21 different addiction types: physical, behavioral, and impulse control disorders
Table of content
- What are the types of physical addiction?
- What are the types of behavioral addiction?
- What are the types of impulse control disorder?
- How does addiction treatment change based on addiction type?
- How to understand which addiction type you have?
- Do addiction symptoms change based on addiction type?
- Which addiction type is the most dangerous for financial well-being?
- Which addiction type is the most dangerous for physical well-being?
- Which addiction type is the most dangerous for psychological well-being?
- Which addiction type is the most dangerous for social well-being?

Addiction type is the division or classification of addictive behaviors according to several criteria, including the substance or activity, the behavioral pattern, and the psychological or physiological consequences on the individual.
The three main addiction types are physical addiction, behavioral addiction, and impulse control disorders.
Physical addiction occurs when the body becomes so dependent on a substance to the point of experiencing withdrawal symptoms without it. The substance alters brain chemistry, creating a physical need to continue using to feel normal.
Behavioral addiction is a compulsion to engage in rewarding non-substance-related behaviors despite negative consequences. Addictive behaviors lead to dependence and provide emotional relief or pleasure by activating the same brain circuits as substance addiction.
Impulse control disorders (ICDs) are conditions involving difficulty resisting impulses or urges, resulting in harmful outcomes. ICDs cause significant distress or impairment in daily functioning.
What are the types of physical addiction?
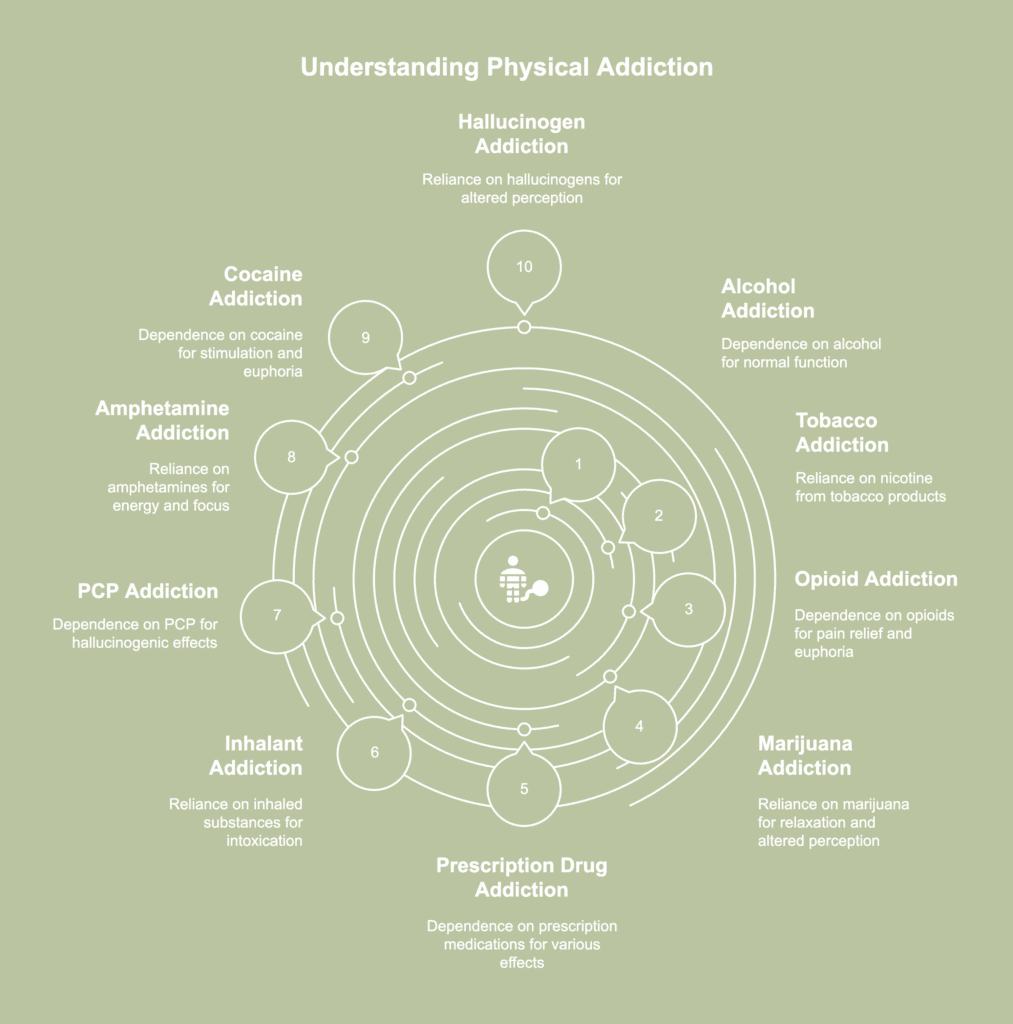
Physical addiction refers to disorders characterized by chronic or persistent use of tolerance-forming drugs and addictive substances. Types of physical addiction refer to different forms of substance dependence involving a chemical reliance of the body on certain drugs to function normally. The types of physical addiction are listed below.
- Alcohol addiction
- Tobacco addiction
- Opioid addiction
- Marijuana addiction
- Prescription drug addiction
- Inhalant addiction
- PCP addiction
- Amphetamine addiction
- Cocaine addiction
- Hallucinogen addiction
1. Alcohol addiction
Alcohol addiction involves compulsive alcohol drinking, leading to loss of control over intake and causing various health and life-quality issues. Regular consumption of alcoholic beverages increases susceptibility to becoming physically addicted due to the potential for developing dependence.
Alcoholism is associated with harm to important organs, including the liver, heart, kidney, and digestive system. Unhealthy alcohol use weakens the immune system, alters brain activity, and fuels long-term cognitive deterioration.
The causes of alcohol addiction include genetic, psychological, physiological, and social factors, as well as psychological characteristics, like impulsivity, low self-esteem, and a need for validation, according to a 2012 article titled “Understanding alcohol use disorders and their treatment” published by the American Psychological Association.
Alcohol addiction treatment often involves medications, behavioral treatments, and mutual-support groups, as per a publication titled “Understanding Alcohol Use Disorder” last updated in January 2025 by the National Institute on Alcohol Abuse and Alcoholism.
The article mentioned the United States Food and Drug Administration (FDA) has currently approved three medications with the purpose of assisting individuals in reducing alcohol consumption and averting symptom recurrence or relapse: disulfiram, acamprosate, and naltrexone (oral and long-acting injectable formulations).
Each nonaddictive medication is used independently or in combination with behavioral therapies or peer groups.
Help is available for individuals struggling with alcoholism through a variety of treatment centers focusing on the condition. Alcohol treatment facilities offer a safe, controlled setting for people to successfully detoxify from alcohol.
2. Tobacco addiction
Tobacco addiction, often classified as nicotine dependence or tobacco use disorder, is the strong reliance on tobacco products resulting from nicotine’s addictive qualities. The main psychoactive ingredient in cigarette smoke, nicotine, produces pleasant feelings, making people more susceptible to being addicted to nicotine.
Chronic obstructive pulmonary disease (COPD), encompassing conditions like emphysema and chronic bronchitis, is brought on by smoking, along with diabetes, cancer, heart disease, stroke, and lung disorders, as stated in a 2024 article titled “Cigarette Smoking” published by the Centers for Disease Control and Prevention.
Nicotine’s pharmacokinetic properties, or the way it is metabolized in the body, play a role in causing tobacco addiction, as per a 2020 report titled “Is nicotine addictive?” from the National Institute on Drug Abuse (NIDA).
The main courses of treatment for nicotine addiction are counseling and nicotine replacement therapy. Tobacco addiction treatment centers are available, encompassing specialized divisions like pulmonary rehabilitation units or smoking cessation clinics.
3. Opioid addiction
Opioid addiction is characterized by compulsive drug-seeking and use of opioids, prescription pain medication, and illicit narcotics such as heroin despite negative consequences and withdrawal effects after cessation.
According to a 2019 paper by Wang et al., titled “Opioid Addiction, Genetic Susceptibility, and Medical Treatments: A Review,” opioid addiction impairs cognitive and behavioral functioning, with effects persisting beyond the cessation of opioid use.
Furthermore, long-term addiction has disruptive effects to the brain’s intellectual abilities, leading to poor judgment and making relationships and stable employment challenging to sustain.
Reasons for opioid addiction include environmental, genetic, and lifestyle factors. Methadone, buprenorphine, and naltrexone are the three primary drug options available to treat opioid addiction.
These drugs are taken in conjunction with family and friend assistance and counseling, according to a 2020 American Society of Addiction Medicine publication titled “Opioid Addiction Treatment: A Guide for Patients, Families and Friends.”
Opioid addiction treatment facilities are intended to provide assistance to clients throughout the entirety of the recovery process. Treatment programs often begin with medical detoxification, involving supervised withdrawal from opioids to manage acute symptoms safely.
4. Marijuana addiction
Marijuana addiction is a disorder associated with chronic relapse caused by compulsive marijuana use and intake despite detrimental effects and withdrawal symptoms when deprived of the drug.
The addictive nature of marijuana stems from tetrahydrocannabinol (THC), the main psychoactive compound affecting the brain’s reward system and encouraging continued use.
Weed, a common term for marijuana, has been linked to significant cognitive impairments, particularly affecting memory, attention, and decision-making, as highlighted in a 2018 report titled “Cannabis Addiction and the Brain: a Review” by Zehra et al.
In addition, the substance has an impact on the regulation of emotions, elevating the susceptibility to mood disorders including anxiety and depression. Prolonged cannabis use is associated with the development of “amotivational syndrome,” characterized by diminished motivation and interest in formerly pleasurable activities.
The causes of marijuana addiction include genetics, early use, preexisting mental health conditions, and environmental influences.
Treatment for marijuana disorders include behavioral treatments, such as cognitive behavioral therapy (CBT), contingency management, and motivational enhancement therapy, as well as medications, as per a 2024 report titled “Cannabis (Marijuana)” from the National Institute on Drug Abuse.
While marijuana addiction treatment centers are not as prevalent as institutions for substances like alcohol or opioids, there are facilities and programs available specifically designed to address marijuana addiction.
Treatment centers understand marijuana, though often viewed as less harmful than other substances, causes dependency in certain individuals, leading to negative life consequences.
5. Prescription drug addiction
Prescription drug addiction is described as the compulsive use and misuse of prescription medication, usually prescribed for the treatment of mental health conditions or pain management, in excess of the recommended dosages.
Benzodiazepine addiction serves as one example of this type of physical addiction, involving compulsive misuse of benzo medications beyond prescribed doses and resulting in physical and psychological dependence.
Prescription drug addiction results in physical health complications, such as respiratory depression, cardiovascular problems, liver damage, and an increased risk of overdose, particularly with opioids and sedatives.
The condition damages a person’s mental health as well, contributing to symptoms of anxiety, depression, paranoia, and cognitive impairment. Addiction to prescription drugs strains relationships with family, friends, and colleagues, as individuals prioritize obtaining and using drugs over responsibilities and personal connections.
Reasons behind addiction to prescription drugs are to experience the “high” effect, relax, alleviate tension, or peer influence and pressure, while others take them to be more productive.
Treatment options for prescription drug addiction include detoxification and counseling. Treatment centers or rehabs specializing in addiction to prescription medicine are available to help individuals recover.
6. Inhalant addiction
Inhalant addiction, otherwise known as inhalant misuse, is the intentional inhalation of vapors by sniffing from chemical products to become intoxicated or achieve a “high” effect.
Inhalants are volatile chemical vapors creating a mind-altering effect when inhaled. Fuel, adhesives, varnishes, dry cleaning agents, deodorants, hair sprays, paint thinners, paint removers, dry cleaning fluids, glues, typewriter correction fluids, and gasoline are among several inhalant-containing products, according to a 2008 study titled “Inhalant abuse: A clinic-based study” by Kumar et al.
The study mentioned inhalants quickly enter the bloodstream through the lungs after inhalation; the chemicals then exert toxic effects on the brain and other organs, leading to intoxication in the user. Hallucinations, delusions, and lightheadedness emerge.
The causes of inhalant addiction include genetics, family history of abusing drugs, a personal history of mental illness or chronic substance abuse, and social and environmental factors.
Types of treatment for inhalant use disorder includes medical detoxification, inpatient rehabilitation, and outpatient programs.
According to a study by Howard et al., published in July 2011 titled “Inhalant Use and Inhalant Use Disorders in the United States,” there is a severe lack of treatment programs specifically designed for inhalant addiction in the United States.
During the investigation, only one program, the Tundra Swan Inhalant Treatment Program, was operational at the McCann Treatment Center in Bethel, Alaska. The Yukon-Kuskokwim Health Corporation manages the facility. A maximum of 19 young individuals between the ages of 10 and 18 are accommodated at a given time.
Most participants primarily come from rural communities in Alaska. Treatment programs encompass conventional indigenous cultural traditions, such as indigenous dancing, crafts, and sweat lodges, along with extensive family engagement.
7. PCP addiction
PCP addiction is characterized by the excessive and uncontrollable consumption of phencyclidine, a potent hallucinogenic drug initially created as an anesthetic but now predominantly used for recreational purposes.
PCP, otherwise known as angel dust, induces hallucinations, distorted perceptions of reality, and feelings of detachment from oneself and the environment.
Reasons for PCP addiction include genetics, trauma, environmental influences, life stressors, imbalances in brain chemicals, mental health disorders, lack of social support, and peer pressure.
PCP addiction treatment options include medication to relieve withdrawal symptoms in an inpatient program and behavior modification strategies through counseling (talk therapy), according to an article titled “Substance use – phencyclidine (PCP)” last reviewed in May 2024 by MedlinePlus.
PCP addiction treatment facilities and rehabs help individuals battling with the condition. The complex nature of PCP addiction and the severity of consequences have led clinics to design comprehensive programs tailored specifically for affected individuals.
8. Amphetamine addiction
Amphetamine addiction is a condition associated with the compulsive use of a highly addictive stimulant, amphetamine, and the presence of withdrawal symptoms upon cessation.
In certain cases, people think amphetamine is the same as methamphetamine—another stimulant drug. Although the two are related in a sense that both are part of the amphetamine class of drugs, they are not exactly the same.
Both have licit types, but methamphetamine is significantly more powerful than amphetamines and is more frequently produced, sold, and used illegally. Meth is rarely used for medical purposes, making methamphetamine addiction a more dangerous type of addiction.
Amphetamine use induces euphoria, heightens alertness, and boosts energy and confidence. According to a 2019 paper by McKetin et al., titled “Mental health outcomes associated with of the use of amphetamines: A systematic review and meta-analysis,” amphetamine addiction causes harmful effects in the body and the brain, namely increased level of psychosis, depression, suicidality, and heightened level of interpersonal violence.
The causes of amphetamine addiction include changes in brain chemistry, easy access to amphetamines, co-occurring mental health disorders, and life stressors.
Treatments for amphetamine use disorder include behavioral therapies, medications for severe withdrawal symptoms, addiction education, and peer support groups.
Amphetamine addiction treatment centers are readily available and essential for people struggling with the chemical abuse. Such facilities provide individualized programs to assist people in overcoming the condition.
9. Cocaine addiction
Cocaine addiction is the obsessive use of cocaine despite medical, psychological, and behavioral repercussions.
Repeated cocaine use causes acute kidney and liver problems, worsens cardiovascular and respiratory diseases, and induces psychiatric comorbidities such as mood disorders, anxiety, and suicidal ideation.
Social pressure, existing mental health problems, and genetics are the potential reasons people use cocaine and develop an addiction. A shared environment highly influences cocaine dependence and increases the risk of substance abuse disorder as well.
Treatment of cocaine addiction is possible through pharmacological and behavioral treatments. Inpatient and outpatient treatment centers and programs are available.
10. Hallucinogen addiction
Hallucinogen addiction is a type of substance addiction revolving around the compulsive use of hallucinogens, such as PCP, ketamine, and LSD, altering an individual’s awareness of their surroundings, thoughts, and feelings.
According to a 2022 review by Schlag et al., titled “Adverse effects of psychedelics: From anecdotes and misinformation to systematic science,” the potential negative psychological side effects of hallucinogens, include anxiety attacks, paranoia, and, in rare instances, chronic mental illnesses like Hallucinogen Persisting Perception Disorder (HPPD), a condition causing users to have flashbacks and visual abnormalities long after the drug’s effects have worn off.
Causes of hallucinogen addiction include genetic predispositions, differences in brain chemistry, environmental influences, lack of healthy coping mechanisms, underlying mental health conditions, and cultural attitudes towards drug use.
Treatments for hallucinogen addiction are medication-assisted treatment (MAT), behavioral therapies, and support groups.
Specialized treatment centers for individuals addicted to hallucinogens play a significant role in addressing the chemical dependency. People in such facilities receive personalized plans designed to end hallucinogen use and restore control over life.
What are the types of behavioral addiction?
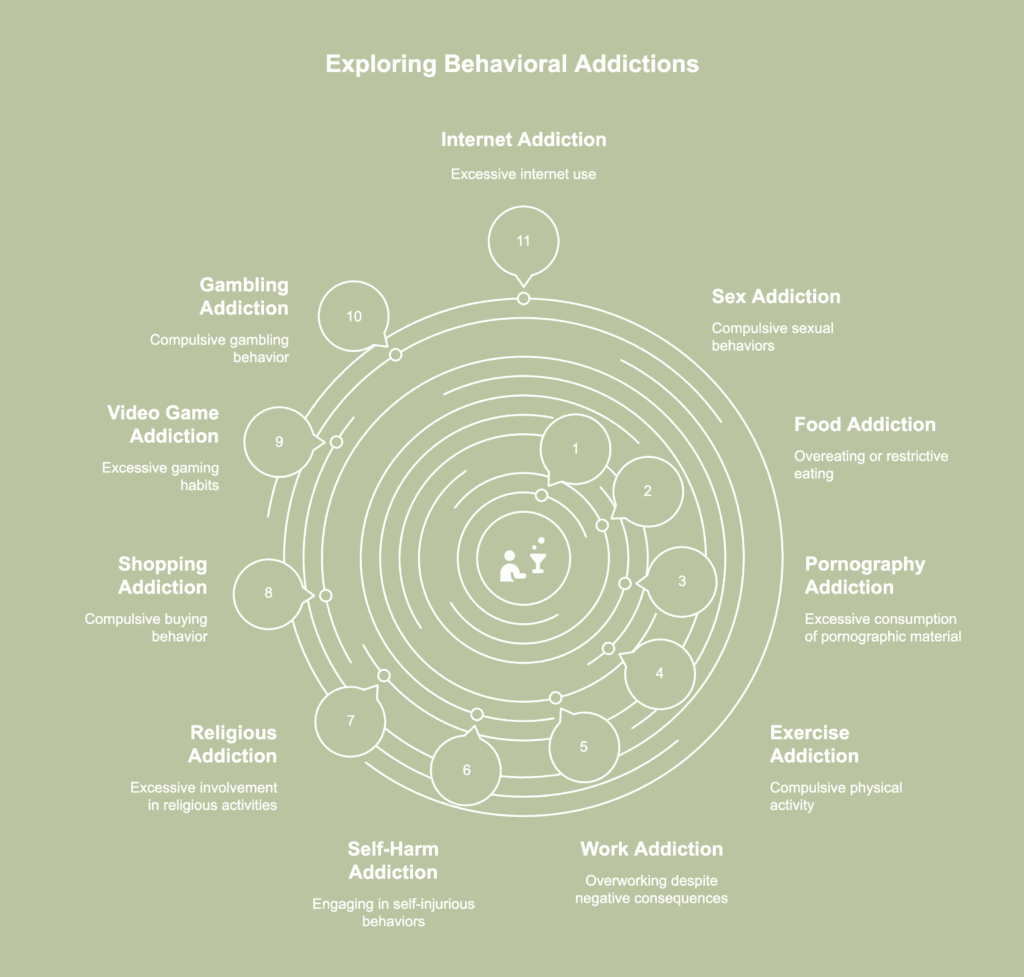
Behavioral addictions refer to compulsive engagement in repetitive, non-substance-related behaviors that are difficult to control and continue despite harmful effects. Types of behavioral addiction include a variety of obsessive behaviors producing psychological benefits and cause recurrent involvement in spite of negative outcomes. The types of behavioral addiction are listed below.
- Sex addiction
- Food addiction
- Pornography addiction
- Exercise addiction
- Work addiction
- Self-harm addiction
- Religious addiction
- Shopping addiction
- Video game addiction
- Gambling addiction
- Internet addiction
1. Sex addiction
Sex addiction is a psychiatric disorder characterized by uncontrollable sexual thoughts, urges, and impulses acted upon to achieve a “fix” comparable to what a person with substance abuse gets from consuming a particular drug or alcohol.
Sex addiction has a profound impact on the affected individual, causing impact on relationships, intense feelings of guilt, shame, and low self-esteem, unintended pregnancies, sexually transmitted infections (STIs), decreased productivity at work, and legal issues.
The causes of sex addiction include neurotransmitter imbalance, damage to brain regions mediating human sexual behavior, emotional dysregulation, family dysfunction, childhood abuse, and adverse effects of certain medications.
Treatment for sex addiction often involves medications, psychotherapy, and self-help groups. The primary objective of treatment is to assist a patient in effectively controlling impulses and diminishing problematic behaviors, all while maintaining the ability to engage in healthy sexual activities and relationships.
Facilities specifically designed for individuals with sex addiction provide support. Programs aim to address the root causes of compulsive sexual behavior and help clients achieve recovery.
2. Food addiction
Food addiction is a behavioral addiction wherein a person becomes dependent on highly palatable foods, has intense cravings, and experiences difficult-to-control urges to eat food.
As per a 2021 study by Octavian Vasiliu, titled “Current Status of Evidence for a New Diagnosis: Food Addiction-A Literature Review,” food addiction has been linked to a multitude of health complications, encompassing psychological and psychiatric issues (e.g., diminished self-esteem, major depressive disorder, and binge eating disorder), somatic complications (e.g., obesity or overweight status, metabolic imbalances, diabetes mellitus, or cardiovascular diseases), and social concerns (e.g., apprehension of social stigmatization associated with obesity or overweight status or addictive-like behavior).
The study explained a variety of complex factors contributing to food addiction, such as modifications in brain chemistry and function, genetics, mental conditions like depression or stress, and the presence of extremely appetizing foods in one’s immediate surroundings.
Due to the complicated and multifaceted nature of food addiction and its intricate bio-psycho-social etiology, an integrated therapeutic approach involving psychotherapy, medication, and social support is necessary.
Clinics intended to treat addictive eating behavior have specific programs meant to help people break unhealthy eating habits and build a healthier relationship with food.
3. Pornography addiction
Compulsive consumption of pornographic material despite harmful effects on relationships, mental health, and daily life describes the behavioral problem known as pornography addiction.
Porn addiction frequently impairs emotional health and causes emotions of guilt, humiliation, or anxiety due to excessive consumption. Relationships, interest in actual physical intimacy, and day-to-day functioning are all negatively impacted by the condition over time.
Reasons for porn addiction include underlying mental health conditions, relationship issues, unhealthy cultural norms, and biological factors.
Treatment methods for pornography addiction include therapy, medication, support groups, lifestyle changes, and couples’ counseling.
Specialized institutions offer assistance to individuals addicted to pornography. Clinics focus on recovery through personalized remedies targeting underlying causes of the condition.
4. Exercise addiction
Exercise addiction (EA) is a behavioral addiction indicated by compulsive engagement in any type of physical exercise despite harmful consequences. Exaggerated training affects a person both physically and mentally.
Excessive exercise causes physical injuries, psychological distress interfering with self-worth and image, and eating disorders.
Exercise addiction is often brought on by a number of factors, such as stress or unpleasant emotions, the activation of the brain’s reward system, social pressure to maintain a particular body type or level of fitness, and problems with body image, as per a 2023 study by Aviv Weinstein and Attila Szabo, titled “Exercise addiction: A narrative overview of research issues.”
Typically, cognitive-behavioral therapy is advised for most behavioral addictions. Additionally, alternative behavioral approaches like contingency management provide rewards for abstaining from a specific exercise or reducing the intensity of a previously addictive behavior.
Facilities geared at treating exercise addiction offer specific assistance. Individuals are assisted in managing the issues leading to compulsive exercise habits through the implementation of programs.
5. Work addiction
Work addiction, otherwise known as workaholism, is a behavioral addiction characterized by an obsessive preoccupation with work, often to the detriment of one’s health, relationships, and overall well-being.
A person with work addiction experiences chronic stress, exhaustion, sleep difficulties, decreased productivity, headaches, anxiety, depression, burnout, and decreased life satisfaction.
The causes of work addiction include perfectionistic tendencies, high levels of conscientiousness, cultural norms glorifying overwork, a strong need for achievement, underlying psychological issues such as low self-esteem, anxiety, depression, and traumatic experiences or family dynamics during childhood.
Psychotherapy, counseling, and lifestyle modifications are commonly used in the treatment of workaholism with the goal of treating the root reasons of addiction and fostering a better work-life balance.
While treatment facilities or rehabs specifically for work addiction are not as prevalent as centers for substance addictions, specialized programs and therapists trained in treating behavioral addictions like work addiction are available.
6. Self-harm addiction
Self-harm addiction, otherwise known as non-suicidal self-injury (NSSI) addiction, refers to a compulsive pattern of deliberately inflicting harm to oneself as a way of coping with emotional distress or regulating overwhelming emotions.
Self-harm is not officially recognized as a diagnosis in psychiatric classification systems like the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5).
The effects of self-harming behavior on a person include physical injuries, including cuts, bruises, burns, and broken bones, exacerbation of mental health problems, being withdrawn, strained relationships with loved ones, and feelings of guilt, shame, and low self-esteem.
Suicidal behavior (SB) sometimes coexist with self-harming tendencies, complicating the individual’s emotional state and increasing the need for intervention.
Factors contributing to self-harm addiction include experiencing trauma, abuse, or neglect during childhood or adolescence, underlying mental health conditions, genetic predispositions, exposure to self-harm behaviors, and peer pressure.
Treatments for NSSI addiction include psychotherapy, support groups, medication, and inpatient care for more severe cases.
Treatment facilities specialize in assisting with addictive behaviors including self-harm and associated mental health problems. People are able to focus on overcoming self-harm addiction and begin laying a road toward long-term rehabilitation in specialized institutions because of the kind and encouraging environment.
7. Religious addiction
Religious addiction is the unhealthy fixation with religious doctrine, customs, or rituals to the extent of interfering with daily living and general well-being. While faith offers numerous individuals guidance and comfort, religious addiction shows up as a strong and compulsive connection to religious activities interrupting daily life and personal relationships.
Among the consequences of religious addiction are social isolation and withdrawal, guilt, anxiety, perfectionism, black-and-white thinking, and self-care neglect.
The causes of religious addiction include a history of trauma or abuse, cultural and familial influences, existential concerns, and certain personality traits, like perfectionism and scrupulosity.
A combination of psychotherapy, counseling, and support groups are commonly used in the treatment of religious addiction with the goal of resolving the underlying psychological and emotional issues fueling the addiction.
Although specific treatment facilities exclusively for religious addiction are unavailable, individuals often seek assistance from mental health professionals, religious counselors, or support groups addressing religious obsession and fanaticism.
8. Shopping addiction
Shopping addiction, otherwise known as compulsive buying behavior (CBB), is an inability to control the urge to make purchases constantly. People with shopping addiction shop to cope with stress and anxiety, relieve boredom, and indulge in the excitement incited by purchase.
Shopping addiction severely impacts finances and often involves compulsive collecting. Emotional struggles, mental health challenges, and external environmental factors contribute to the development of the condition.
Results of a 2022 report by Octavian Vasiliu, titled “Therapeutic management of buying/shopping disorder: A systematic literature review and evidence-based recommendations” demonstrated how successful cognitive behavioral therapy (CBT) is when used as the main intervention for compulsive buying/shopping disorder (CBSD).
Additionally, evidence exists supporting the use of CBT in conjunction with antidepressants as well as serotonergic antidepressants alone.
Offering a safe environment to examine spending patterns and build better financial management skills, shopping addiction treatment centers specialize in addressing problems with obsessive buying and overspending.
9. Video game addiction
Video game addiction or internet gaming disorder is indicated by persistent and dysfunctional engagement in video games, causing both physical and mental distress.
Video game addiction has various detrimental effects, such as diminished self-esteem and life satisfaction, inadequate social support, disrupted sleep patterns, poor academic performance, impaired clinical attention, compromised episodic and working memory, impaired problem-solving abilities, and diminished writing and speaking skills, according to a 2023 review by Limone et al., titled “The epidemiology and effects of video game addiction: A systematic review and meta-analysis.”
The reasons for addictive gaming include underlying mental health conditions like anxiety or depression, availability of gaming gadgets, high-speed internet access, societal conventions looking at gaming as entertainment, genetic predispositions, and variations in brain chemistry.
A combination of psychotherapy, counseling, behavioral treatments, and lifestyle modifications are often used in the treatment of video game addiction with the goal of addressing the root causes of the addiction and creating more healthy coping mechanisms.
Dedicated treatment facilities or rehabs exclusively for video game addiction offer a compassionate and empathetic environment for individuals to address persistent gaming habits, cultivate healthier gaming behaviors, and strive for a more balanced lifestyle.
10. Gambling addiction
Gambling addiction, otherwise known as pathological gambling or compulsive gambling, is a behavioral addiction marked by an irresistible compulsion to gamble notwithstanding adverse outcomes.
Disordered gambling leads to financial troubles, debt, bankruptcy, loss of savings, guilt and humiliation, interpersonal disputes, legal issues, sleep disruptions, and stress-related illnesses.
Genetic predisposition, parental gambling, latent mental health conditions, exposure to gambling opportunities, social norms glorifying gambling, peer pressure, and intense competitiveness are all contributors to gambling addiction.
A multifaceted treatment approach is frequently necessary for gambling disorder (GD); treatment options include cognitive behavioral therapy (CBT), motivational interviewing (MI), pharmacotherapy, and dietary and lifestyle modifications, according to a 2014 study by Sarah W. Yip and Marc N. Potenza, titled “Treatment of Gambling Disorders.”
The study noted cognitive behavioral therapy (CBT) and motivational interviewing serve as effective alternatives to medication, especially for patients opting not to undergo pharmacological treatment.
Treatment facilities solely for gambling addiction offer a compassionate and empathetic setting for individuals to address gambling habits, cultivate healthier behaviors, and progress toward a life free from addiction.
11. Internet addiction
Internet addiction refers to an excessive and compulsive dependence on internet-related activities, leading to significant impairment in various aspects of life. Individuals with internet addiction spend excessive amounts of time online, neglecting personal, social, and occupational responsibilities in favor of internet use.
Problematic internet use (PIU) leads to social disengagement and seclusion, compromised performance in school or work, obesity, eye strain, sleep disturbances, emotional turmoil, and monetary difficulties.
Sociocultural factors (such as demographics, acceptance of and access to the Internet), biological vulnerabilities (such as genetics, abnormalities in neurochemical processes), and psychological predispositions (such as personality traits, negative affects) are among the factors contributing to internet addiction, as per a study by Cash et al., published in November 2012 with the title “Internet Addiction: A Brief Summary of Research and Practice.”
Psychological methods like motivational interviewing, group therapy, and cognitive-behavioral therapy (CBT) as well as pharmacological treatments using SSRIs and other drugs were examined in the study.
Among treatment options, CBT remains the most commonly recommended approach, focusing on changing internet use behaviors and addressing thoughts contributing to internet addiction disorder (IAD).
Treatment facilities catering to internet addiction offer a nurturing setting wherein afflicted individuals cultivate more constructive online behaviors while striving to attain a more harmonious and satisfying offline existence.
What are the types of impulse control disorder?
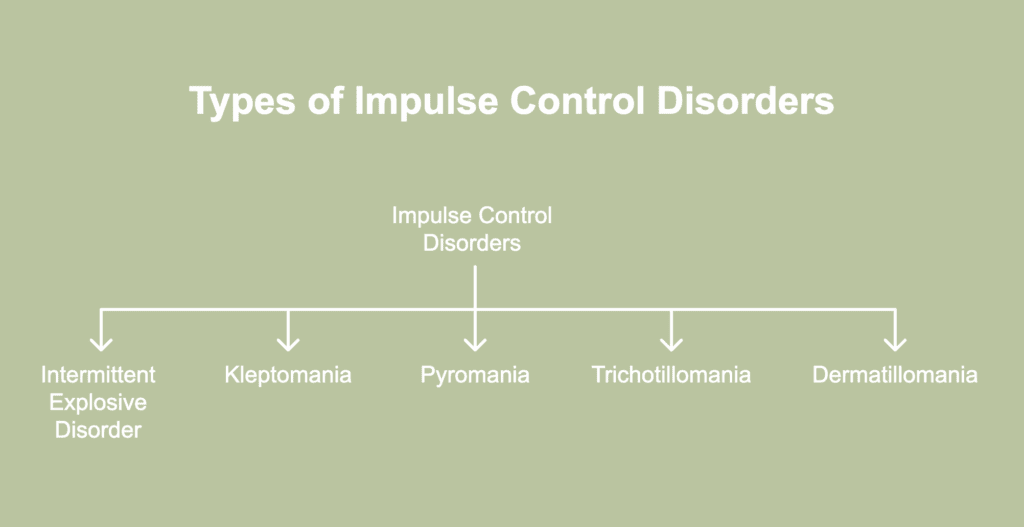
Impulse control disorders (ICDs) refer to a group of psychiatric disorders characterized by difficulty resisting urges or impulses possibly harmful to oneself or others. Types of impulse control disorder are distinct mental illnesses marked by difficulties resisting negative impulses or desires, usually leading to disruptive and repetitious behaviors. The types of impulse control disorder are listed below.
- Intermittent explosive disorder
- Kleptomania
- Pyromania
- Trichotillomania
- Dermatillomania
1. Intermittent explosive disorder
Intermittent explosive disorder (IED) is a psychiatric condition marked by repeated instances of impulsive aggression, such as sudden and excessive anger outbursts often not in proportion to the triggering factors or stressors at hand.
Individuals with IED experience intense feelings of anger, irritability, and rage, leading to explosive and uncontrolled expressions of aggression towards others or property.
The causes of intermittent explosive disorder include genetics, abnormalities in brain structure and function, exposure to adverse childhood experiences, and growing up in families exhibiting explosive behavior.
Treatments for IED include psychotherapy and medications, such as antidepressants and mood stabilizers/antiepileptics. Fluoxetine, an antidepressant, and oxcarbazepine, an antiepileptic medication, have potential benefits for treating intermittent explosive disorder, as per a 2022 report by Tahir et al., titled “Pharmacotherapy of impulse control disorders: A systematic review.”
Behavioral health hospitals mainly aid the treatment of IED. People with mental health issues, emotional difficulties, or behavioral problems receive thorough care and therapy at specialist medical facilities.
2. Kleptomania
Kleptomania is a recurrent, irresistible urge to steal, not for financial gain or personal use. Individuals with kleptomania experience an uncontrollable desire to steal things they don’t need or want.
The disorder involves increased tension, anxiety, and excitement relieved through stealing—however, the repercussions of stealing often cause guilt, shame, and depression.
The causes of kleptomania are not fully understood, but several factors contribute to its development, including a family history of impulse control disorders or mood disorders, neurobiological abnormalities, co-occurring mental health problems, traumatic experiences, and childhood adversity.
Treatment options for kleptomania include psychotherapy and medications such as opioid antagonists, primarily naltrexone, as well as self-help groups.
In an 8-week double-blind, placebo-controlled 2009 trial by Grant et al., titled “A Double-Blind, Placebo-Controlled Study of the Opiate Antagonist, Naltrexone, in the Treatment of Kleptomania” involving 25 kleptomaniac participants, naltrexone was found to dramatically lower impulses to steal and the act of stealing when compared to a placebo.
Specialized establishments for kleptomania provide a helpful and understanding atmosphere for people to examine symptoms, learn coping strategies, and gain more control over urges.
3. Pyromania
Pyromania is an impulse control disorder involving an uncontrollable urge to start fires. The disorder is stimulated by desires to undertake harmful behaviors such as fire setting to relieve stress, anxiety, and tension, and at the same time, experience a rush of pleasure and intense high.
Pyromania adversely impacts an individual, causing legal consequences like imprisonment due to arson and fines, damaging relationships, reputation, and career, and putting the affected person and the people around them in danger due to fire injuries.
The causes of pyromania include genetics, brain chemical imbalance, co-occurring psychiatric disorders, and traumatic life events.
Treatment for pyromania involves cognitive behavioral therapy (CBT) and medications, such as selective serotonin reuptake inhibitors (SSRIs), atypical antipsychotics, or antiepileptic drugs.
Facilities providing treatment for pyromania are typically within specialized mental health centers or addiction treatment programs. Therapy services assist individuals in identifying and addressing factors triggering deliberate fire-setting activities.
4. Trichotillomania
Trichotillomania is a mental health disorder characterized by obsessive and repetitive hair pulling, leaving one with obvious bald patches or hair loss. A common coping strategy for stress, anxiety, or other emotional difficulties, hair-pulling disorder disrupts everyday functioning and self-esteem.
Individuals with trichotillomania experience an irresistible urge to pull out strands of hair, often feeling tension or anxiety beforehand and relief or gratification afterward.
Trichotillomania is often brought on by a variety of factors, such as boredom, isolation, traumatic life events, mental health disorders, and genetic predispositions.
Treatment options for hair pulling disorder include habit reversal training (HRT), support groups, and medicines, such as antidepressants, opioid antagonists, atypical neuroleptics, and glutamatergic agents.
Rehabilitation institutions catering to individuals with trichotillomania do exist, albeit not exclusively. Mental health professionals, addiction counselors, or programs targeting body-focused repetitive behaviors and associated mental health concerns provide additional support.
5. Dermatillomania
Dermatillomania, otherwise known as excoriation disorder or skin picking disorder, is a mental health condition characterized by repetitive and compulsive picking, scratching, or picking at one’s own skin, leading to skin damage, lesions, and potential scarring.
Individuals with dermatillomania experience an intense urge to pick at perceived imperfections or irregularities on the skin, often resulting in significant physical and psychological distress.
The causes of chronic skin picking include genetics, structural brain changes, stress, anxiety, or other mental health conditions, boredom, and feelings of guilt or shame.
Treatment options for pathological skin picking are cognitive behavioral therapy (CBT), habit reversal training (HRT), support groups, and medications, such as antidepressants and anticonvulsants.
Trichotillomania rehabilitation facilities exist, though most address a broader range of conditions rather than focusing solely on the specific issue. Still, such places provide trichotillomania patients individualized programs like therapy and support in a controlled environment.
How does addiction treatment change based on addiction type?
Addiction treatment changes based on addiction type by tailoring interventions to the specific substance or behavior and its effects on the brain and body. Substance addictions like alcohol or opioids often require medical detoxification and medication-assisted therapy, while behavioral addictions such as gambling rely primarily on cognitive-behavioral therapy (CBT).
The intensity of treatment differs as well; severe drug dependencies require inpatient care, whereas mild addictions are managed through outpatient programs or support groups. Co-occurring mental health disorders influence treatment approaches, highlighting the necessity of addressing both addiction and underlying conditions simultaneously.
As per a 2014 publication titled “Principles of Drug Addiction Treatment: A Research-Based Guide (Third Edition)” from the National Institute on Drug Abuse (NIDA), no treatment is universally suitable for all individuals.
Treatment differs based on the patient’s characteristics and the specific drug taken. Treatment settings, interventions, and services must be tailored to address the specific issues and needs of each person in order to facilitate successful reintegration into society, the workplace, and productive family life.
How to understand which addiction type you have?
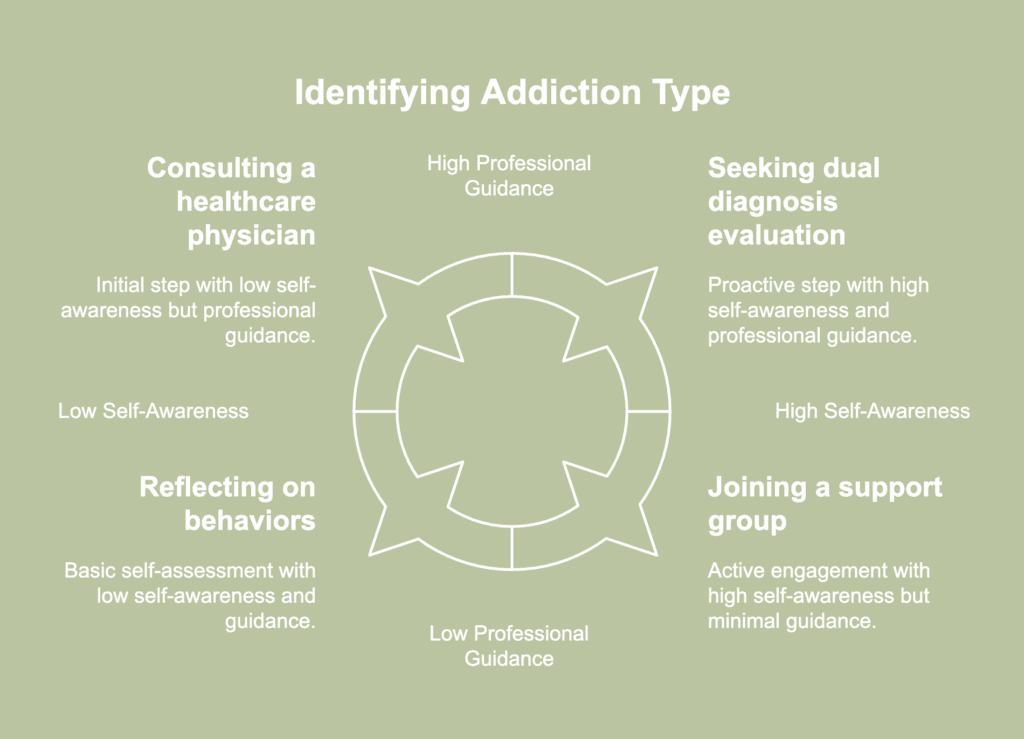
To understand which addiction type you have, it is necessary to focus on your behavior and the compulsions you exhibit. An instructional list to help you understand which addiction type you have is presented below.
- Self-assessment: Reflect on your behaviors and patterns related to the substance or behavior in question. Consider whether you experience cravings, withdrawal symptoms, or difficulty controlling your use.
- Identify patterns: Look for patterns in your behavior, such as increased tolerance, spending excessive time or money on the substance or behavior, or experiencing negative consequences in your personal or professional life.
- Research: Educate yourself about the different types of addiction, including physical addiction (substance dependence) and behavioral addiction (compulsive behaviors). Understand the specific criteria and symptoms associated with each type.
- Consult a professional: Consulting a healthcare physician or addiction specialist is wise as credentialed experts conduct thorough assessments, provide diagnosis, and recommend appropriate treatment courses.
- Observe effects: Pay attention to the effects of compulsive substance use or behavior on your physical health, mental well-being, relationships, and daily functioning. Consider whether the addiction primarily involves a substance or a specific behavior.
- Seek support: Reach out to support groups or online communities for individuals struggling with addiction. Talking about your own experiences and hearing about others’ struggles is a way to validate and offer insightful information.
- Keep a journal: Keep a journal to track feelings, thoughts, and actions related to addiction. Patterns, changes over time, and triggers become easier to identify through journaling.
- Consider dual diagnosis: If you suspect having underlying mental health issues contributing to your addiction, consider seeking a dual diagnosis evaluation. Various individuals with addiction have co-occurring mental health disorders, requiring integrated treatment.
- Be open to feedback: Be open to feedback from trusted friends, family members, or healthcare professionals. At times, others notice signs of addiction you are not able to recognize in yourself.
- Take action: After identifying the type of addiction, take proactive steps to address the issue. Actions include seeking professional treatment, joining a support group, altering your lifestyle, or developing strategies to manage cravings and triggers.
Do addiction symptoms change based on addiction type?
Addiction symptoms do change depending on the type of addiction an individual experiences. Physical addiction, often associated with substance dependence, typically involves symptoms such as increased tolerance to the substance, withdrawal symptoms when the substance is not used, and a compulsive need to use the substance despite negative consequences.
Symptoms manifest as cravings, physical discomfort, and psychological distress. On the other hand, behavioral addiction, characterized by compulsive behaviors, presents with symptoms such as preoccupation with the behavior, loss of control over the behavior, and continued engagement in the behavior despite adverse effects on one’s health, relationships, or daily functioning.
Consider the contrasting symptoms between someone struggling with alcohol addiction and another grappling with gambling addiction. Symptoms of alcohol addiction—a type of physical addiction—include physical dependence characterized by tolerance, withdrawal symptoms such as tremors or sweating when not drinking, and compulsive consumption despite negative consequences like liver damage or strained relationships.
Conversely, in gambling addiction, a type of behavioral addiction, symptoms involve preoccupation with gambling activities, loss of control over gambling behavior, and continued gambling despite mounting financial losses and legal troubles.
While both individuals exhibit signs of addiction such as craving, inability to stop substance use or specific behaviors, and negative consequences, the specific manifestations vary significantly due to the distinct nature of the addictive substances or behaviors involved.
Which addiction type is the most dangerous for financial well-being?
Gambling addiction is the addiction type widely regarded as the most dangerous for financial well-being. Financial well-being is the general state of one’s stability and health in terms of money, including income, savings, debt management, financial security, and capacity to fulfill financial commitments.
Gambling addiction, otherwise known as ludomania, involves obsessive gambling behavior persisting despite adverse outcomes. One’s financial condition is disastrously affected by gambling; major losses, debt, bankruptcy, and financial disaster are common outcomes.
Addiction to gambling is frequently accompanied by risky financial behaviors, including chasing losses, borrowing money, taking out loans, or resorting to other similar practices to finance gambling activities. Such actions contribute to escalating debt, financial stress, and diminishing assets.
Which addiction type is the most dangerous for physical well-being?
Opioid addiction is the addiction type considered most dangerous for an individual’s physical well-being. Physical well-being refers to the overall state of a person’s physical health and vitality, encompassing factors such as fitness, nutrition, sleep quality, immune function, and absence of illness or injury.
The obsessive use of opioid medicines despite detrimental effects—like health hazards, legal issues, and poor social functioning—is known as opioid addiction.
Chronic opioid use results in a range of adverse health outcomes, including respiratory depression, overdose, infectious diseases (such as HIV or hepatitis from needle sharing), cardiovascular complications, gastrointestinal issues, hormonal imbalances, and neurological impairments.
Further endangering physical health and well-being is the higher risk of accidents, injuries, and early mortality linked to opiate addiction.
Which addiction type is the most dangerous for psychological well-being?
Cocaine addiction is the most dangerous type of addiction for an individual’s psychological well-being. Psychological well-being reflects an individual’s mental health and emotional resilience, encompassing contentment, self-esteem, happiness, stress management, and the ability to navigate life’s challenges.
Cocaine addiction is a persistent and recurring disorder distinguished by compulsive and problematic consumption of the drug, regardless of the adverse repercussions.
Mood disorders including anxiety, depression, restlessness, and irritability are common among cocaine addicts. Intense and persistent symptoms often interfere with the ability to experience satisfaction or enjoyment in daily life.
Psychosis, encompassing hallucinations, delusions, paranoia, and disordered thinking, occurs more frequently in people addicted to cocaine and significantly disrupts perception of reality and functional performance.
Which addiction type is the most dangerous for social well-being?
Alcohol addiction is the most dangerous type of addiction for social well-being, owing to its pervasive legal status, widespread social acceptance, and profound repercussions at both the individual and societal levels.
Social well-being incorporates elements like community involvement, social support, belongingness, and the nature of bonds with peers, family, and friends, therefore reflecting the state of a person’s social interactions, relationships, and connections.
Alcohol addiction, otherwise known as alcohol dependence or alcohol use disorder (AUD), is a chronic condition distinguished by compulsive and excessive alcohol consumption. People struggling with alcohol addiction frequently have strong cravings, eventually causing alcohol use to increase.
A strong link exists between alcohol addiction and social well-being because long-term alcohol misuse causes a variety of interpersonal and social issues. Drinking too much sours friendships, family ties, and love connections. Trust and closeness in relationships are undermined by the resulting disputes, conflicts, and communication failures.
Addiction to alcohol additionally results in legal problems, including DUI (driving under the influence) arrests, accusations of public intoxication, and legal challenges pertaining to alcohol-related events. Serious social consequences from legal issues include social marginalization, financial instability, and job loss.