Opioid addiction: definition, types, symptoms, signs, long-term effects, withdrawal, and treatment
Table of content
- What is opioid addiction?
- What are the types of opioid addiction?
- What are the symptoms of opioid addiction?
- What are the signs of opioid addiction?
- What are the opioid addiction withdrawal symptoms?
- What are the long-term effects of opioid addiction?
- What are the treatments for opioid addiction?
- What are the risk factors for opioid addiction?
- What are the causes of opioid addiction?

Opioid addiction is a chronic, relapsing disorder characterized by the obsessive use of opioid medicines despite negative effects. The condition often involves physical dependence, with the body adapting to the drug and withdrawal symptoms emerging when use is reduced or stopped.
The types of opioid addiction include heroin addiction, oxycodone addiction, hydrocodone addiction, morphine addiction, codeine addiction, fentanyl addiction, methadone addiction, buprenorphine addiction, hydromorphone addiction, oxymorphone addiction, and tramadol addiction.
The symptoms of opioid addiction are drowsiness, poor decision making, mood swings, irritability, depression, lowered motivation, anxiety attacks, and withdrawal symptoms.
Signs of addiction to opioids include shallow or slow breathing rate, physical agitation, abandoning responsibilities, confusion, constricted pupils, constipation, euphoria, tolerance, and continued use.
Long-term effects of opioid addiction manifest in physical, psychological, and socio-economic ways.
Symptoms of opioid addiction withdrawal are lacrimation or rhinorrhea, goosebumps, muscle pain, nausea/vomiting, insomnia, and extreme light sensitivity.
Treatment options for opioid addiction include medications (methadone, buprenorphine, naltrexone), cognitive behavioral therapy (CBT), counseling, support groups, and motivational interviewing (MI).
What is opioid addiction?
Opioid addiction refers to a chronic and progressive disorder marked by an overpowering drive to use opioid substances despite harmful consequences. Frequently misused opioids include illegal drugs such as heroin and fentanyl, along with prescription painkillers like morphine and oxycodone.
Individuals with opioid addiction often develop physical dependence; their bodies adjust to the drug’s presence, resulting in tolerance and withdrawal symptoms once usage decreases or stops.
How common is opioid addiction?
Opioid addiction is extremely common, affecting approximately 16 million people worldwide and 2.1 million in the United States, according to a publication by Dydyk et al., titled “Opioid Use Disorder” last updated in January 2024.
The article further noted opioid addiction remains a major factor in the ongoing epidemic across the US, severely reducing the quality of life for individuals suffering from the condition.
What is the other name for opioid addiction?
The other name for opioid addiction is opioid use disorder (OUD). The term is used in diagnostic manuals like the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) to provide a more accurate and less stigmatizing description.
Health professionals prefer the term opioid use disorder for conveying a medical perspective and a neutral tone. Referring to the condition as OUD encourages a more compassionate and medical approach to care and recovery.
What are the types of opioid addiction?
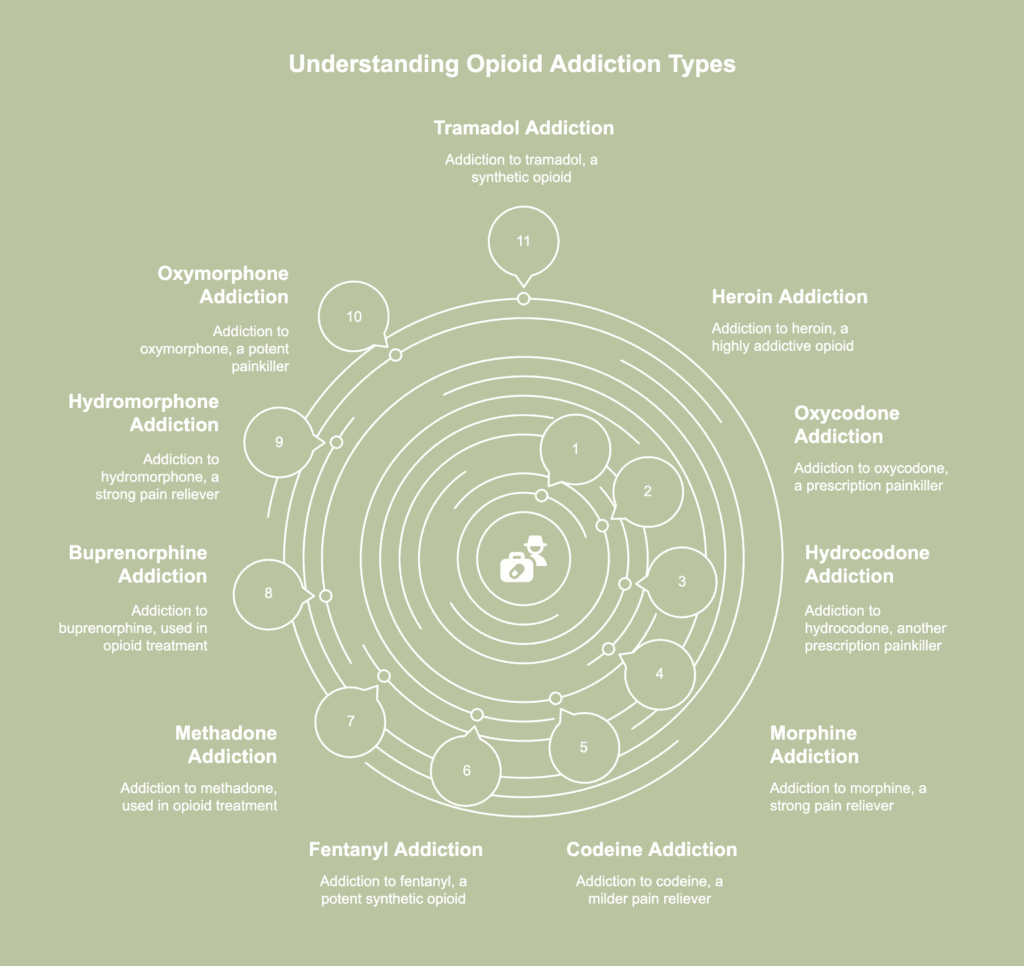
Types of opioid addiction encompass a wide range of categories and patterns of opioid misuse and dependency individuals encounter. The types of opioid addiction are listed below.
- Heroin addiction
- Oxycodone addiction
- Hydrocodone addiction
- Morphine addiction
- Codeine addiction
- Fentanyl addiction
- Methadone addiction
- Buprenorphine addiction
- Hydromorphone addiction
- Oxymorphone addiction
- Tramadol addiction
1. Heroin addiction
Heroin addiction is a long-term condition brought on by the regular consumption of the extremely addictive narcotic heroin. Intense cravings, a loss of control, and prolonged use despite the detrimental effects on health and daily life result from the condition.
Heroin addiction statistics revealed in 2022, 0.3% (or 900,000) of people aged 12 or older reported having a heroin use disorder in the previous year, according to a 2023 publication titled “Key Substance Use and Mental Health Indicators in the United States: Results from the 2022 National Survey on Drug Use and Health” from the Substance Abuse and Mental Health Services Administration (SAMHSA).
Adults 26 years of age or older had the largest percentage of individuals with a heroin use disorder in the past year (0.4 percent, or 864,000 persons).
2. Oxycodone addiction
Oxycodone addiction is characterized as a strong drive to take the semi-synthetic opioid beyond medical requirement, often resulting in compulsive behavior. Continued misuse damages relationships, impairs judgment, and triggers withdrawal symptoms when not taken.
According to statistics available for oxycodone addiction from the article titled, “Key Substance Use and Mental Health Indicators in the United States: Results from the 2022 National Survey on Drug Use and Health” published in November 2023 by the Substance Abuse and Mental Health Services Administration, in 2022, 2.5 million persons, or 30.7% of prescription painkiller abusers from the previous year, misused oxycodone medications, including generic oxycodone, Roxicodone, Percocet, Percodan, and OxyContin.
3. Hydrocodone addiction
Hydrocodone addiction develops from repeated misuse of the opioid medication, often taken in larger amounts or for longer periods than prescribed. Numerous adverse health consequences result from the condition.
When it comes to statistics on hydrocodone addiction, SAMHSA, in a 2023 publication titled “Key Substance Use and Mental Health Indicators in the United States: Results from the 2022 National Survey on Drug Use and Health” revealed of the 8.5 million individuals in 2022 aged 12 or older and had abused prescription painkillers in the previous year, 45.1%, or 3.7 million, had abused hydrocodone products.
4. Morphine addiction
Morphine addiction is a long-term, relapsing disease marked by the obsessive use of morphine, a potent opioid painkiller frequently given for severe pain treatment. Tolerance, withdrawal symptoms, and major disruptions to regular activities and health are typically the outcomes of prolonged abuse.
Figures on morphine addiction in the 22nd chapter of the book Global Emergency of Mental Disorders titled “The opioid epidemic” by Moini et al., stated in a recent National Institute on Drug Abuse research, 89% of men and women with opioid dependence tested positive for morphine.
5. Codeine addiction
Codeine addiction is the obsessive use of codeine, an opioid painkiller and cough suppressant present in numerous prescription drugs. Due to cravings and withdrawal symptoms, the disorder compromises judgment, everyday functioning, and general well-being.
Codeine addiction statistics show codeine product abuse accounted for 22.2%, or 1.9 million individuals, of the prescription pain reliever abuse in the previous year among individuals aged 12 and up, as per a 2023 publication titled “Key Substance Use and Mental Health Indicators in the United States: Results from the 2022 National Survey on Drug Use and Health” from (SAMHSA).
6. Fentanyl addiction
Fentanyl addiction is a serious, frequently fatal substance dependence brought on by the misuse of fentanyl, a synthetic opioid with a far higher potency than heroin or morphine.
Statistics involving fentanyl addiction confirmed in 2022, 991,000 individuals aged 12 or older (or 0.4 percent) misused prescription fentanyl or used illegally manufactured fentanyl (IMF) in the previous year, according to an article titled “Key Substance Use and Mental Health Indicators in the United States: Results from the 2022 National Survey on Drug Use and Health” published in November 2023 by SAMHSA.
7. Methadone addiction
Methadone addiction is a condition marked by over-reliance on methadone, a long-acting opioid commonly prescribed for pain relief or included in opioid replacement programs for individuals addicted to heroin or similar substances.
According to methadone addiction statistics provided by the United States Department of Justice’s 2003 publication titled “Methadone Fast Facts,” the Treatment Episode Data Set indicated a significant rise in the number of patients treated for “other opiates” misuse, including methadone, from 28,235 in 2000 to 36,265 in 2001.
8. Buprenorphine addiction
Buprenorphine addiction is a condition defined by the chronic and obsessive consumption of buprenorphine, a partial opioid agonist commonly used to treat pain and opioid use disorders.
Buprenorphine is frequently combined with naloxone and sold under the brand name Suboxone, a medication formulated to reduce misuse. However, certain individuals misuse Suboxone by dissolving or injecting the drug, leading to what is commonly referred to as Suboxone addiction.
According to a 2021 study by Han et al., titled “Trends in and Characteristics of Buprenorphine Misuse Among Adults in the US,” statistics on buprenorphine addiction revealed in 2019, approximately 2.4 million adults in the United States used buprenorphine, and 0.7 million (29.2%) misused the drug.
9. Hydromorphone addiction
Hydromorphone addiction is characterized by an individual’s dependence on hydromorphone, a potent opioid analgesic employed to alleviate severe pain. Although effective for short-term relief, prolonged or improper use leads to physical dependence and psychological cravings.
Hydromorphone addiction data show in 2022, 8.5 million individuals aged 12 or older misused prescription pain relievers within the past year. Among them, 102,000 people, or 1.2%, reported abusing hydromorphone products, based on SAMHSA’s 2023 report titled “Key Substance Use and Mental Health Indicators in the United States: Results from the 2022 National Survey on Drug Use and Health.”
10. Oxymorphone addiction
Oxymorphone addiction is a serious medical condition characterized by the misuse of oxymorphone, a potent opioid painkiller prescription for the treatment of severe pain. Continued use often results in escalating tolerance, withdrawal symptoms, and an increased risk of overdose.
According to information concerning oxymorphone addiction from the article “Key Substance Use and Mental Health Indicators in the United States: Results from the 2022 National Survey on Drug Use and Health” published in November 2023 by SAMHSA, during the year 2022, a total of 8.5 million individuals aged 12 or older engaged in the misuse of prescription pain medicines. Out of the total number, 1.4% (equivalent to 119,000 persons) were misusing oxymorphone products.
11. Tramadol addiction
Tramadol addiction is characterized by an individual’s dependence on tramadol, a synthetic opioid frequently prescribed for the alleviation of moderate to severe pain. Although considered less potent than drugs like oxycodone or morphine, tramadol still carries a significant risk for physical dependence and psychological addiction.
Statistics relating to tramadol addiction reveal an estimated 1.6 to 1.8 million Americans reporting any misuse of oral tramadol in the past year, either alone or in combination, from 2015 to 2017, according to a study titled “Misuse of Tramadol in the United States: An Analysis of the National Survey of Drug Use and Health 2002-2017” by Reines et al., published in June 2020.
What are the symptoms of opioid addiction?

Symptoms of opioid addiction encompass several indications someone is experiencing an opioid dependence. The symptoms of opioid addiction are listed below.
- Drowsiness: One of the most common signs of opioid use is excessive drowsiness. Sedation occurs because opioids depress the central nervous system, making the individual appear extremely sleepy or lethargic.
- Poor decision making: As a result of impaired judgment, people addicted to opioids often engage in risky behavior, such as driving under the influence, breaking the law to get narcotics, or neglecting personal responsibilities. A 2016 review by Biernacki et al., titled “Decision-making ability in current and past users of opiates: A meta-analysis” evaluated heroin users’ cognitive performance; chronic users showed consistently weaker results across various tasks, with impairments continuing even after 1.5 years of abstinence.
- Mood swings: Opioid addiction causes drastic fluctuations in mood, ranging from extreme euphoria during drug use to deep sadness or irritability during periods without the substance. The effects of the substance on brain chemistry—especially the areas in charge of reward and pleasure—cause mood instability.
- Irritability: As substance dependence deepens, individuals often display heightened agitation, particularly when access to the drug is limited. Such emotional responses frequently arise from withdrawal discomfort or the ongoing pressure of sustaining addictive behavior.
- Depression: Opioids artificially elevate feelings of pleasure, but long-term use reduces the brain’s ability to produce such sensations naturally. As a result, emotional lows become more pronounced when the drug is not present. A 2022 paper titled “Mood and Anxiety Symptoms in Persons Taking Prescription Opioids: A Systematic Review with Meta-Analyses of Longitudinal Studies” by Leung et al., revealed the use of prescription opioids, especially when frequent, high-dose, or protracted, correlates with heightened risks of mood and anxiety disorders, with more substantial evidence supporting a link to depression and anxiety than to bipolar disorder or post-traumatic stress disorder (PTSD).
- Lowered motivation: Opioid addiction frequently results in a noticeable decline in motivation to engage in everyday activities. The individual’s focus shifts almost entirely to obtaining and using the drug, neglecting personal and professional responsibilities.
- Anxiety attacks: Anxiety attacks are common among people suffering from opioid addiction. A 2021 report by Clark et al., titled “A Narrative Literature Review of the Epidemiology, Etiology, and Treatment of Co-occurring Panic Disorder and Opioid Use Disorder” established a substantial bidirectional association between panic disorder (PD) and OUD, influenced by common behavioral (precipitation, self-medication, shared vulnerability) and biological (periaqueductal gray serotonin-opioid interactions) mechanisms.
- Withdrawal symptoms: When someone dependent on opioids stops or greatly reduces usage, withdrawal symptoms typically occur. The body reacts physically to the absence of the substance, often producing intense discomfort and pushing continued drug use as a means of relief.
What are the signs of opioid addiction?
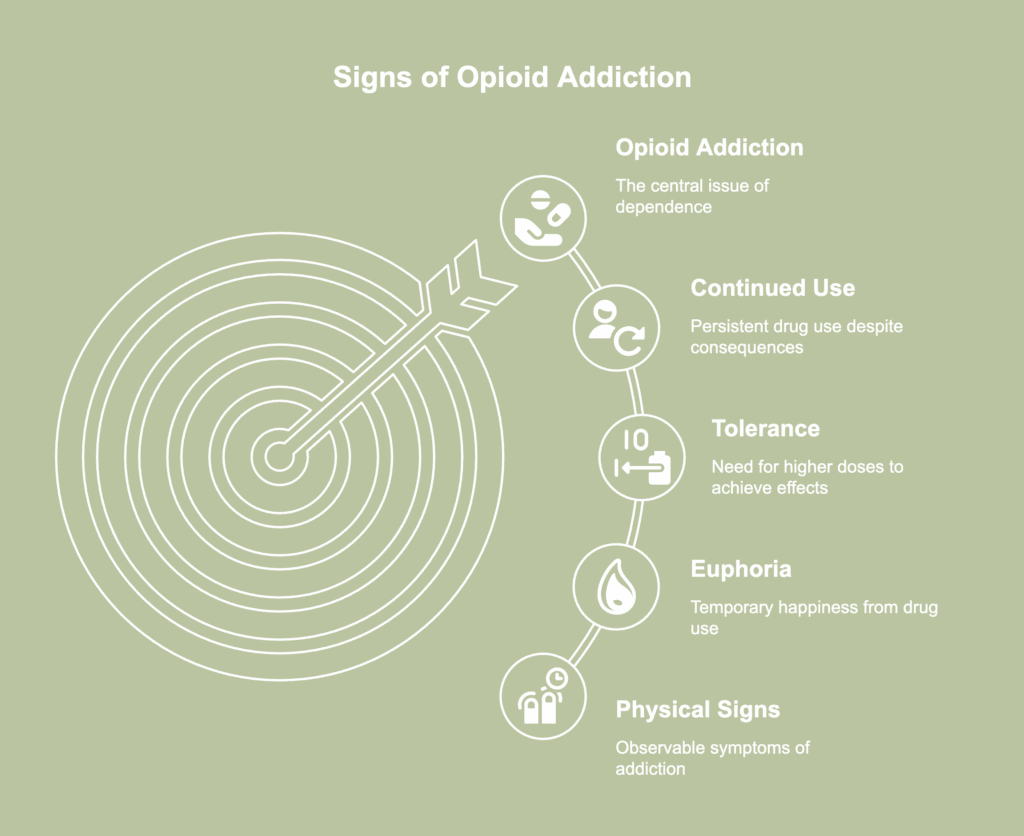
Signs of opioid addiction are apparent indicators showing an individual is experiencing dependence on opiates. The signs of opioid addiction are listed below.
- Shallow or slow breathing rate: Opioid use depresses the respiratory system, leading to a noticeably slow or shallow breathing rate. As use continues or dosage increases, breathing becomes noticeably weaker or slower, even during periods of rest. Regular opioid use dulls the body’s natural response to rising carbon dioxide levels, preventing the usual urge to breathe deeply.
- Physical agitation: While opioids typically cause drowsiness, withdrawal or lack of access to the drug leads to physical agitation. The behavior is often a response to the body’s craving for the drug and the discomfort of withdrawal symptoms.
- Abandoning responsibilities: Individuals addicted to opioids often neglect responsibilities at work, school, or home, leading to poor performance, absenteeism, and a general decline in productivity. Personal relationships additionally suffer as the individual becomes increasingly preoccupied with obtaining and using the drug.
- Confusion: Opioid addiction often leads to cognitive impairments, resulting in confusion and disorientation. According to a 2021 research article by Moghaddam et al., titled “Cognitive Impairment in Opium Use Disorder,” with significant effect sizes suggesting clinically relevant deficiencies, working memory, information-processing speed, and verbal memory were the most affected cognitive domains in OUD.
- Constricted pupils: Unlike other causes of small pupils, opioid-induced constriction tends to remain consistent and is often one of the first visual signs of misuse. The change stems from the drug’s impact on the parasympathetic nervous system, a part of the body responsible for controlling involuntary functions. Law enforcement and healthcare providers frequently check pupil size to assess recent opioid use or overdose.
- Constipation: Opioid drugs impede gastric emptying and peristalsis in the gastrointestinal tract, resulting in delayed medication absorption and enhanced fluid absorption, as stated in the article “Opioid-Induced Constipation” by Sizar et al., last updated in August 2023. Insufficient fluid levels in the intestine lead to the hardening of feces and the development of constipation.
- Euphoria: A surge of intense happiness or well-being emerges when opioids elevate dopamine levels in the brain. Although the sensation fades quickly, the pleasurable effect creates a strong desire to continue using the drug to relive the experience.
- Tolerance: One of the main manifestations of opioid addiction is tolerance, a consequence of the body’s adjustment to prolonged drug use. Over time, the same amount of opioids produces a weaker effect, prompting the need for higher doses to achieve the desired relief or euphoria. The danger of negative side effects and overdosing rises with dosage.
- Continued use: People keep using the drug even when health, relationships, or obligations suffer. Changes in brain chemistry known to impair judgment and increase the desire to use drugs are frequently the cause of the behavior. The opioid-dependent reward system reinforces recurrent use patterns. Attempts to stop typically result in cravings or withdrawal symptoms, pushing the person to return to the substance.
What are the opioid addiction withdrawal symptoms?
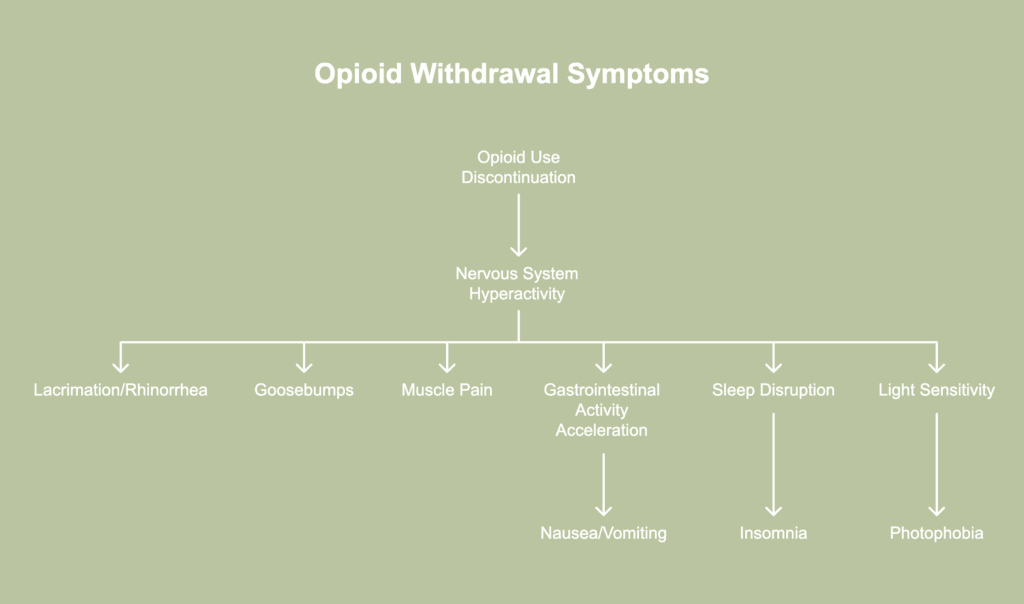
Opioid addiction withdrawal symptoms describe the variety of effects arising when someone dependent on opioids reduces or discontinues use of the substance. The opioid addiction withdrawal symptoms are listed below.
- Lacrimation or rhinorrhea: Lacrimation (excessive tearing) and rhinorrhea (runny nose) are common signs of opioid withdrawal due to the sudden disruption of the body’s regulation of fluids. When opioid use stops, the nervous system becomes hyperactive, leading to an overproduction of tears and nasal secretions. Such reactions often mimic the signs of a cold or allergies, though no infection is present.
- Goosebumps: Goosebumps, medically known as piloerection, commonly appear during withdrawal due to heightened nervous system activity. When opioids are no longer present, the body loses the calming effect the drug once provided, leading to overstimulation of nerve signals. The response activates tiny muscles at the base of hair follicles, causing the skin to form bumps and the hair to stand on end.
- Muscle pain: Once opioid use stops, the nervous system becomes overactive and sensitive, amplifying pain perception throughout the body. Muscles and joints begin to feel sore, tight, or even cramp without any physical exertion or injury. A 2020 review by Pergolizzi Jr. et al., titled “Opioid withdrawal symptoms, a consequence of chronic opioid use and opioid use disorder: Current understanding and approaches to management” stated the release of an excessive amount of norepinephrine (NE) during opioid discontinuation is the cause of numerous acute physical signs and symptoms of opioid withdrawal, including muscle cramps.
- Nausea/vomiting: Opioids slow digestion and dull nerve responses in the gut, so once the substance is removed, the body rebounds by accelerating gastrointestinal activity. The sudden shift overwhelms the digestive tract, triggering queasiness and an urge to vomit. The brain’s vomiting center, affected by opioid use, becomes highly sensitive during withdrawal. As a result, even minor stimuli like movement, smells, or stress provoke nausea.
- Insomnia: The absence of an addictive substance removes the false sense of calm once relied upon for sleep. According to a 2020 mini review by Eacret et al., titled “Bidirectional Relationship between Opioids and Disrupted Sleep: Putative Mechanisms,” deep non-rapid eye movement (NREM), rapid eye movement (REM), and general sleep quality are all negatively impacted by acute and chronic opioid use and withdrawal. Conversely, poor sleep exacerbates opioid usage by increasing pain sensitivity, negative feelings, and relapse risk.
- Extreme light sensitivity: During drug withdrawal, individuals experience extreme sensitivity to light, otherwise known as photophobia. Upon cessation of opioid use, the sudden absence of the drug causes a rebound effect. The nervous system becomes hyperactive and overly sensitive to stimuli, including light.
What are the long-term effects of opioid addiction?
Long-term effects of opioid addiction refer to the consequences resulting from prolonged opioid abuse. The long-term effects of opioid addiction are listed below.
- Physical
- Psychological
- Socio-economic
1. Physical long-term effects of opioid addiction
The physical long-term effects of opioid addiction include gastrointestinal problems, respiratory issues, cardiovascular system complications, increased risk of falls and fractures, reproductive health-related problems, and a heightened risk for HIV and other infectious diseases.
Harmful outcomes affecting multiple organ systems and overall health often reach severe levels. Physical addiction to opioid worsens existing medical conditions and blocks recovery by promoting repeated substance use. Continuous disruption interferes with natural healing processes and places sustained stress on the body.
2. Psychological long-term effects of opioid addiction
The psychological long-term effects of opioid addiction include persistent depression, anxiety disorders, and cognitive impairments, such as memory loss, impaired decision-making, and difficulty concentrating.
Chronic opioid use leads to persistent depression, as the brain’s ability to regulate mood becomes impaired. Anxiety disorders are likewise prevalent, characterized by elevated levels of panic and stress.
Cognitive impairments, such as memory loss and difficulty concentrating, arise from the neurotoxic effects of prolonged opioid use. Such mental and emotional disturbances reflect psychological addiction, driven not just by physical need but by entrenched mental reliance.
3. Socio-economic long-term effects of opioid addiction
The socio-economic long-term effects of opioid addiction include job loss, financial instability, strained relationships, legal troubles, reduced productivity, and increased healthcare costs.
Ongoing drug use interferes with workplace performance, often leading to absenteeism or termination. Unemployment and reduced income contribute to mounting debt and an inability to meet basic needs.
Family and social connections weaken as trust erodes and conflicts increase. Drug-related offenses give rise to legal problems, leading to fines, arrests, or imprisonment.
Addiction reduces productivity on both an individual and community level. Both public and private healthcare systems bear a significant financial burden as a result of long-term health issues associated with opiate usage.
What are the complications and dangers of opioid addiction?
The complications and dangers of opioid addiction include death, persistent constipation, infections, mental health disorders, overdose, respiratory depression, and organ damage. Chronic constipation arises from opioids slowing gastrointestinal function, often leading to discomfort, bloating, or bowel obstruction.
Unsafe usage methods or contaminated needles result in illnesses such as heart valve infections, hepatitis, or human immunodeficiency virus (HIV). Addiction frequently coexists with psychiatric conditions, including depression and anxiety.
OUD frequently results in drug overdose, a state known to be fatal if not treated promptly. According to a 2023 publication titled “Opioid overdose” from the World Health Organization, in 2019, substance use caused around 600,000 deaths globally. Opioids contributed to nearly 80% of all fatalities, with overdose accounting for roughly 25% of the total death toll.
Opioids suppress the respiratory system, creating a risk of dangerously slow or stopped breathing. Long-term use leads to chronic health decline by harming important organs like the kidneys, liver, and heart. Advanced stages of addiction sometimes lead to fatal outcomes, especially when combined with potent substances like fentanyl.
What are the treatments for opioid addiction?

Treatments for opioid addiction refer to a variety of interventions intended to assist individuals in overcoming opioid dependence. The treatments for opioid addiction are listed below.
- Medications (methadone, buprenorphine, and naltrexone): Medications play a vital role in treating opioid use disorder by helping stabilize brain chemistry and reduce drug cravings. Methadone, a synthetic opioid agonist, works similarly to other opioids by targeting brain opioid receptors to ease cravings and withdrawal symptoms, according to an article titled “Medications for Opioid Use Disorder” published in March 2025 by the National Institute on Drug Abuse (NIDA). Buprenorphine, a partial opioid agonist, helps relieve cravings and manage withdrawal. Naltrexone, an opioid antagonist, blocks opioid effects and stops any euphoric sensations from occurring, making it useful for relapse prevention.
- Cognitive behavioral therapy (CBT): Individuals dealing with OUD often benefit from CBT, a structured form of psychotherapy. Effective problem-solving skills, methods for managing stress, and the ability to recognize one’s own triggers are all part of the approach. The sessions center around developing more constructive ways of thinking and responding to challenging situations. CBT gradually promotes enhanced coping mechanisms and increased emotional resilience.
- Counseling: Counseling plays a vital role in treatment and generally works alongside all prescribed medications, based on a 2016 publication titled “Opioid Addiction Treatment: A Guide for Patients, Families and Friends” from the American Society of Addiction Medicine. Sessions additionally help individuals work through personal, social, or external challenges possibly linked to substance dependence.
- Support groups: Support groups provide mutual encouragement and connection through a community made up of individuals with shared experiences of opioid addiction. Attending support group meetings on a consistent basis fosters accountability, reduces feelings of isolation, and enhances social support.
- Motivational interviewing (MI): An effective, low-cost intervention for unmotivated OUD patients, MI enhances treatment retention and abstinence rates in brief sessions, according to a 2024 paper by Durpoix et al., titled “Psychotherapies in opioid use disorder: toward a step-care model.” Motivational interviewing encourages people to investigate personal reasons for change in a non judging environment, therefore helping with opioid addiction.
Which opioid addiction treatment is the most effective?
The most effective treatment for opioid addiction is frequently the combination of medication, counseling, and other forms of support, as stated in a report titled “Opioid Addiction Treatment: A Guide for Patients, Families and Friends” published in 2016 by the American Society of Addiction Medicine.
Incorporating multiple elements allows for a more tailored approach to each patient, addressing both psychological and physical factors involved in addiction while significantly improving the chances of lasting recovery.
What is the success rate for opioid addiction treatment?
The success rate for opioid addiction treatment is highlighted in a 2020 study titled “Trends in abstinence and retention associated with implementing a Medication Assisted Treatment program for people with opioid use disorders using a Collective Impact approach” by Brunisholz et al., reporting 84% opioid abstinence and 58% retention at 365 days through a community-based MAT program in Utah.
The program used a collective impact approach and recorded 75% abstinence and 94% retention at 90 days. Results reflect the effectiveness of combining medication with coordinated community efforts. Sustained participation and high abstinence rates demonstrate the potential of structured, community-driven treatment models.
Another study by Roger D. Weiss and Vinod Rao titled, “The Prescription Opioid Addiction Treatment Study: What have we learned” published in April 2017 revealed a 12-week stabilization period using buprenorphine-naloxone (bup-nx) led to abstinence or near-abstinence in 49% of participants, demonstrating the effectiveness of maintenance therapy.
A short 4-week bup-nx taper resulted in a 7% success rate, which remained low at 8–9% after eight weeks. The outcome highlights the difficulty of discontinuing medication without sustained support. Long-term treatment proves more reliable for managing opioid use disorder.
Can you overcome opioid addiction without professional help?
No, you cannot overcome opioid addiction without professional help due to the complex physical and psychological nature of the condition. Withdrawal symptoms such as nausea, anxiety, insomnia, and intense cravings make self-detox extremely difficult and potentially dangerous.
Professional treatment offers medical supervision to ease withdrawal and reduce health risks. Structured programs offer behavioral techniques aiming at emotional triggers and compulsive thinking habits.
Without guidance, relapse becomes more likely as individuals struggle to manage cravings and stressors alone. A thorough, well managed approach is usually necessary for long-term recovery from opioid addiction.
What are the issues with opioid addiction treatment?
The issues with opioid addiction treatment include social and internalized stigma related to using medications for opioid use disorder (OUD), logistical issues, treatment experiences, and knowledge gaps, a 2020 paper by Mackey et al., titled “Barriers and Facilitators to the Use of Medications for Opioid Use Disorder: a Rapid Review” revealed.
The study explained patients often faced both internalized and social stigma linked to the use of OUD medications. Medication was viewed as a “crutch” and believed to fall short of representing true sobriety. Past negative encounters with OUD treatment, including mistreatment or insufficient support from staff, presented major barriers as well.
Barriers related to logistics, such as costly charges, trouble locating providers, transportation problems, and prerequisites to first fail abstinence-based treatments, were identified. Finally, a lot of people had no idea what to anticipate from drugs like naltrexone and had little information about available treatments.
What are the risk factors for opioid addiction?
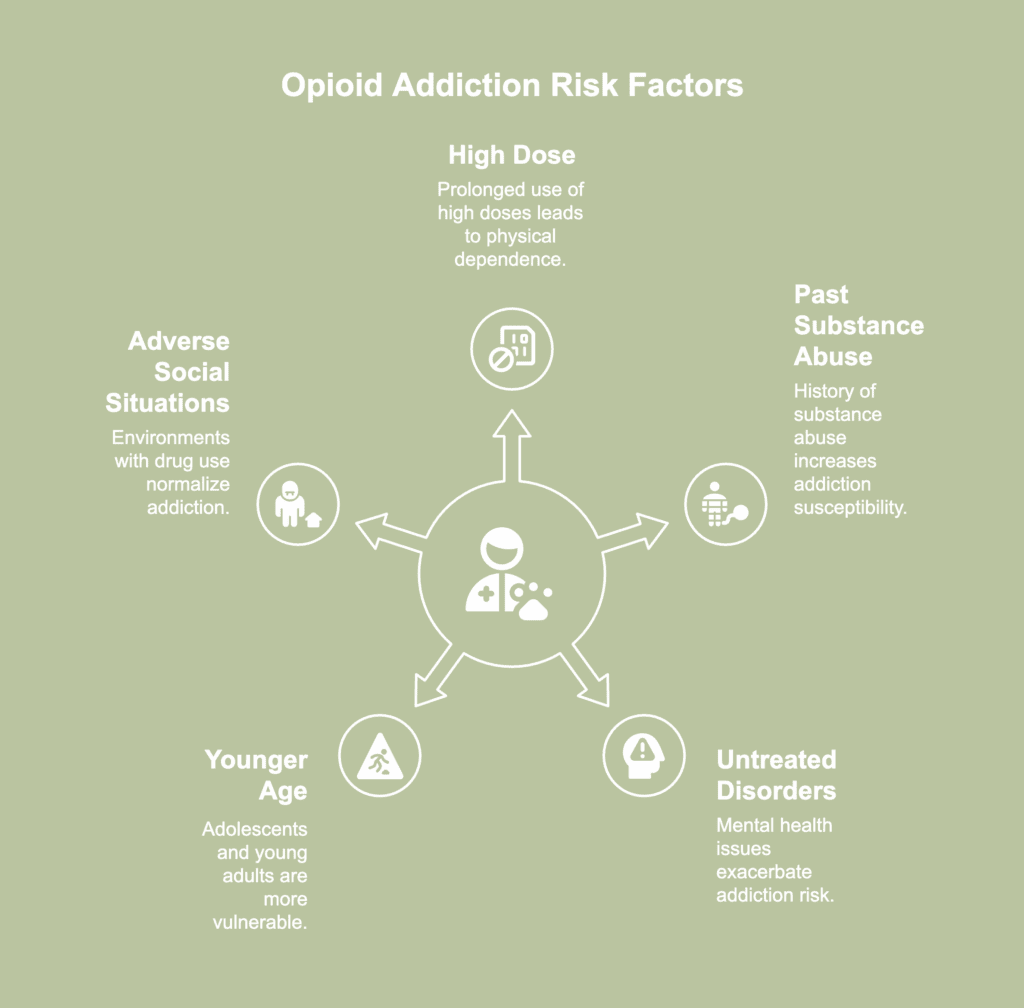
Risk factors for opioid addiction describe a person’s predisposition toward opioid dependence as a result of certain conditions, behaviors, or traits. The risk factors for opioid addiction are listed below.
- High dose: Taking high doses of opioids, especially over a prolonged period, significantly increases the risk of addiction. Higher doses lead to greater physical dependence as the body becomes accustomed to the drug’s effects.
- Past or current substance abuse: Individuals with a history of substance dependence, including alcohol or other drugs, are more likely to develop an addiction to opioids. Prior substance abuse alters brain chemistry and increases susceptibility to addiction.
- Untreated psychiatric disorders: Mental health disorders increase the risk of opioid addiction, especially if left untreated. A 2019 paper by Cragg et al., titled “Risk Factors for Misuse of Prescribed Opioids: A Systematic Review and Meta-Analysis” reported individuals with mental health disorders were twice as likely to misuse prescribed narcotics. Individuals tend to misuse medications to ease withdrawal symptoms, produce psychological effects, or substitute for other substances.
- Younger age: Young adults and adolescents face a higher risk of developing opioid addiction. According to a 2019 study by Cragg et al., titled “Risk Factors for Misuse of Prescribed Opioids: A Systematic Review and Meta-Analysis,” prescription medications often end up misused by younger individuals due to easy availability from friends or family. However, study findings indicated greater misuse among youth even when access to prescribed opioids remained equal across age groups. Higher likelihood of abuse among younger populations persisted regardless of source.
- Adverse social or familial situations promoting abuse: Growing up or living in environments with prevalent or accepted drug use increases the risk of opioid addiction. Social influences—such as peer pressure and normalized attitudes toward drug use—foster experimentation and regular opioid use.
Is there a connection between opioid addiction and ADHD?
Yes, there is a connection between opioid addiction and ADHD, as rates reported by Beslot et al., in a 2024 study titled “ADHD: prevalence and effect on opioid use disorder treatment outcome in a French sample of patients receiving medication for opioid use disorder—the influence of impulsivity as a mediating factor” showed 46% of OUD patients had probable childhood ADHD—significantly higher than in the general population (4–5%).
ADHD is linked to earlier opioid use onset, reduced educational attainment, and elevated impulsivity, including negative urgency, lack of premeditation, and sensation seeking. Negative urgency alone explained 44% of the association between childhood ADHD and treatment failure, emphasizing its contribution to relapse risk. Such traits complicate recovery and hinder treatment progress.
What are the causes of opioid addiction?
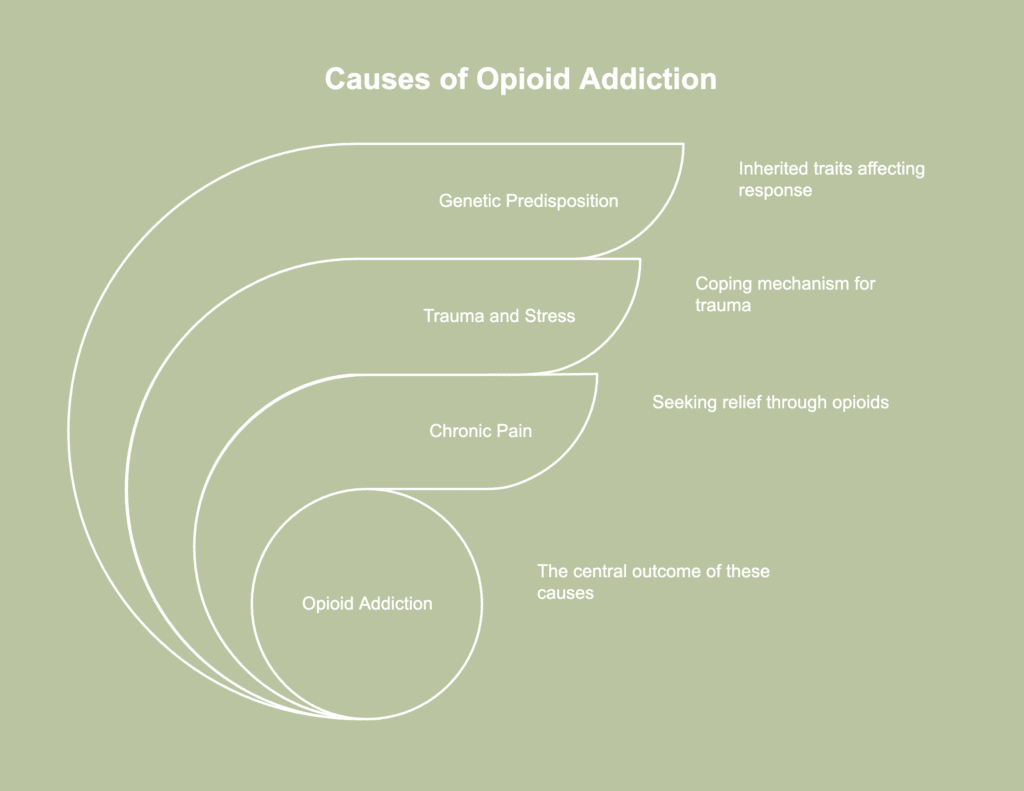
Causes of opioid addiction denote the diverse elements interacting intricately, leading to the emergence of opioid dependence. The causes of opioid addiction are listed below.
- Genetic predisposition: Genetic predisposition contributes to opioid addiction by influencing how the brain responds to opioids. Individuals with a family history of substance use disorders often possess inherited traits enhancing reward sensitivity or limiting impulse control. Variations in specific genes affect opioid receptor activity, making certain people more susceptible to dependence. Inherited vulnerability increases the likelihood of addiction when opioids are introduced.
- Trauma and stress: Experiencing significant trauma, whether from physical, emotional, or sexual abuse, leads individuals to misuse opioids as a coping mechanism. According to a 2024 report by Rodríguez et al., titled “Trauma exposure across the lifespan among individuals engaged in treatment with medication for opioid use disorder: differences by gender, PTSD status, and chronic pain,” significant trauma burden is present among patients undergoing medication treatment for opioid use disorder (MOUD), with 99.7% indicating the experience of at least one traumatic event, and notable prevalence in interpersonal (e.g., 79% intimate partner violence), non-interpersonal (86% accidents), and childhood (81% total) categories.
- Chronic pain: Individuals enduring ongoing pain often seek relief through opioids, a pattern likely to result in dependency. As time passes, the body builds tolerance, requiring higher dosages to achieve the same effect, raising the likelihood of addiction. People with chronic pain face heightened vulnerability when alternative methods for pain control remain unaddressed.
How long does it take to develop an opioid addiction?
The time it takes to develop an opioid addiction is highly conditional on a number of variables, such as one’s genetic composition, the amount and frequency of opioid usage, and any preexisting mental health issues.
It is important to note, however, that tolerance develops unexpectedly quickly, even in instances of intense pain; clinical indications of tolerance manifest within a couple of weeks, according to a 2013 article titled “Long-Term Opioid Treatment” by Craig T. Hartrick.
While tolerance is a component of addiction and is often an early step toward it, addiction itself is a broader and more severe condition involving behavioral and psychological aspects.