How do drugs impact the brain: effects and role in addiction

Drugs impact the brain by modifying the structural, chemical, and functional integrity of critical regions involved in reward response, emotional regulation, self-control, learning, and memory.
The long-term effects of drug use on the brain include desensitization of the reward circuitry, impairment of chemical balance, alteration of synaptic plasticity, reduction of gray and white matter, modification of hippocampal activity, and enlargement of cerebral ventricles.
Drug use leads to addiction by impairing the normal functionality of the brain’s reward system. Repeated drug use dysregulates the dopaminergic pathways and induces tolerance and withdrawal.
How do drugs impact the brain?
Drugs impact the brain by altering its structure, chemical balance, and functionality and disrupting the pathways involved in modulating reward, emotions, self-control, learning, and memory formation. Repeated drug exposure induces neuroadaptations at the cellular and molecular levels that impair brain functions to the extent that the individual is rendered incapable of exerting control over their drug-use behaviors. The impact of drugs on the brain is highly dependent on genetic, environmental, and psycho-social factors.
What part of the brain is affected by drugs?
The parts of the brain affected by drugs are the basal ganglia, the extended amygdala, and the prefrontal cortex, according to a July 2020 release by the National Institute on Drug Abuse titled “Drugs, Brains, and Behavior: The Science of Addiction–Drugs and the Brain.” These brain regions are responsible for regulating attention, perception, reward, and emotion. Dysregulation of these processes is known to contribute to the development and maintenance of drug abuse.
The basal ganglia region is a key component of the brain’s reward circuit. In particular, two sub-regions of the basal ganglia are involved in the mechanisms of drug addiction–the nucleus accumbens and the dorsal striatum, as noted in the chapter “THE NEUROBIOLOGY OF SUBSTANCE USE, MISUSE, AND ADDICTION” in the 2016 publication by the Substance Abuse and Mental Health Services Administration (US) titled Facing Addiction in America: The Surgeon General’s Report on Alcohol, Drugs, and Health [Internet]. The nucleus accumbens is responsible for experiencing rewards or the pleasurable effects of substances and forming motivation. The dorsal striatum is involved in learning habits and routines, such as those associated with habitual drug-taking behaviors.
The extended amygdala is located below the basal ganglia. Aside from neurotransmitters involved in experiencing the positive reinforcing effects of drugs, this region includes critical components of the brain’s stress system, according to a 2009 article by George F. Koob published in the journal Brain Research, titled “Brain stress systems in the amygdala and addiction.” It controls the brain’s response to stress and negative emotions like anxiety, distress, and irritability. These emotional states are associated with drug withdrawal. Chronic drug use makes this region hypersensitive to negative emotions and feelings, and individuals feel compelled to continue using drugs just to escape the discomfort of withdrawal.
The prefrontal cortex is involved in executive functions like making decisions, controlling impulses and emotions, organizing thoughts, and planning actions. Drugs of abuse like stimulants have been found to increase activity in specific areas of the prefrontal cortex, according to a 2011 article by Rita Z. Goldstein and Nora D. Volkow published in the journal Nature Reviews Neuroscience, titled “Dysfunction of the prefrontal cortex in addiction: neuroimaging findings and clinical implications.” The result is the strengthening and reinforcement of substance-related processes like emotional responses, working memories, cravings, drug expectations, attentional bias to drug contexts, and automated behaviors. Chronic drug exposure triggers neuroadaptations that result in these neuropsychological processes suppressing processes not related to drugs, such as motivation to pursue goals that do not involve taking drugs.
How do drugs affect neurotransmitters and brain chemistry?
Drugs affect neurotransmitters and brain chemistry in two ways: by altering the concentration and functioning of dopamine in the brain or by influencing the activity of other neurotransmitters that alter how the mesolimbic dopaminergic pathway or the reward circuit of the brain functions, according to authors Denise M. Tomkins and Edward M. Sellers in their 2001 article titled “Addiction and the brain: the role of neurotransmitters in the cause and treatment of drug dependence” published in the Canadian Medical Association Journal. Neurons communicate with one another via signals that are transmitted by neurotransmitters. Dopamine is one such neurotransmitter that is implicated in the development and maintenance of addiction.
All substances of abuse increase the concentration of dopamine in the brain, according to a 2007 article by Volkow et al., published in the journal Archives of Neurology, titled “Dopamine in Drug Abuse and Addiction–Results of Imaging Studies and Treatment Implications.” Drugs like cocaine and amphetamines increase its levels by preventing the reuptake of dopamine while opioids, alcohol, and nicotine do so by triggering the release of dopamine (Tomkins and Sellers, 2001).
A majority of drugs of abuse interfere with dopamine signaling, according to a release by the Genetic Science Learning Center (University of Utah) titled “Drugs Affect Many Brain Pathways.” Impaired dopamine signaling affects several critical neural pathways including the mesolimbic pathway that is associated with memory, reward, motivation, and addiction.
Gamma-aminobutyric acid (GABA) is an inhibitory neurotransmitter that modulates the functioning of the mesolimbic dopaminergic pathway. Drugs of abuse like opioids, alcohol, and nicotine block the inhibitory effect of GABA, thereby increasing dopamine activity (Tomkins and Sellers, 2001).
Drugs affect other neurotransmitter signaling systems, such as serotonin (5-HT), norepinephrine (NE), and acetylcholine (ACh), and the endogenous opioid system, as mentioned by Sarah Davis and Jun Zhu in the chapter “Substance abuse and neurotransmission” from the book Advances in Pharmacology published in 2022. These signaling systems are associated with drug-induced neuroadaptations. For instance, amphetamines, cocaine, alcohol, and LSD (lysergic acid diethylamide) interfere with serotonin signaling. Impaired serotonin signaling is linked to depression, anxiety disorders, and obsessive-compulsive disorders, which are mental health conditions known to trigger the development of or exacerbate already existing substance abuse issues.
What are the long-term effects of drug use on the brain?
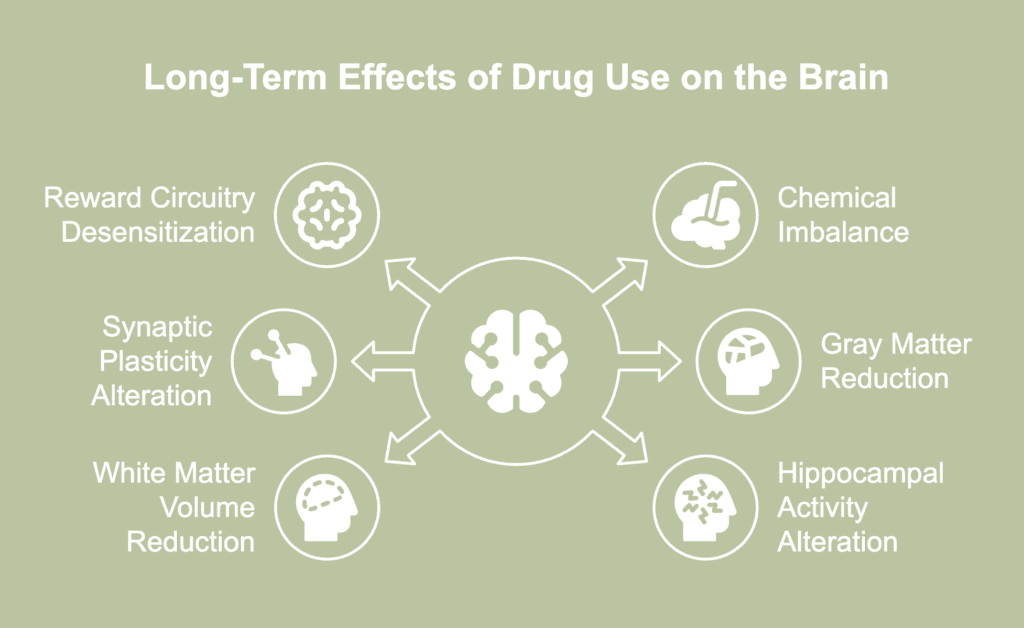
The long-term effects of drug use on the brain are listed below.
- Increased desensitization of the reward circuitry: The brain adapts to the surge of dopamine after every instance of drug use and the resulting hyperstimulation of the reward circuitry by reducing the number of dopamine D2 receptors, as explained in a 2008 article by Volkow et al., published in the journal Neuropharmacology, titled “Imaging dopamine’s role in drug abuse and addiction.” These neuroadaptations desensitize the reward circuitry, so the drug user has to take more of the substance to derive the earlier level of high. This marks the development of drug tolerance.
- Dysregulated chemical balance: Chronic drug abuse produces chemical imbalances in the brain by triggering neurons to release supranormal amounts of neurotransmitters or by interfering with the normal recycling process of these chemicals. Drug-induced chemical imbalances in the brain are implicated in multiple neural dysfunctionalities that contribute to the maintenance of addiction. For instance, neuroplastic changes triggered by dopamine imbalance are associated with increased reactivity of the brain to drug cues, decreased sensitivity to natural rewards, impaired self-regulation, and heightened sensitivity to stressful situations, according to a 2015 article by Nora D. Volkow and Marisela Morales published in the journal Cell, titled “The Brain on Drugs: From Reward to Addiction.” Drug-induced chemical imbalance is known to impair memory formation, decision-making abilities, inhibitory control, emotional regulation, and cognitive functionalities, according to a 2023 article by Rezayof et al., published in the journal Neurochemistry International, titled “Addictive drugs modify neurogenesis, synaptogenesis and synaptic plasticity to impair memory formation through neurotransmitter imbalances and signaling dysfunction.” Dysregulated chemical balance has additionally been linked with multiple physical and mental effects of drug abuse, such as tremors, abnormal heart rate, low mood, impaired sleep cycle, and disorganized thoughts.
- Altered synaptic plasticity: Substances of abuse are known to impair synaptic plasticity in critical regions of the brain, according to a 2021 article by Julian Cheron and Alban de Kerchove d’Exaerde published in the journal Translational Psychiatry, titled “Drug addiction: from bench to bedside.” One of these regions is the mesolimbic dopamine system, which is involved in the reward-processing mechanism of the brain. Experiments on animal models have shown that the synaptic adaptations in the reward circuitry triggered by long-term drug use contribute to the development of addictive behaviors, according to a 2014 article by Christian Lüscher and Robert C. Malenka published in the journal Neuron, titled “Drug-evoked synaptic plasticity in addiction: from molecular changes to circuit remodeling.” Unfortunately, synaptic adaptations induced by chronic drug abuse outlast the presence of the drug in the brain and trigger a remodeling of the neural circuitry. This development contributes to the maintenance of addiction and increases the risk of relapsing.
- Reduced gray matter: Chronic drug abuse is associated with a significant reduction in gray matter in specific regions of the brain, such as parts of the frontal cortex, the insula, and the striatum, according to a 2018 article by Mackey et al., published in The American Journal of Psychiatry, titled “Mega-Analysis of Gray Matter Volume in Substance Dependence: General and Substance-Specific Regional Effects.” Disruptions in these regions of the brain are associated with greater cravings and an increased risk of relapse, a lack of self-awareness about an addiction problem, maladaptive responses to stressors, and an inability to gauge future reward values that results in poor decision-making. The cognitive deficits associated with alterations in gray matter volume are associated with a lack of control over drug-use behaviors, according to a 2018 article by Kaag et al., published in the journal Drug and Alcohol Dependence, titled “The relation between gray matter volume and the use of alcohol, tobacco, cocaine and cannabis in male polysubstance users.” The authors suggest that the reduced volume of specific areas of the prefrontal cortex contributes to a prevalence of treatment resistance among sections of polysubstance users.
- Reduced white matter volume: Studies on individuals who chronically abuse tobacco, alcohol, cocaine, cannabis, opioids, and methamphetamine have shown lower volumes of white matter in the thalamus, which are the result of neuroadaptations to drug exposure, according to a 2021 article by Pando-Naude et al., published in the journal Translational Psychiatry, titled “Gray and white matter morphology in substance use disorders: a neuroimaging systematic review and meta-analysis.” The reduced structural and functional integrity of the thalamic region is believed to be associated with the expression of powerful cravings in response to drug cues. There is significant scientific evidence to support the role of dopamine and the reward circuitry in the development and maintenance of addiction. The above findings point to the role of drug-induced neuroplasticity in the frontocortical regions of the brain in motivating reward-seeking behaviors.
- Altered hippocampal activity: Neurogenesis refers to the production of new neurons, and the hippocampus is one of the only two regions in the brain that generates neurons well into adulthood. The hippocampus is critically involved in learning, memory, and emotional regulation. It has been found that chronic alcohol abuse reduces hippocampal volume, according to a 2017 article by Wilson et al., published in the journal Psychological Medicine, titled “Problematic alcohol use and reduced hippocampal volume: a meta-analytic review.” It is also well established that substances of abuse alter synaptic plasticity in the hippocampus, according to a 2021 article by Yosef Avchalumov and Chitra D. Mandyam published in the journal Brain Sciences, titled “Plasticity in the Hippocampus, Neurogenesis and Drugs of Abuse.” Insults to the hippocampus hamper its normal functions and thus impair critical emotional and cognitive processes.
- Enlarged cerebral ventricles: Individuals who chronically abuse alcohol and heroin have been found to have significantly enlarged ventricles compared to those who do not abuse these substances, according to a 2024 article by Montana et al., published in the journal Biomedicines, titled “Macroscopic and Microscopic Cerebral Findings in Drug and Alcohol Abusers: The Point of View of the Forensic Pathologist.” Authors Jeong et al., in their 2013 article titled “Morphometric abnormalities of the lateral ventricles in methamphetamine-dependent subjects” published in the journal Drug and Alcohol Dependence note the prevalence of lateral ventricular enlargement in methamphetamine abusers. Ventricular enlargement is associated with cerebral atrophy.
Can you get brain damage from drugs?
Yes, you can get brain damage from drugs if they are used chronically and in high doses. Long-term and heavy use of drugs is associated with severe neurological problems that last for an extended period. Substances of abuse like alcohol, cocaine, heroin, morphine, methamphetamine, and nicotine compromise the stability and functionality of the blood-brain barrier depending on dosage and route of administration, according to a 2020 article by Pimentel et al., published in the journal Frontiers in Neuroscience, titled “Effects of Drugs of Abuse on the Blood-Brain Barrier: A Brief Overview.” The result is disruptions in normal cellular function that prove to be neurotoxic. However, a majority of the brain alterations caused by substances of abuse are reversed once the drug is eliminated from the body. Drug-induced neurological issues typically do not lead to permanent brain damage.
It has been found that anhedonia, a condition where an individual is unable to find pleasure in previously rewarding activities, is associated with stimulant addiction, according to a 2010 article by Leventhal et al., published in the journal Experimental and Clinical Psychopharmacology, titled “Anhedonia Associated With Stimulant Use and Dependence in a Population-Based Sample of American Adults.” The authors believe that the condition is linked to a drug-induced dysregulation of the brain’s reward circuitry.
Although rare, hallucinogen abuse has been found to trigger the development of hallucinogen persisting perception disorder (HPPD). It is a long-lasting neurological disorder characterized by visual hallucinations that have the possibility of causing significant distress and/or impairment of an individual’s ability to function normally.
Wernicke-Korsakoff Syndrome (WKS) is a severe neurological complication of brain impairment caused by alcohol abuse. One of its syndromes, Wernicke encephalopathy, is a short-term condition that is cured if treatment begins early. This condition is marked by symptoms like impaired muscle coordination, paralysis of specific eye nerves, and confusion. The other syndrome, Korsakoff’s psychosis, has the potential to cause long-term and irreversible memory and learning difficulties, and even death in severe cases.
Severe brain damage resulting from the direct use of drugs of abuse is noted in a percentage of overdosing cases. The damage is usually caused by hypoxia where oxygen supply to the brain is hampered. Hypoxia is triggered when the respiratory rate is reduced to dangerously low levels, a development commonly associated with overdosing cases involving opioids, alcohol, benzodiazepines, and other sedatives. Hypoxic brain damage manifests as symptoms like memory impairment, stroke, seizures, mental confusion, impaired body movement, weakened motor abilities, paralysis of the legs, and slowed reactions. These symptoms are transient or permanent.
Drugs have the ability to cause brain damage indirectly. Traumatic brain injury (TBI) and drug addiction frequently co-occur. Substance abuse is associated with risk-taking and impulsive behaviors, cognitive deficits, poor motor control, and loss of inhibition that increase the risk of an individual being involved in serious falls and/or vehicular accidents, according to a 2012 article by Olson-Madden et al., published in the journal Rehabilitation Research and Practice, titled “Substance Use and Mild Traumatic Brain Injury Risk Reduction and Prevention: A Novel Model for Treatment.” Individuals are known to engage in violent or aggressive behaviors or become victims of crimes under the influence of substances. These events raise their risk of sustaining injuries that damage the brain.
How can one reverse brain damage from drugs?
One can reverse brain damage from drugs by undergoing and continuing treatment, practicing prolonged abstinence, exercising regularly, eating a nutritious diet, practicing mindfulness exercises, and establishing good sleep hygiene. For instance, a limited number of studies show that engaging in physical exercise improves inhibitory control and increases activity in the prefrontal cortex, the seat of executive controls, in substance users, according to a 2019 article by Costa et al., published in the journal Frontiers in Psychiatry, titled “Rewiring the Addicted Brain Through a Psychobiological Model of Physical Exercise.”
Mindfulness-based interventions have been shown to strengthen the cognitive, affective, and neural circuits impaired by prolonged drug use, according to a 2018 article by Priddy et al., published in the journal Substance Abuse and Rehabilitation, titled “Mindfulness meditation in the treatment of substance use disorders and preventing future relapse: neurocognitive mechanisms and clinical implications.” A nutritious and balanced diet, especially one rich in omega-3 fatty acids, is known to promote neural repair after brain insults.
Does the brain heal after using drugs?

Yes, the brain heals after using drugs in a majority of instances if abstinence is followed and therapy is continued. Authors Hampton et al., in their 2019 article titled “Substance Abuse and White Matter: Findings, Limitations, and Future of Diffusion Tensor Imaging Research” published in the journal Drug and Alcohol Dependencenote that abstinence has been shown to partially reverse drug-induced changes in white matter in nicotine, cocaine, and cannabis users.
Alcohol abuse is known to cause a reduction in the volume of cortical grey matter. It has been shown that abstinence led to an increase in grey matter volume in a sample of individuals who abused alcohol, according to a 2013 article by Garavan et al., published in the journal Current Opinion in Neurobiology, titled “The Neurobiology of Successful Abstinence.” Authors Volkow et al., in their 2001 article titled “Loss of Dopamine Transporters in Methamphetamine Abusers Recovers with Protracted Abstinence” published in the Journal of Neuroscience note that prolonged abstinence is known to partially restore dopamine transporter levels in the brains of a sample of methamphetamine users. The extent of brain recovery after a period of using drugs depends on the type of damage, the nature of the substance being abused, the magnitude and duration of abuse, and how soon therapy is initiated.
How long does it take for the brain to heal?
There is no scientific consensus on how long it takes for the brain to heal after using drugs. The timeline depends on the nature of the substance abused, the magnitude and duration of drug use, the nature and extent of initial impairment, the presence of a co-occurring mental illness, the individual’s general health status, and whether they are undergoing treatment. The age of the individual is a critical variable. It has been found that three weeks of abstinence reversed brain shrinkage to a greater degree in younger individuals with alcoholism than older subjects, according to a 2013 article by Garavan et al., published in the journal Current Opinion in Neurobiology, titled “The Neurobiology of Successful Abstinence.” Healing tended to occur more rapidly during the first month of abstinence compared to the rates observed in the next 6-9 months.
How does drug use lead to addiction in the brain?
Drug use leads to addiction in the brain via drug-induced neuroadaptive mechanisms that alter brain structures and interfere with normal neural functioning with consequent behavioral implications, as explained in the chapter “THE NEUROBIOLOGY OF SUBSTANCE USE, MISUSE, AND ADDICTION” in the 2016 publication by the Substance Abuse and Mental Health Services Administration (US) titled Facing Addiction in America: The Surgeon General’s Report on Alcohol, Drugs, and Health [Internet]. These neural changes drive the shift from controlled and occasional drug taking to compulsive and impulsive drug use, a hallmark of addiction.
The brain’s reward system and addiction are implicitly linked. Substances of abuse exert their initial reinforcing effects by producing a surge of dopamine after taking a drug, resulting in feelings of intense pleasure. Drugs of abuse affect the brain significantly more than natural rewards. This supraphysiological stimulation of the reward circuitry is perceived as highly salient, according to a 2008 article by Volkow et al., published in the journal Neuropharmacology, titled “Imaging dopamine’s role in drug abuse and addiction.” The perception of salience drives attention, triggers arousal, and conditions the brain to form positive associations between drugs and pleasure. This conditioned learning motivates future drug-seeking behaviors.
Repeated exposure to drugs desensitizes the brain’s reward circuitry. Chronic drug users have fewer dopamine receptors and reduced dopamine function than those who do not take drugs. This results in drug users needing to take more of the drug to feel the earlier level of high, a state known as drug tolerance. Drug tolerance drives increased use of drugs. Chronic and repeated administration of drugs causes the body to adapt to the presence of the substance. So, uncomfortable withdrawal symptoms arise when drug use is reduced or suspended, a state that indicates dependence. Drug users feel compelled to continue using drugs to escape the pain and discomfort of withdrawal. This marks the transition from impulsive to compulsive use of substances. Compulsive drug use is a hallmark of addiction.
Reduced dopamine functionality also results in impaired functioning of specific regions of the brain, such as the orbitofrontal cortex, the dorsolateral prefrontal cortex, and the cingulate gyrus (Volkow et al., 2008). Disruptions in these regions manifest as compulsive and impulsive drug-use behaviors and impairment of executive functions, the latter resulting in cognitive deficits. Authors Rezayof et al., in their 2023 article published in the journal Neurochemistry International, titled “Addictive drugs modify neurogenesis, synaptogenesis and synaptic plasticity to impair memory formation through neurotransmitter imbalances and signaling dysfunction,” state that the transition from drug use to drug dependence is associated with cognitive deficits like poor decision-making ability, impaired control over drug use, and impaired memory formation.
How long does it take for the brain to become dependent on drugs?
There is no established timeline for the brain to become dependent on drugs. It is possible for an individual to develop dependence after using drugs for only a short time, according to a 1987 article by Miller et al., published in the Journal of Substance Abuse Treatment, titled “The relationship of addiction, tolerance, and dependence to alcohol and drugs: a neurochemical approach.” The time it takes for the brain to become dependent on drugs is influenced by factors like the nature of the substance used, its route of administration, the age of onset of drug use, the presence of a mental illness in the individual, their genetic makeup, and their history of trauma.
How does drug tolerance affect the brain?
Drug tolerance affects the brain through associated neuroadaptive mechanisms that increase the risk of developing chemical dependence on substances of abuse. The development of tolerance is characterized by the desensitization of the brain’s reward system, according to a 2002 article by Roy A. Wise, published in the journal Neuron, titled “Brain Reward Circuitry: Insights from Unsensed Incentives.” When an individual develops drug tolerance, they need more of the substance or need to take it more frequently to experience the earlier level of high.The development of tolerance is a manifestation of the body’s attempt to achieve homeostasis by compensating for the imbalance of neurotransmitters.
Besides the gradual reduction in the effect of the drug, other neural adaptations follow the development of tolerance. These adaptations manifest as increased sensitivity to even minute alterations in drug dose; the emergence of the rebound phenomenon; and significant negative reactions to drug withdrawal in dependent populations, as noted by Abraham Peper in a 2004 article titled “A theory of drug tolerance and dependence I: a conceptual analysis” published in the Journal of Theoretical Biology. When drug tolerance develops, impulsive drug use becomes compulsive drug taking because the individual now uses drugs to escape the discomfort of withdrawal.
How do drugs affect mental health?

Drugs affect mental health by triggering changes in brain structure and functionality characterized by the manifestation of short- and long-lasting psychiatric symptoms. All drugs of abuse alter an individual’s perception of objects and experiences, their moods, and behavioral responses.
In vulnerable populations, drug use is known to contribute to the development of serious mental disorders, such as generalized anxiety disorder, manic depression, schizophrenia, and panic disorder, or the aggravation of the symptoms of an existing mental illness. Children and adolescents who use drugs are particularly vulnerable to negative mental health outcomes later in life, such as the development of full-blown addiction or occurrence of a mental illness, according to a 2020 release by the National Institutes on Drug Abuse (US) titled “Common Comorbidities with Substance Use Disorders Research Report.”


