Hydrocodone addiction: signs, withdrawal symptoms, and treatment
Table of content
- What is hydrocodone addiction?
- What are the signs of hydrocodone addiction?
- What are the withdrawal symptoms of hydrocodone?
- What are the treatments for hydrocodone addiction?
- Why is using hydrocodone addictive?
- What are the causes of hydrocodone addiction?
- What are the side effects of hydrocodone?
- What are the risk factors for hydrocodone addiction?

Hydrocodone addiction is a persistent condition marked by the irresistible use of hydrocodone notwithstanding detrimental outcomes. The psychological and physiological aspects of the condition cause cravings and withdrawal when the substance is not used.
The signs of hydrocodone addiction include compulsive drug-seeking behavior, tolerance, using the medication for longer duration or in higher quantities than planned, cravings, engaging in dangerous activities while under the influence, persisting in substance use despite health problems, and neglecting responsibilities.
The withdrawal symptoms of hydrocodone addiction are anxiety, sweating, nausea and vomiting, muscle aches, insomnia, chills, high blood pressure, and excessive yawning.
Treatments for hydrocodone addiction include detoxification, cognitive behavioral therapy (CBT), support groups and 12-step programs, inpatient rehabilitation, and outpatient rehabilitation.
What is hydrocodone addiction?
Hydrocodone addiction is a type of opioid use disorder (OUD) indicated by the compulsive use of the opioid prescription painkiller hydrocodone despite risks to one’s health, interpersonal connections, and day-to-day functioning.
Hydrocodone is effective in pain management but carries a high potential for abuse and dependence. Addiction (substance dependence) develops as users build tolerance, requiring higher doses to achieve the same effect, leading to physical dependence marked by withdrawal symptoms and psychological dependence characterized by intense cravings.
What are the brand names for hydrocodone?
The brand names for hydrocodone include Vicodin, Norco, Lortab, Hysingla ER, Dolorex Forte, Maxidone, Co-Gesic, and Hycodan. Multiple brand names of hydrocodone are available; most of these drugs enhance pain relief by combining hydrocodone with paracetamol.
Often prescribed to control moderate to severe pain, Vicodin is among the most identifiable brands. Norco, sharing a similar formulation with Vicodin, usually has a higher hydrocodone-to-acetaminophen ratio, delivering more potent relief for individuals needing stronger medication. Another common choice is Lortab, providing a similar combination of acetaminophen and hydrocodone.
How common is hydrocodone addiction?
Hydrocodone addiction is common; of the 8.5 million individuals aged 12 and older who abused prescription painkillers in 2022, 45.1% (or around 3.7 million) particularly abused hydrocodone products, according to a 2023 publication titled, “Key Substance Use and Mental Health Indicators in the United States: Results from the 2022 National Survey on Drug Use and Health” from the Substance Abuse and Mental Health Services Administration.
The publication further noted traditionally, hydrocodone medications have been the most often prescribed opioids, therefore boosting availability for usage. Following similar prescribing trends, hydrocodone products represented the most frequently abused prescription analgesics during 2022.
What are the signs of hydrocodone addiction?

Signs of hydrocodone addiction are any of the several clues pointing to a person’s addiction to the opioid painkiller. The signs of hydrocodone addiction are listed below.
- Compulsive drug-seeking behavior: Individuals with hydrocodone addiction often go to great lengths to obtain the drug, including visiting multiple doctors or pharmacies, known as “doctor shopping.” Some engage in unlawful actions like prescription forgery. The incessant need to get the substance ruins relationships and throws everyday responsibilities in a downward spiral.
- Tolerance: Tolerance develops when a person needs higher doses of hydrocodone to achieve the same pain-relieving effects. According to a continuing education activity last updated in October 2024 by Manuchehr Habibi and Peggy Y. Kim, titled “Hydrocodone and Acetaminophen,” the most frequent adverse effect of hydrocodone, like all opioids, is tolerance to higher dosages in order to preserve the same degree of pain management and physical dependence.
- Using the medication for longer duration or in higher quantities than planned: Affected individuals use hydrocodone for more extended periods or in higher doses than initially prescribed or planned. The behavior often stems from developing tolerance and a subsequent need for greater quantities to achieve the same effects. Such usage increases the risk of severe side effects, dependence, and overdose.
- Cravings: People addicted to hydrocodone often face powerful cravings, making concentration on other tasks nearly impossible. Usually persistent and strong, cravings cause one to think constantly about getting and using the drug. A key psychological aspect of addiction, cravings signify a high degree of dependency.
- Engaging in dangerous activities while under the influence: Hydrocodone addicts engage in dangerous activities while under the influence, such as driving or operating heavy machinery. Such behavior endangers both the individual and those nearby. Impaired coordination and judgment from the drug frequently result in accidents and legal trouble.
- Persisting in substance use despite health problems: Despite experiencing physical health issues like chronic constipation or mental health problems such as anxiety or depression, individuals continue using hydrocodone. The ongoing use exacerbates medical conditions, creating a detrimental cycle of dependency and worsening health.
- Neglecting responsibilities: Addiction to hydrocodone often results in the abandonment of both personal and professional duties. Missed workdays, unfulfilled family commitments, and poor self-care frequently occur as drug use takes precedence over basic responsibilities. Behavioral patterns reflect a deep disruption of daily structure and priorities.
What are the withdrawal symptoms of hydrocodone?
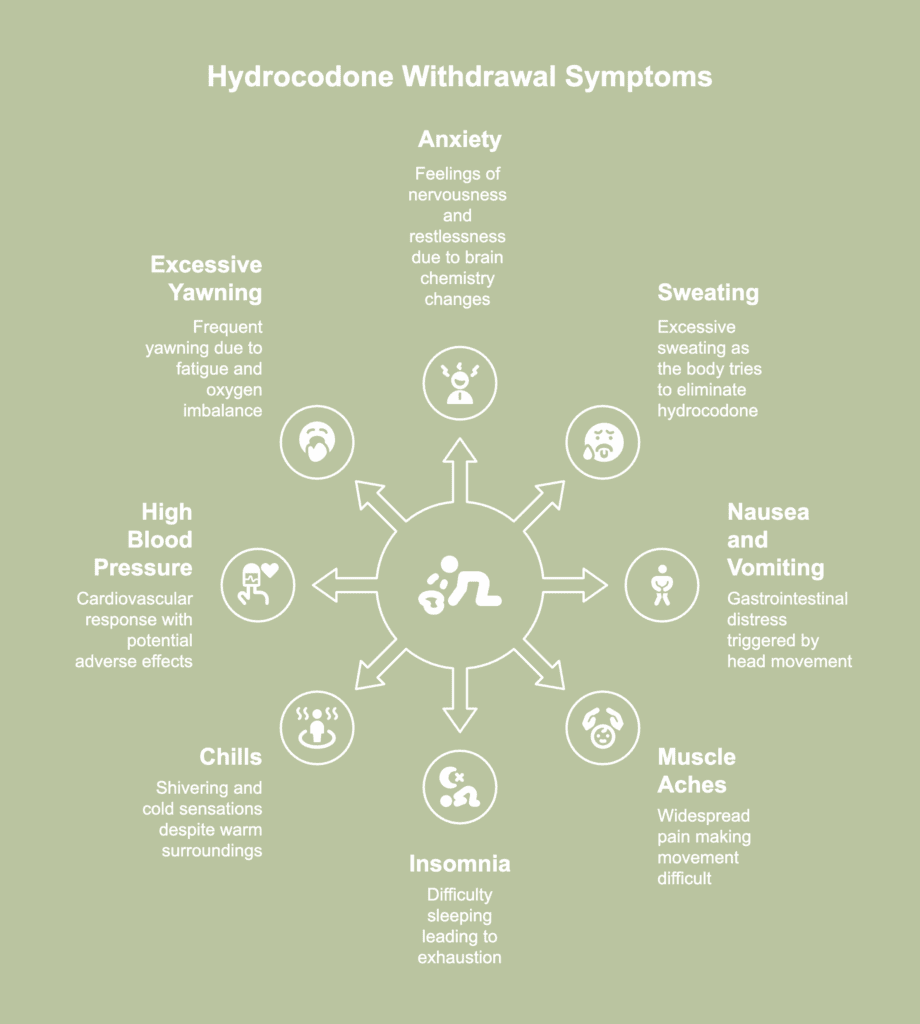
Withdrawal symptoms of hydrocodone refer to the effects emerging when a person suffering from dependence on the drug suddenly reduces or stops usage. The withdrawal symptoms of hydrocodone are listed below.
- Anxiety: Anxiety during withdrawal manifests as feelings of nervousness, restlessness, and worry. The symptom arises because the brain’s chemistry is adjusting to the absence of hydrocodone. Anxiety interferes with daily activities and exacerbates the stress of withdrawal.
- Sweating: Excessive sweating is a physical response to the body’s attempt to rid itself of hydrocodone. A 2017 case report by Hong et al., titled “Methadone-Induced Hyperhidrosis Treated With Oxybutynin” concerned a 35-year-old male undergoing methadone maintenance therapy who subsequently developed hyperhidrosis (excessive sweating) soon after commencing treatment. The report proposed a potential mechanism for opioid-induced sweating involving histamine release triggered by opioids such as methadone. A study cited by the paper supports the explanation, showing successful treatment of opioid-induced hyperhidrosis using an antihistamine (desloratadine, 5 mg/day).
- Nausea and vomiting: Nausea and vomiting are common gastrointestinal symptoms experienced during withdrawal. According to a 2017 article by Heuser et al., titled “Preventing opioid-induced nausea and vomiting: Rest your head and close your eyes?,” opioid-induced nausea and vomiting (OINV) is triggered by head movement since opioids disrupt the balance processes in the inner ear, therefore giving contradictory messages to the brain and causing nausea.
- Muscle aches: Muscle aches and pains result from the body’s readjustment to functioning without hydrocodone. Pains tend to be widespread and debilitating, making movement and daily tasks difficult.
- Insomnia: Insomnia, or difficulty sleeping, is a frequent withdrawal symptom leaving individuals feeling exhausted and irritable. As per a 2017 study by Serdarevic et al., with the title “The Association between Insomnia and Prescription Opioid Use: Results from a Community Sample in Northeast Florida,” the utilization of prescription opioids is markedly correlated with a 42–44% heightened probability of insomnia, irrespective of established risk factors such as depression, anxiety, and pain.
- Chills: Chills often occur alongside sweating as the body’s temperature regulation becomes disrupted during withdrawal. Individuals experience shivering and cold sensations even in warm environments. The symptom contributes to the overall physical discomfort of withdrawal.
- High blood pressure: High blood pressure, or hypertension, occurs as the body’s cardiovascular system responds to the absence of hydrocodone. A higher risk of cardiovascular problems, dizziness, and headaches are a few of the possible adverse effects.
- Excessive yawning: Excessive yawning frequently appears during hydrocodone withdrawal, likely caused by the body’s effort to balance oxygen levels while combating fatigue. Yawning tends to happen repeatedly throughout withdrawal, commonly linked to tiredness or low energy. Although relatively benign, excessive yawning is indicative of the body’s stress response to withdrawal.
What are the treatments for hydrocodone addiction?
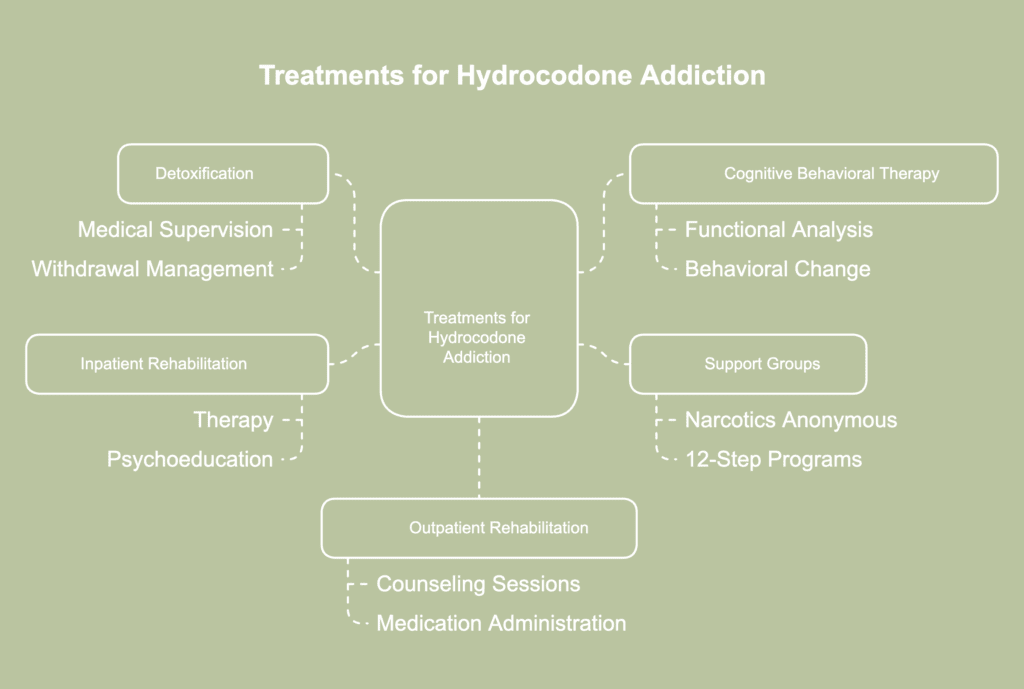
Treatments for hydrocodone addiction refer to the various approaches used to help individuals stop using the drug and recover from dependence. The treatments for hydrocodone addiction are listed below.
- Detoxification: Detoxification, or detox, is the process of allowing the body to remove hydrocodone and manage withdrawal symptoms in a safe and controlled environment. Medical personnel usually oversee the process and offer medicine and support to alleviate the psychological and physical symptoms of withdrawal. Detox—an initial step in addiction treatment—stabilizes patients and helps with the transition to sobriety.
- Cognitive behavioral therapy (CBT): The shift in thinking encouraged by CBT helps reduce the urge to rely on hydrocodone as a coping mechanism. According to a 2023 paper by Durpoix et al., titled “Psychotherapies in opioid use disorder: toward a step-care model,” CBT addresses vicious cycles of dysfunctional behaviors and is beneficial for both OUD and co-occurring mental disorders (such as anxiety and depression). Targeting emotions, beliefs, and actions, the method uses functional analysis to assist patients in recognizing and changing faulty conditioning.
- Support groups and 12-step programs: Support groups, such as Narcotics Anonymous (NA), provide a community of individuals in recovery, offering mutual support and accountability. Recognizing powerlessness over addiction, offering amends, and assisting others in recovery form several core principles of 12-step programs designed to promote and maintain sobriety. Support group participation creates a feeling of community and offers continuous social and emotional support.
- Inpatient rehabilitation: Inpatient rehab requires residing at a treatment center for a designated time, offering access to intensive therapy and medical supervision. The regulated surroundings free one from daily stresses and usual triggers, allowing complete focus on recovery. Inpatient programs often include a combination of therapy, psychoeducation, counseling, and holistic treatments.
- Outpatient rehabilitation: Outpatient rehab allows individuals to receive treatment while continuing to live at home and attend to daily responsibilities. Regular trips to a clinic or treatment facility for counseling sessions, medication administration, and support groups are all part of treatment. Outpatient rehab offers flexibility and is a good option for people with milder addictions or as a step-down program after inpatient treatment.
When is hydrocodone addiction counseling necessary?
Hydrocodone addiction counseling is necessary when an individual shows signs of dependency or addiction to the drug, such as compulsive use, inability to stop despite negative consequences, and experiencing withdrawal symptoms.
When addiction begins to harm relationships, employment, and physical well-being, seeking counseling becomes essential. Professional help holds even greater importance after failed attempts to quit independently or when underlying mental health conditions fuel the addiction.
Is hydrocodone addiction treated in rehab?
Yes, hydrocodone addiction is treated in rehab. Treatment centers offer structured programs aimed at assisting people in quitting drugs and reestablishing good habits. Medical detox is often the first step, allowing withdrawal symptoms to be managed under supervision.
Patients attend therapy sessions to treat the psychological components of addiction following detoxification. Behavioral therapies like cognitive behavioral therapy assist people in improving coping skills and altering negative thought patterns.
Rehab programs additionally include group therapy, relapse prevention planning, and educational workshops. Both inpatient and outpatient options are available, depending on the severity of the addiction.
Can you overcome hydrocodone addiction on your own?
No, you cannot overcome hydrocodone addiction on your own. The physical dependence, intense cravings, and emotional challenges involved often make self-recovery extremely difficult. Without medical supervision, withdrawal symptoms become overwhelming and potentially dangerous.
Trying to quit without assistance often leads to relapse due to the absence of a structured support system. Formal treatment provides medical supervision, therapeutic guidance, and behavioral tools to address the physical and emotional components of addiction.
Support from trained professionals and peers strengthens motivation and accountability. Recovery outcomes are significantly better when guided by a comprehensive treatment plan rather than through self-reliance alone.
Is Suboxone an effective treatment for hydrocodone addiction?
Yes, Suboxone is an effective treatment for hydrocodone addiction. For the relief of cravings and withdrawal symptoms, Suboxone combines buprenorphine with naloxone. Individuals addicted to opiates benefit from Suboxone as a safer option, as it stabilizes brain chemistry without causing a strong high.
People are able to work toward long-term healing while regaining control over everyday affairs thanks to the medication. Treatment gains considerably greater efficacy when paired with behavioral therapy and counseling.
However, misuse of Suboxone leads to Suboxone addiction if not taken under medical supervision. Proper medical oversight ensures the medicine is used safely and effectively as part of a comprehensive addiction treatment program.
Why is using hydrocodone addictive?
Hydrocodone is addictive due to its strong action on the brain’s reward centers. Pleasure and pain relief are brought about by the drug’s effect on dopamine levels. Once the brain begins associating hydrocodone with comfort and satisfaction, the rewarding sensation promotes repeated use.
A 2021 article by Meier et al., titled “The Role of Mu-Opioids for Reward and Threat Processing in Humans: Bridging the Gap from Preclinical to Clinical Opioid Drug Studies” explained mu-opioid receptors (MORs) serve as the main binding sites for opioids and appear in large concentrations throughout the human brain.
MORs influence multiple mental and emotional functions, including reward responses, mood control, and choices in behavior. Prolonged exposure to opioids interferes with mu-opioid system performance, altering how the brain handles pleasure and stress.
Such interference results in problems with emotional stability and learning—both factors intensify the addictive nature of opioid drugs. A stronger desire for and greater enjoyment of rewarding experiences directly connects to the elevated risk of addiction.
Mu-opioid activity amplifies pleasure during rewarding events and boosts motivation during the anticipation or pursuit of a reward.
Can you overdose on hydrocodone?
Yes, you can overdose on hydrocodone. Taking high doses of hydrocodone opioid slows down central nervous system functions, including breathing and heart rate. Respiratory depression poses the greatest danger, as breathing becomes dangerously shallow or stops altogether.
In severe cases, coma or death potentially results without immediate medical attention. Mixing hydrocodone with alcohol or benzodiazepines significantly increases overdose risk. Prompt treatment with naloxone and emergency care reverses life-threatening effects when administered in time.
According to a publication by Cofano et al., last updated in February 2024 titled “Hydrocodone,” to avoid an overdose caused by an uncontrolled and fast medicine distribution, hydrocodone pills and capsules must not be chewed, crushed, or dissolved.
What are the signs of hydrocodone overdose?
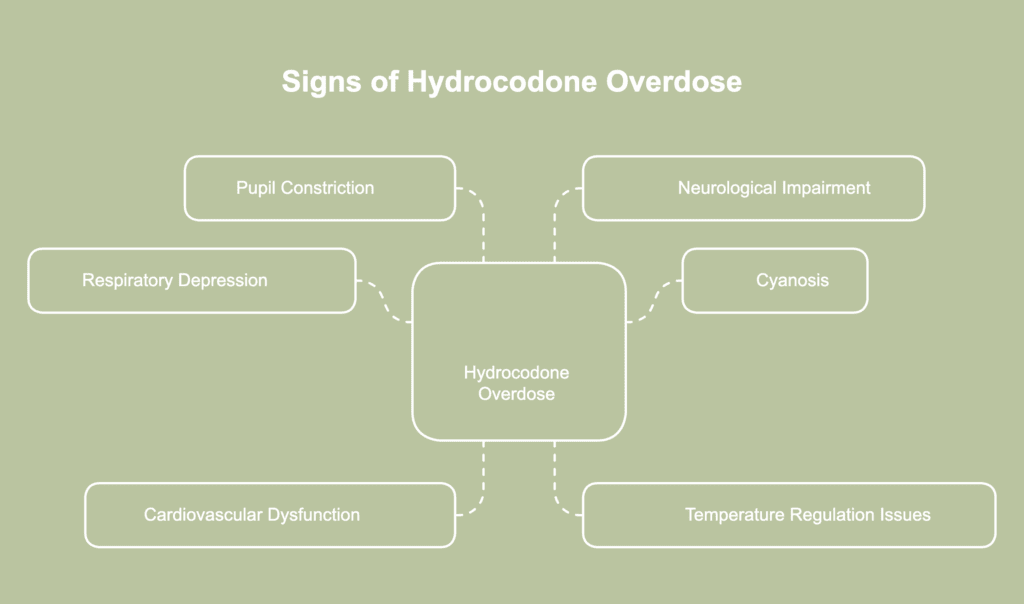
Signs of hydrocodone overdose refer to the symptoms indicating an individual has consumed a dangerously high amount of hydrocodone. The signs of hydrocodone overdose are listed below.
- Slow or shallow breathing: One of the most dangerous signs of hydrocodone overdose is slow or shallow breathing, otherwise known as respiratory depression. The drug significantly reduces the respiratory rate, leading to insufficient oxygen intake. The primary cause of death for individuals abusing or overdosing on opioids is opioid-induced respiratory depression, according to a 2020 article titled “The Physiology and Maintenance of Respiration: A Narrative Review” by Lynn R. Webster and Suzanne Karan.
- Bluish discoloration of lips or fingernails: Bluish discoloration of the lips or fingernails, known as cyanosis, occurs due to a lack of oxygen in the blood, a serious consequence of respiratory depression caused by overdose. Cyanosis signals inadequate oxygen delivery to vital organs and tissues.
- Slow or irregular heartbeat: Hydrocodone overdose slows central nervous system activity, interfering with signals responsible for controlling cardiovascular function. Slowed respiration reduces oxygen levels in the blood, placing strain on the heart. Oxygen deprivation and altered brain activity interfere with normal heart rhythms, potentially triggering arrhythmias. Severe overdoses lead to dangerously slow, erratic, or uneven heartbeats requiring emergency intervention.
- Cold or clammy skin: The skin feels cold and clammy to the touch during an opiate overdose, indicating poor circulation and reduced body temperature. The symptom results from the body’s compromised ability to regulate temperature and blood flow due to the depressant effects of hydrocodone.
- Pinpoint pupils: Pinpoint pupils, or unusually small pupils, are a classic sign of opioid overdose, including hydrocodone. Opioids constrict the muscles of the iris, leading to reduced pupil size. Pinpoint pupils often appear early during an overdose and tend to occur alongside symptoms such as drowsiness and slowed breathing.
- Confusion: Excessive intake of hydrocodone hampers neurological activity, leading to slowed mental responses. Decreased oxygen delivery to the brain affects cognitive function, resulting in confusion and difficulty focusing. Drug accumulation in the body changes the balance of neurotransmitters, affecting memory and judgment. Mental clarity declines as toxicity increases, resulting in noticeable confusion.
- Decreased level of consciousness: A decreased level of consciousness serves as a critical warning sign of an overdose, with the affected person appearing heavily sedated, sluggish, or unresponsive. The condition results from hydrocodone’s ability to suppress central nervous system activity, disrupting normal brain operations. The person struggles to stay awake, has difficulty responding to questions or stimuli, and in severe cases, falls into a coma.
How addictive is hydrocodone compared to oxycodone?
Hydrocodone and oxycodone are both highly addictive opioids, but oxycodone is generally considered to have a slightly higher potential for addiction. The stronger euphoric effects linked to oxycodone frequently lead to misuse at an earlier stage. Hydrocodone still produces rewarding sensations but does so less intensely, resulting in a slower progression to compulsive use.
Oxycodone’s persistently high likeability and mild side effects account for both the drug’s disproportionate contribution to opioid-related morbidity (such as emergency department (ED) visits) and preferred use among recreational users, according to a 2012 study by Wightman et al., titled “Likeability and Abuse Liability of Commonly Prescribed Opioids” published in the Journal of Medical Toxicology.
Oxycodone’s greater appeal often results from pharmacological characteristics like rapid onset, unique interaction with mu-opioid receptors, or specific metabolic processes, contributing to a greater risk of oxycodone addiction.
How long does it take to get addicted to hydrocodone?
It takes as little as a few days to several weeks to get addicted to hydrocodone, depending on dosage, frequency, and individual susceptibility. Regular use triggers the brain’s reward circuits, reinforcing the behavior through feelings of euphoria and pain relief.
Repeated exposure quickly builds tolerance, requiring higher amounts to achieve the same effect. As per a 2019 report by Klimas et al., titled “Strategies to Identify Patient Risks of Prescription Opioid Addiction When Initiating Opioids for Pain: A Systematic Review,” prescription opioid use disorder is more likely to develop in people taking opioids for 30 days or longer (3.5–4.9 times) or in high doses (>120 morphine milligram equivalents (MME)/day, 3.2–3.4 times).
What are the causes of hydrocodone addiction?
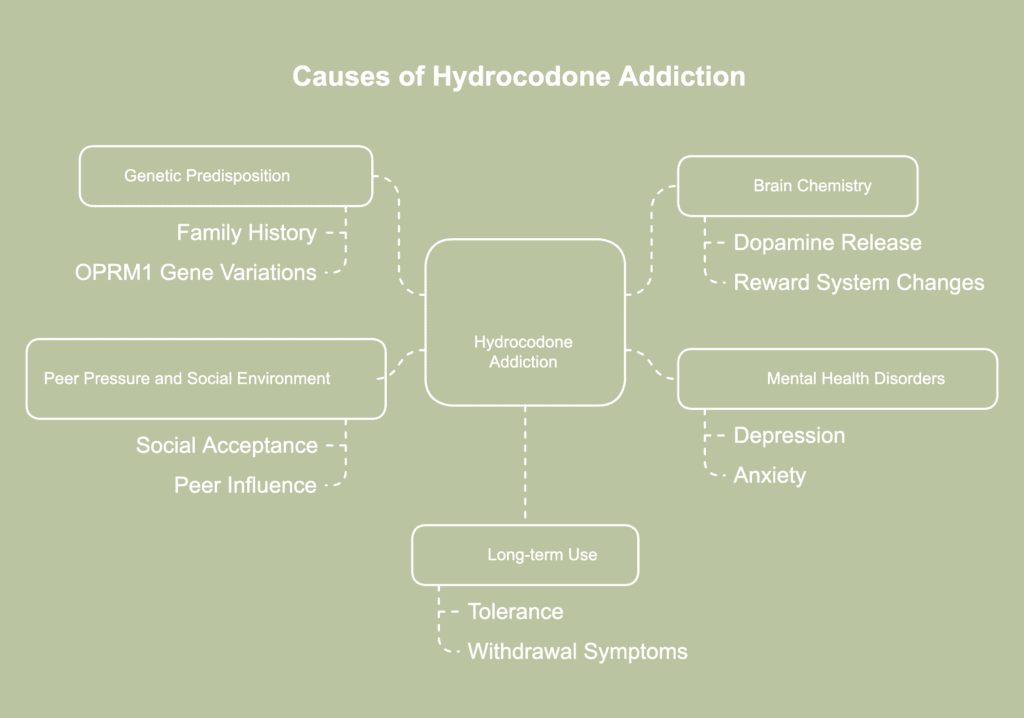
Causes of hydrocodone addiction refer to the various factors contributing to the development of dependency on hydrocodone. The causes of hydrocodone addiction are listed below.
- Genetic predisposition: Genetic predisposition plays a significant role in the development of hydrocodone addiction. Individuals with a family history of addiction inherit certain genetic traits, making dependence more likely. According to an article titled, “Opioid addiction” last updated in November 2017 by MedlinePlus, most opioid medications mainly attach to the mu (μ) opioid receptor, a product of the OPRM1 gene. Common variations in the OPRM1 gene appear to influence how the body reacts to opioids, including the dosage needed for effective pain relief. Genetic diversity in the OPRM1 gene shows a connection, particularly in certain populations, to a heightened risk of developing opiate addiction.
- Brain chemistry: The dopamine released when hydrocodone interacts with opioid receptors in the brain generates intense feelings of pleasure and reinforces drug-taking behavior. Repeated exposure changes the brain’s reward system, causing increased dependence on the substance to experience pleasure. Natural production of dopamine becomes disrupted, reducing the ability to enjoy everyday activities. Brain circuits adjust to ongoing stimulation, often leading to uncontrollable urges to seek the drug.
- Mental health disorders: The pain caused by mental health conditions often lead people to self-medicate, seeking temporary comfort through opioids. According to a 2020 publication titled “Common Comorbidities with Substance Use Disorders Research Report” from the National Institute on Drug Abuse, research indicates 43% of patients receiving treatment for substance use disorder (SUD) related to non-medical prescription painkiller use have a diagnosis or symptoms of a mental health condition, especially depression and anxiety.
- Peer pressure and social environment: Peer pressure and the social environment play a crucial role in the initiation and continuation of hydrocodone use. Being in a social circle where drug use is prevalent increases the likelihood of experimenting with hydrocodone. Continued use in such settings leads to addiction as individuals seek acceptance or are influenced by others’ behaviors.
- Long-term use: Long-term use of hydrocodone significantly increases the risk of addiction due to the development of tolerance and physical dependence. Over time, individuals require higher doses to achieve the same pain-relieving or euphoric effects, leading to a cycle of escalating use. When the body adjusts to regular hydrocodone exposure, reducing or stopping use triggers withdrawal, encouraging further consumption.
What are the side effects of hydrocodone?

Side effects of hydrocodone refer to the unintended and often adverse reactions occurring when taking hydrocodone. The side effects of hydrocodone are listed below.
- Drowsiness: Drowsiness or sedation significantly affects hydrocodone users due to the drug’s depressant impact on the central nervous system, impairing cognitive and motor functions and posing dangers for driving or operating heavy machinery. While a certain degree of drowsiness diminishes over time as the body adjusts to the medication, persistent sedation interferes with daily activities.
- Dizziness: Dizziness frequently occurs with hydrocodone use, often resulting from the drug’s ability to lower blood pressure and disrupt balance. Hydrocodone causes lightheadedness or vertigo by upsetting the brain’s capacity to integrate sensory data including spatial orientation and balance. In certain users, the medicine reduces blood pressure, lowering cerebral blood flow causing dizziness.
- Constipation: Hydrocodone slows down the digestive system by binding to opioid receptors in the gut. Reduced intestinal movement follows, leading to slower processing of food and waste. Individuals then experience difficulty passing stool and prolonged constipation. The longer hydrocodone is used, the more pronounced the side effect becomes.
- Dry mouth: Hydrocodone influences the autonomic nervous system, affecting saliva production. Reduced saliva leads to a dry, sticky feeling often linked to discomfort. Persistent dry mouth increases the risk of tooth decay and gum issues over time.
- Agitation: Hydrocodone affects neurotransmitters responsible for mood regulation. Disruption in brain chemical balance often triggers restlessness or heightened emotional sensitivity. Irritability and discomfort tend to emerge during the comedown or withdrawal period. Such emotional disturbances reflect the brain’s struggle to stabilize without the drug’s influence.
- Difficulty urinating: Difficulty urinating, or urinary retention, is a possible side effect of hydrocodone due to its effects on the muscles controlling the bladder. Individuals experience a decreased urge to urinate, a weak urine stream, or a feeling of incomplete bladder emptying. A 2008 review article by Verhamme et al., titled “Drug-Induced Urinary Retention: Incidence, Management and Prevention” explained how opioids lower the urge to urinate by interfering with nerve signals responsible for bladder function. Increased muscle tension around the urinary sphincter occurs due to overstimulation of the sympathetic nervous system, making urination more difficult.
- Unusual tiredness: Unusual tiredness or fatigue results from hydrocodone use, stemming from the drug’s sedative properties and overall depressant effects on the central nervous system. Excessive tiredness affects daily functioning, productivity, and overall quality of life.
What are the risk factors for hydrocodone addiction?

Risk factors for hydrocodone addiction are any number of factors making someone more likely to become dependent on the drug. The risk factors for hydrocodone addiction are listed below.
- Stress: Chronic stress is a common contributor to hydrocodone addiction, as individuals use the drug to cope with stressors. Hydrocodone’s relaxing and euphoric effects offer a momentary reprieve from uncomfortable circumstances or emotions. However, relying on the medication to relieve stress eventually results in compulsive use and addiction.
- High dose of opioid: Taking high doses of hydrocodone significantly increases the risk of addiction due to the intensified effects on the brain’s reward system. An article titled “Risk Factors for Opioid Misuse, Addiction, and Overdose” from the United States Department of Labor asserted the risk of misuse and fatal overdoses increases as the opioid dose increases. Higher doses, defined by amounts exceeding 100 morphine milligram equivalents (MME), are associated with a risk more than twice as high as smaller concentrations. Even modest doses (e.g., 20-50 MME) carry a risk.
- Accessibility and availability: Easy access to hydrocodone, whether through legitimate prescriptions or illicit sources, heightens the risk of addiction. Over-prescription and the widespread availability of hydrocodone lead to misuse and dependency. Easy access to the medication raises the chances of misuse and heightens the risk of developing a substance dependency.
- Previous substance abuse: People with a history of substance abuse often experience changes in brain function, increasing vulnerability to forming new dependencies. Patterns linked to previous addictive behaviors and unhealthy coping strategies frequently lead to hydrocodone misuse.
- Early-onset use: Taking hydrocodone for the first time at an early age disrupts brain development, particularly in regions involved in impulse control and decision-making. An increased risk of long-term dependence is associated with increased sensitivity to the drug’s effects due to early exposure. Continued use from an early stage reinforces addictive behaviors over time.