Substance abuse assessment tools: definition, importance, and types
Substance abuse assessment tools refer to questionnaires, forms, and clinical interviews used to determine the nature and extent of an individual’s substance use problem; their risk factors and chances of developing an addiction; and how likely they are to develop complications from substance use.
Substance abuse assessment tools are important because they facilitate the timely and targeted delivery of therapeutic interventions to individuals who are addicted to substances or are at risk of developing drug and/or alcohol addiction. These tools are thus able to prevent problematic substance use habits from progressing to full-blown addiction. They allow healthcare practitioners to formulate customized and patient-centric treatment plans.
The different types of substance abuse assessment tools are the Alcohol Use Disorders Identification Test (AUDIT), Paddington Alcohol Test (PAT), CAGE Assessment, CRAFFT Screening Test, TAPS screening (TAPS-1), and Drug Abuse Screening Test (DAST-10).
What are substance abuse assessment tools?
Substance abuse assessment tools are standardized questionnaires, screening forms, and diagnostic interviews designed to determine an individual’s drug and alcohol use or misuse patterns, risk factors, and their chances of developing an addiction. These tools typically conform to specified guidelines for administration, scoring, and interpretation.
Specific tools reveal whether an individual is at low, moderate, or high risk of developing complications from substance use. The insights and findings obtained from these assessment tools help determine the need, if any, for intervention and the most effective treatment strategy for an individual.
Why are substance abuse assessment tools important?
Substance abuse assessment tools are important because they help identify individuals with an addiction problem or those who are at risk for developing a substance use disorder, thereby facilitating the timely and targeted delivery of treatment. These tools help evaluate the nature and extent of a substance use problem; the presence, if any, of a comorbid physical and/or psychiatric condition in the patient that will influence disease trajectory and medical care; and the need for intervention and/or further assessment.
The wealth of information that these tools unearth allows healthcare practitioners to formulate a customized treatment plan. These tools are designed to gather information in a structured and comprehensive way and cut through the stigma and misinformation around substance use. They thus open up a channel of communication with the patient, enhance the clinical relationship, and encourage positive change.
Substance abuse assessment tools facilitate addiction treatment by identifying individuals who require harm reduction interventions or intensive treatment for a full-blown addiction. This ensures that individuals receive and benefit from interventions that prevent problematic substance use habits from progressing to full-blown drug addiction.
These tools promote holistic and long-term addiction recovery by allowing physicians to assess the risk or confirm the presence of other or comorbid physical and/or psychiatric diseases that are likely affecting the addiction process and will influence the treatment plan, according to a May 2024 publication by the Johns Hopkins University, titled “Substance Use Screening, Risk Assessment, and Use Disorder Diagnosis in Adults.”
For instance, the presence of a comorbid condition like depression necessitates the delivery of an integrated treatment program that addresses both psychiatric conditions concurrently. Additionally, these tools allow healthcare practitioners to learn about a patient’s medical history, family history, and the socio-cultural influences on their health and substance-use habits. This knowledge helps physicians create patient-centered treatment plans that are effective and convenient for an individual to adhere to.
What is the process of substance abuse assessment?
The process of substance abuse assessment involves a preliminary screening followed by thorough evaluation, formal diagnosis, treatment planning and/or referral to treatment services, and ongoing monitoring. Screening is conducted to determine the likelihood of an individual having a substance use disorder or evaluate their risk factors for developing substance addiction.
Screening is done using instruments like questionnaires and interviews administered by a healthcare practitioner or self-reports completed by the individual being screened. The outcome of a screen is a “yes” or a “no.” A positive screen is followed by a risk assessment process that uses instruments like clinical interviews, self-reports, personal history-taking, collateral report gathering, and laboratory tests to obtain information.
During risk assessment, individuals are asked questions about the frequency and intensity of substance use to evaluate the clinical significance and severity of their drug-use behaviors. Additionally, the individuals are assessed for biomedical, emotional, and behavioral conditions and complications, treatment readiness, relapse and/or persistent use potential, recovery history, and living environment. Their responses help healthcare practitioners determine how risky their substance use problem is, how likely they are to experience the adverse consequences of their drug-use habits, and to what extent. Knowing about the individual’s familial, social, and vocational supports and deficits helps healthcare professionals specify the appropriate level of care and plan viable treatment plans.
Depending on their risk scores (low, moderate, or high), individuals are referred to treatment directly without providing feedback or advice, or offered brief intervention to motivate them to consider entering into brief or intensive treatment. It is also possible that individuals are only educated on the potential adverse consequences of their substance use habits.
Screening and assessments are carried out periodically based on clinical evidence. These follow-up assessments are a part of an ongoing monitoring process to evaluate treatment response and modify treatment strategies, if needed.
Who conducts substance abuse assessments?
Substance abuse assessments are typically conducted by licensed mental healthcare practitioners with specialized training to carry out intensive and accurate examinations. A team comprising multiple professionals, such as a psychiatrist, a psychologist, a substance abuse counselor, and/or a social worker, will likely conduct this examination at a specialized addiction treatment facility.
Substance abuse assessments are conducted by professionals who are specialists in substance abuse issues. In instances where specialists are not available, assessments are carried out by physicians, physician assistants, clinical nurse specialists, and nurse practitioners, as noted in the chapter “Assessment” from the 1997 publication by the Substance Abuse and Mental Health Services Administration, titled “A Guide to Substance Abuse Services for Primary Care Clinicians.”
These professionals have experience in empathic motivational interviewing. They are knowledgeable about the signs and symptoms of substance abuse, the biopsychosocial effects of substances of abuse, and the possible disease trajectory. They are aware of the common comorbid conditions associated with drug abuse and the classification system of the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), and are able to interpret disease findings in the context of the DSM system. Their holistic body of knowledge also includes a keen and insightful understanding of how to apply and interpret standardized assessments.
Where are substance abuse assessments taken?
Substance abuse assessments are taken in primary care settings, emergency departments of healthcare establishments, and trauma units. These assessments are carried out in school settings, youth social service agencies, mental healthcare facilities, and facilities under the criminal justice system.
Why does one need substance abuse assessment?
One needs a substance abuse assessment to identify the presence and determine the severity of a substance use disorder. This knowledge helps inform and guide treatment planning by healthcare professionals. The percentage of individuals with risk factors for developing a substance use disorder is considerably higher than that of individuals with an active addiction. Individuals need an assessment if they are concerned that their symptoms and/or alcohol- or drug-use behaviors place them at an increased risk of developing a substance use disorder.
The findings from a substance use assessment help explore the medical, behavioral, social, financial, occupational, and academic problems that are likely caused and/or aggravated by their use of a substance.
Assessments determine the severity (mild, intermediate, moderate, or severe) of an established addiction issue, thereby compelling individuals to move past denial and accept that they have a problem that needs to be remedied. This realization encourages them to contemplate making positive change and/or re-examine their degree of readiness for treatment. Eventually, substance abuse assessments help individuals halt the progression of a substance use disorder and/or reduce the negative health and psychosocial consequences of a full-blown addiction problem.
What are the different types of substance abuse assessment tools?
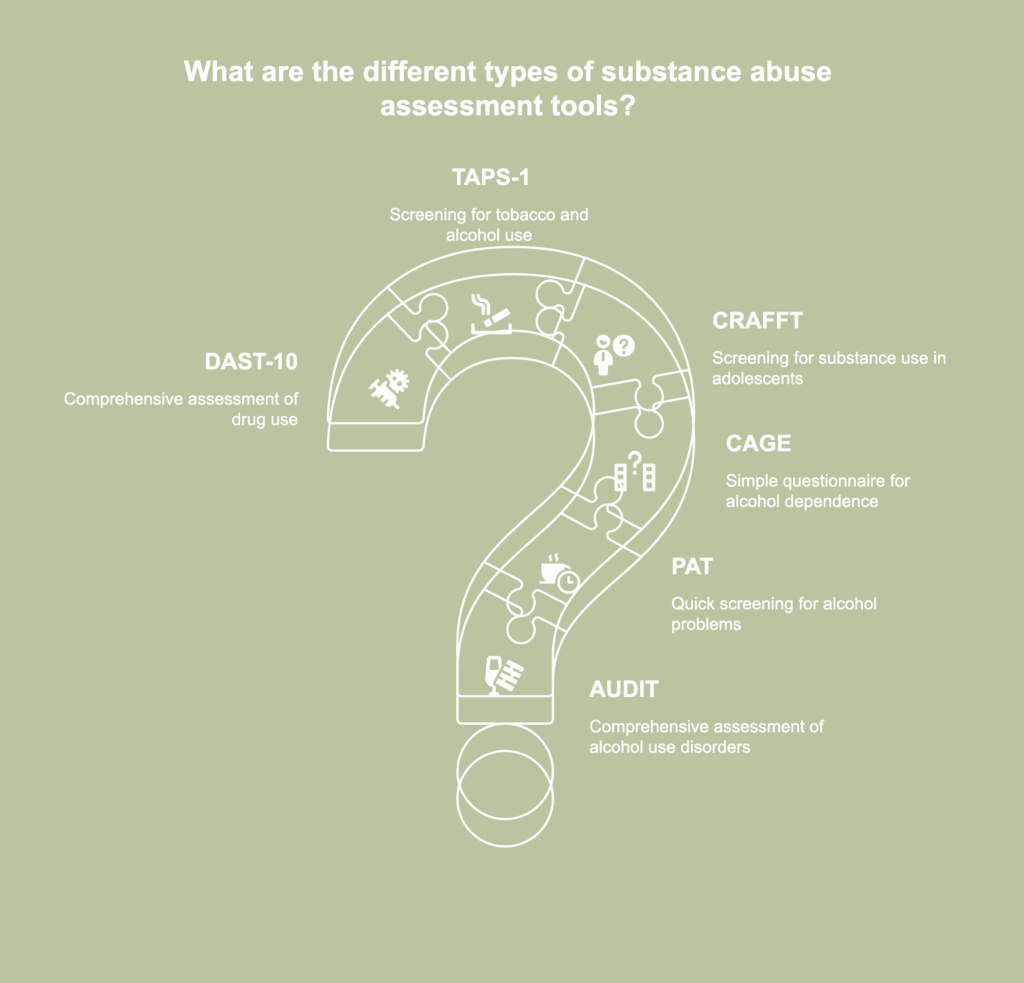
The different types of substance abuse assessment tools are listed below.
- Alcohol Use Disorders Identification Test (AUDIT)
- Paddington Alcohol Test (PAT)
- CAGE Assessment
- CRAFFT Screening Test
- TAPS screening (TAPS-1)
- Drug Abuse Screening Test (DAST-10)
1. Alcohol Use Disorders Identification Test (AUDIT)
The Alcohol Use Disorders Identification Test (AUDIT) was developed by the World Health Organization (WHO) to evaluate the nature and extent of alcohol use and drinking behaviors and alcohol-related problems. It comprises 10 questions and is available in two versions: one that is administered by a clinician and the other, a self-report. Since its publication in 1989, AUDIT has become the most widely used alcohol use screening tool. It is currently available in 40 languages.
The WHO, in its November 2001 publication titled “AUDIT: the Alcohol Use Disorders Identification Test: guidelines for use in primary health care,” notes that the tool has been designed to screen for risky or hazardous alcohol consumption patterns, such as excessive drinking, and to facilitate brief assessments. It has the ability to confirm excessive drinking as the cause of a presenting disease. Additionally, the information gathered through AUDIT helps healthcare practitioners formulate an intervention plan to help risky drinkers reduce or stop alcohol consumption, thereby preventing the onset or exacerbation of alcohol-related physical, emotional, and psychosocial problems. AUDIT helps identify alcohol addiction and multiple consequences of problematic drinking. It is a simple tool, well-suited for use in primary healthcare settings. Although it was developed for use by healthcare practitioners, with appropriate instructions, even non-health professionals are able to use AUDIT.
AUDIT was initially employed for rapidly detecting hazardous or harmful alcohol use patterns. However, it is now increasingly finding usage in epidemiological or cross-cultural studies involving populations with varied demographic characteristics, such as individuals with mental health disorders. The tool also facilitates relevant comparisons among genders and individuals with different sexual orientation, according to a 2023 article by Horváth et al., published in the journal Comprehensive Psychiatry, titled “Psychometric properties of the Alcohol Use Disorders Identification Test (AUDIT) across cross-cultural subgroups, genders, and sexual orientations: Findings from the International Sex Survey (ISS).”
The original version of AUDIT focuses on three primary domains of alcohol consumption. Items 1 to 3 are related to alcohol use; items 4 to 6 focus on alcohol dependence; and items 7 to 10 assess negative consequences. An individual’s score is plotted on the range 0-40 points. A score between 0-7 points indicates low-risk or abstinent drinking, and that between 8-15 points indicates a hazardous alcohol consumption pattern. A score between 16-19 points denotes harmful alcohol use, and alcohol dependence is indicated by a score between 20-40 points. However, authors Horváth et al., in their 2023 article, clarify that the cutoff scores vary based on the population being assessed.
2. Paddington Alcohol Test (PAT)
The Paddington Alcohol Test (PAT) is a brief questionnaire designed to be administered by emergency medical personnel to identify early onset hazardous drinkers among those patients whose presenting condition was likely caused by alcohol misuse. The test was developed by the Emergency Department of St. Mary’s Hospital, Paddington, and first published in 1996. The original version of the test was a 3-item questionnaire that explored the frequency of binge drinking, maximum alcohol consumption, and whether the individual believed alcohol misuse had contributed to their visit to the emergency department.
The PAT Test is used to identify patients who are most likely to benefit from brief advice (BA) about alcohol use. This brief advice comprises an offer of a consultation with an alcohol nurse specialist for a brief and personalized motivational enhancement intervention. It has been observed that for every two patients who choose to receive BA, there is one less emergency department re-admittance over the following year, according to a 2009 article by Robin Touquet and Adrian Brown published in the journal Alcohol and Alcoholism, titled “PAT (2009)—Revisions to the Paddington Alcohol Test for Early Identification of Alcohol Misuse and Brief Advice to Reduce Emergency Department Re-attendance.” This finding justifies the resources spent on BA. The revised PAT (2009) includes information about the clinical manifestations of alcohol misuse and guidelines on when to administer a blood alcohol concentration test.
3. CAGE Assessment
The CAGE Assessment is a preliminary screening test comprising a set of 4 questions designed to identify if an individual has a substance use disorder. The four letters of the acronym CAGE represent the keywords in the four questions. These keywords are Cut, Annoyed, Guilty, and Eye. The test was originally developed to screen for alcohol use disorder by Dr. John Ewing, the founding Director of the Bowles Center for Alcohol Studies of the University of North Carolina at Chapel Hill. Since then, multiple versions of the CAGE Assessment have been designed to screen for dependency on other addictive substances, such as drugs.
Although the CAGE Assessment was designed for self-assessment, it is extensively used in primary care settings. It is a valid tool for identifying problematic alcohol use and dependence in medical and surgical inpatients, psychiatric inpatients, and ambulatory medical patients, according to a 2007 article by Dhalla et al., published in the journal Clinical and Investigative Medicine, titled “The CAGE questionnaire for alcohol misuse: a review of reliability and validity studies.” However, the authors note that the test is less reliable for identifying less severe alcohol use patterns.
The questions in the CAGE Assessment tool have to be answered with a “yes” or a “no.” A response is scored 0 or 1. A higher score indicates problematic substance use. A score of 2 or more, or answering “yes” to two or more questions, is regarded as being clinically significant and indicates dependency on a substance of abuse. However, a CAGE Assessment score is not a formal diagnosis, which should be made by a licensed medical practitioner after conducting a thorough evaluation.
4. CRAFFT Screening Test
The 6-item CRAFFT is a standardized questionnaire designed to screen for substance use in adolescents (aged 12-21 years) in clinical settings. CRAFFT stands for Car; Relax; Alone; Forget; Friends; Trouble. It is a mnemonic of the key alphabets in the test questions. The tool is recommended by the Bright Futures Guidelines of the American Academy of Pediatrics as a screening tool to be administered for preventive care and during wellness visits, the National Institute of Alcohol Abuse and Alcoholism (NIAAA) Youth Screening Guide, and the Center for Medicaid and CHIP Services’ Early and Periodic Screening, Diagnostic and Treatment (EPSDT) program. The questionnaire is available in English and multiple other languages. It is available as an interview tool to be administered by a mental healthcare provider and a questionnaire to be completed by the patient.
Two updated versions of CRAFFT have been made available. Both retain the questions contained in the original version of the test. The CRAFFT 2.1 version includes extra assessments for vaping and the use of edibles as a way of administering marijuana. The CRAFFT 2.1+N version contains additional questions to address tobacco and nicotine use.
The CRAFFT screening test is administered in pediatric healthcare settings and hospital-based adolescent clinics to distinguish between high- and low-risk substance use behaviors in adolescents in the past year. The tool is also able to diagnose mild or moderate to severe substance use disorder. Additionally, the CRAFFT tool is used to determine if further assessment for substance addiction or a longer conversation about substance use context and frequency, and the risks of abusing drugs and alcohol is required.
The CRAFFT tool has demonstrated 76-92% sensitivity, 76-94% specificity, and 0.68-0.81 internal consistency, according to a 2019 article by Shenoi et al., published in the journal Pediatrics, titled “Predictive Validity of the CRAFFT for Substance Use Disorder.” Scientific evidence suggests that CRAFFT is a promising diagnostic tool to assess heavy cannabis use among adolescents, according to a 2021 article by Lee et al., published in the journal Addictive Behaviors, titled “Sensitivity and specificity of the CRAFFT to identify heavy cannabis use: Evidence from a large statewide adolescent sample.”
A baseline CRAFFT score of 2 or more is significantly associated with problematic substance use or a diagnosis of mild or moderate to severe substance use disorder (Shenoi et al., 2019). However, a CRAFFT score equal to or greater than 1 best combines sensitivity and specificity and is used as a cutoff for problematic substance use and a Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), diagnosis of mild substance use disorder at 1, 2, and 3 years.
5. TAPS screening (TAPS-1)
The Tobacco, Alcohol, Prescription medication, and other Substance use (TAPS) Tool consists of two parts: the TAPS-1 screening instrument and the TAPS-2 assessment. The TAPS-1 component is a 4-item screener that has been designed to screen for the problematic use of tobacco, alcohol, prescription medications that are used for non-medical purposes, and illegal drugs, such as cocaine, methamphetamine, marijuana, and hallucinogens, in adults in primary care settings.
These four items are questions about the past 12-month use of the four substance categories. Individuals have to respond by choosing one of the following options: never, less than monthly, monthly, weekly, and daily or almost daily. They receive a “positive” screen on TAPS-1 if they provide any response other than “never.” They are then automatically administered the TAPS-2 component. TAPS-2 identifies the specific substance being used and evaluates the severity of the individual’s substance-use behavior.
The TAPS Tool is used in an interviewer-administered format or as an online or app-based questionnaire, which is completed by the patient using the myTAPS app. The National Institute on Drug Abuse (NIDA) and the Substance Abuse and Mental Health Services Administration recommend the TAPS Tool as a screening instrument for assessing opioid and other substance use in clinical settings.
A TAPS score of 0 indicates no drug use in the previous 3 months. A score of 1 indicates problematic use, and it is recommended that further assessment of the patient be carried out to confirm or rule out risky use. A score of 2 or more indicates a high risk of substance abuse, as noted by NIDA in its web publication titled “TAPS: Tobacco, Alcohol, Prescription medication, and other Substance use Tool.” The TAPS Tool has good to excellent validity for identifying problematic tobacco, alcohol, and marijuana use and fair validity for heroin and stimulant drug misuse, according to a 2022 article by Carter et al., published in the journal Addictive Behaviors, titled “Validation of the tobacco, alcohol, prescription medication, and other substance use (TAPS) tool with the WHO alcohol, smoking, and substance Involvement screening test (ASSIST).”
For instance, it has a sensitivity of 0.92 and a specificity of 0.87 for identifying problematic tobacco use that has an elevated risk of progressing to tobacco addiction. It has a sensitivity and specificity of 0.77 (both) for identifying hazardous alcohol use, according to a 2019 article by Adam et al., published in the journal Addiction Science & Clinical Practice, titled “Electronic self-administered screening for substance use in adult primary care patients: feasibility and acceptability of the tobacco, alcohol, prescription medication, and other substance use (myTAPS) screening tool.”
The TAPS Tool has the potential to be an effective and valuable assessment tool in community pharmacy settings to screen for prescription drug addiction, especially in populations being prescribed opioid medications who have a higher risk of developing an addiction or overdosing.
6. Drug Abuse Screening Test (DAST-10)
The Drug Abuse Screening Test (DAST-10) is a brief screening tool to assess the problems related to drug use, not including tobacco or alcohol use, in the previous 12 months. The different classes of drugs included are cannabis, cocaine, stimulants, hallucinogens, barbiturates, tranquilizers, narcotics, and solvents. The test defines “drug abuse” as the use of prescription and/or over-the-counter medications or drugs in ways not indicated by the prescriber and the use of drugs for non-medical purposes.
The DAST-10 is used to assess drug abuse consequences and severity in clinical settings, formulate action plans, and evaluate treatment outcomes. The test comprises 10 questions that have to be answered with a “yes” or a “no.” A score of 0 means that the individual has reported no problems from their drug use. The degree of problems related to drug use is “low” for a score of 1-2 and warrants monitoring and reassessment at a later date. The degree is ascertained to be “moderate” for a score of 3-5, which warrants further assessment. A score of 6-8 indicates a “substantial” degree of drug use-related problems, and that of 9-10 indicates a “severe” degree of problems. All scores that indicate “substantial” and “severe” degrees of drug-related problems warrant intensive assessment. Scientific studies testify to the excellent validity and reliability of the DAST-10 test, according to a 2020 article by Shirinbayan et al., published in the journal Addiction & Health, titled “The Psychometric Properties of the Drug Abuse Screening Test.”
What is Screening, Brief Intervention, and Referral to Treatment (SBIRT)?

Screening, Brief Intervention, and Referral to Treatment (SBIRT) is a comprehensive, integrated, and evidence-based public health approach to provide early intervention and treatment services to individuals who are at risk of developing or have an existing substance use disorder, according to a 2007 article by Babor et al., published in the journal Substance Abuse, titled “Screening, Brief Intervention, and Referral to Treatment (SBIRT): toward a public health approach to the management of substance abuse.” The SBIRT is based on a universal screening approach where all members of a specific population are screened.
According to authors Thoele et al., in their 2021 article titled “Strategies to promote the implementation of Screening, Brief Intervention, and Referral to Treatment (SBIRT) in healthcare settings: a scoping review” published in the journal Substance Abuse Treatment, Prevention, and Policy, SBIRT is a three-step process. The first step involves using a screening tool to identify risky substance use and assess its severity. The second step involves delivering a brief intervention that is guided by the results of the screening process and clinical considerations. In the third stage, the patient is referred to treatment, if deemed necessary.
SBIRT has been designed to reduce the burden of injury, disability, and disease related to substance abuse, both at the individual and societal levels. Babor et al., in their 2007 article, note that the individual health benefits of SBIRT stemming from reduced drug and alcohol use are substantial and indisputable. By identifying hazardous or potentially risky patterns of substance use, it facilitates early interventions for individuals who are unlikely to seek care and therefore, go undiagnosed before a full-blown addiction takes a toll on their health and the well-being of their loved ones. At the societal level, the benefits include diminished costs from automobile accidents, workplace absenteeism and decreased productivity, arrests, and incarcerations.
Can substance abuse assessment tools be used alongside the Screening, Brief Intervention, and Referral to Treatment (SBIRT)?
Yes, substance abuse assessment tools can be used alongside the Screening, Brief Intervention, and Referral to Treatment (SBIRT). SBIRT helps to identify risky substance use and the presence of full-blown addiction in individuals. After this initial screening process, substance abuse assessment tools are used to understand the severity of the substance use patterns—the number and types of substances used, the frequency and intensity of use, and related problems and symptoms–and the potential for treatment to promote long-term abstinence.
Authors Manuel et al., in their 2015 article published in the Journal of Addiction Medicine, titled “Adapting Screening, Brief Intervention and Referral to Treatment (SBIRT) for Alcohol and Drugs to Culturally Diverse Clinical Populations” mention that SBIRT is improved by the skillful customization of brief intervention strategies and treatment referrals.
Using substance abuse assessment tools alongside SBIRT enables healthcare practitioners to gain a comprehensive understanding of the varied and interlinked aspects of an individual’s substance use problem. This additional knowledge allows them to provide or refer their patients to customized interventions that suit the latter’s unique needs and thus are effective and sustainable.


