arise, reducing risks associated with stopping suddenly. Instead of quitting cold turkey, the body gets time to adjust with fewer setbacks.
- Cognitive behavioral therapy (CBT): CBT helps individuals identify the thoughts and behaviors contributing to DPH misuse. The sessions concentrate on the substitution of unhealthy patterns with practical strategies for the management of tension, anxiety, or insomnia. The therapy delves into the underlying causes of addiction, rather than concentrating solely on surface-level symptoms. Through CBT, a variety of people acquire long-lasting abilities frequently helpful in contexts other than substance abuse recovery.
- Counseling: Individual and group counseling offers a platform for individuals to share experiences and receive guidance. Sessions foster emotional support, coping strategies, and community throughout the recovery journey.
- Support groups (e.g. 12-step programs): Programs modeled after the 12-step approach provide structure, peer encouragement, and a clear path toward recovery. Regular meetings create routines, helping participants stay focused and avoid relapse. Recovering individuals find value in having a sponsor or mentor with firsthand experience overcoming similar challenges. Support groups often continue to benefit individuals long after formal treatment ends.
- Dual diagnosis treatment: When Benadryl addiction exists alongside conditions like anxiety or depression, dual diagnosis treatment addresses both issues simultaneously. The approach prevents one problem from undermining the progress made with the other. Integrated care often involves a team of mental health and addiction specialists working together. Long-term recovery becomes more sustainable when all underlying conditions receive attention.
- Lifestyle and sleep habit changes: Improving daily routines—such as limiting caffeine, sticking to a regular sleep schedule, and creating a calming bedtime environment—helps reduce the urge to rely on antihistamines. Especially since tolerance to diphenhydramine’s sedative effects develops quickly, changing one’s lifestyle is typically the best course of action for chronic insomnia, according to a January 2025 study by Clark et al., titled “Diphenhydramine: It is time to say a final goodbye.”
- Education and relapse prevention planning: Learning about the risks of long-term antihistamine use empowers individuals to make informed choices moving forward. Recognizing triggers and avoiding high-risk situations require awareness. Relapse prevention techniques including coping mechanisms and emergency contacts are part of multiple treatment programs. Continuous learning reinforces long-term commitment and keeps rehabilitation efforts on course.


