Types of phobia
A phobia is an extreme, illogical fear of a particular thing, circumstance, or action frequently resulting in avoidance behaviors. Usually surpassing reasonable prudence, the fear causes major disturbance and interference with daily living. The two types of phobias are specific phobias and complex phobias.
Specific phobias, formerly called simple phobias, are intense, irrational fears focused on particular objects, situations, or activities, such as heights, animals, or confined spaces. Strong anxiety brought on by specific phobias frequently causes people to avoid the feared triggers, upsetting regular activities and routines.
Complex phobias are motivated by continuous, anxiety-inducing worries like agoraphobia or social anxiety, often connected to social rejection or embarrassing events. Severe impairment in daily functioning and long-term avoidance of social situations are common outcomes of such phobias.
The 10 most common phobias include arachnophobia (fear of spiders), acrophobia (fear of heights), ophidiophobia (fear of snakes), cynophobia (fear of dogs), aerophobia (fear of flying), astraphobia (fear of thunder and lightning), social phobia (social anxiety disorder), agoraphobia (fear of open or crowded spaces), trypanophobia (fear of injections), and claustrophobia (fear of confined spaces).
Specific phobias
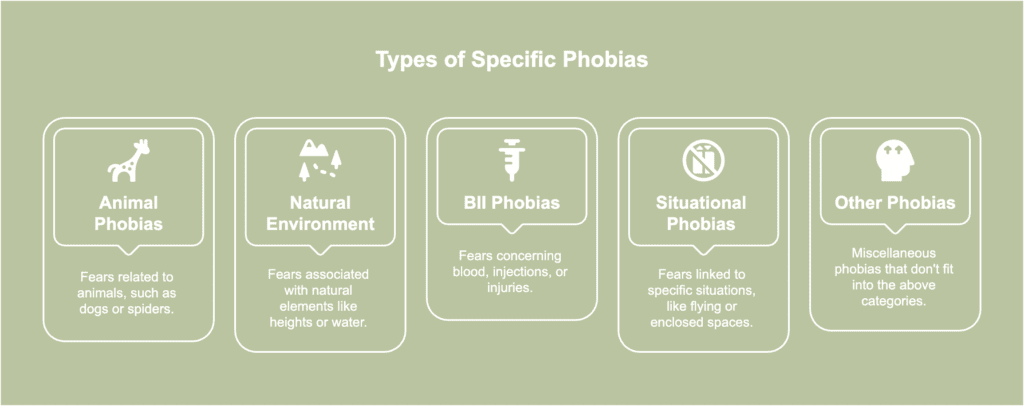
Specific phobias refer to extreme, unwarranted fears directed at certain things or situations. The different types of specific phobias are listed below.
- Animal phobias
- Natural environment phobias
- Blood-injection-injury (BII) phobias
- Situational phobias
- Other specific phobias
Animal phobias
Animal phobias are defined as a chronic, strong fear of particular animals frequently resulting in avoidance behaviors and extreme suffering when the feared animal is present. Otherwise known as zoophobia, such phobias tend to disrupt daily activities, as the fear response activates even at the thought or image of the animal.
Causes typically stem from past traumatic experiences with animals, observational learning (witnessing others show fear toward an animal), or genetic predispositions increasing vulnerability to anxiety disorder.
Symptoms of animal phobias include sweating, rapid heartbeat, shaking, shortness of breath, nausea, lightheadedness, and a strong urge to flee upon seeing or imagining the animal.
Diagnosis involves a psychological assessment, where mental health professionals evaluate the individual’s fear intensity, avoidance behaviors, and the phobia’s impact on daily life. Diagnosing animal phobias usually follows criteria from the DSM-5 (Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition), requiring the fear be excessive, persistent (lasting six months or more), and disruptive to normal functioning.
Treatment options generally include cognitive-behavioral therapy (CBT), particularly exposure therapy, a method gradually desensitizing individuals to the feared animal by repeated, controlled exposure, as well as medications. Medications, such as anti-anxiety drugs or beta-blockers, offer temporary relief from symptoms but are typically combined with therapy for long-term results.
Common examples of animal phobias include fear of spiders (arachnophobia), snakes (ophidiophobia), bats (chiroptophobia), dogs (cynophobia), and insects (entomophobia), each causing unique reactions based on personal or cultural associations with the animal.
Natural environment phobias
Natural environment phobias are intense, irrational fears frequently met with avoidance behaviors and distress when confronted with natural elements such as water, heights, darkness, or storms.
Causes include past traumatic events, such as near-drowning or experiencing a severe storm, as well as genetic factors or cultural influences increasing anxiety around certain natural phenomena.
Symptoms of natural environment phobias include intense anxiety or panic when encountering feared elements, triggering a “fight-or-flight” response, sweating, increased heart rate, trembling as the body responds to perceived danger, an overwhelming urge to escape, extreme worry about future encounters with the feared environment, and irrational thoughts about harm.
Natural environment phobias are diagnosed through a psychological evaluation where medical professionals analyze the degree, duration, and influence of the fear on day-to-day functioning. According to the DSM-5 criteria, diagnosis usually requires the fear to be severe, unreasonable, ongoing, and interfering with day-to-day functioning for a minimum of six months.
Treatment options include cognitive-behavioral therapy (CBT) to challenge negative thought patterns, exposure therapy for gradual desensitization, and, in certain cases, medication to manage symptoms during treatment.
More recent research has looked into novel treatments for specific phobias. For instance, in virtual reality exposure therapy (VRET), an individual with a phobia encounters the feared circumstance within a completely artificial environment recreated by a computer program via a headset.
A 2020 review by Thng et al., titled “Recent developments in the intervention of specific phobia among adults: a rapid review” mentioned VRET has proven effective in addressing multiple phobias, including fear of storms.
Additionally, VRET exhibited substantial decreases in distress, anxiety, and avoidance scores, with results comparable to conventional exposure therapy in numerous instances.
Common natural environment phobias include acrophobia (fear of heights), aquaphobia (fear of water), astraphobia (fear of thunderstorms), and nyctophobia (fear of darkness), each associated with a particular natural element triggering the phobic response.
Blood-injection-injury (BII) phobias
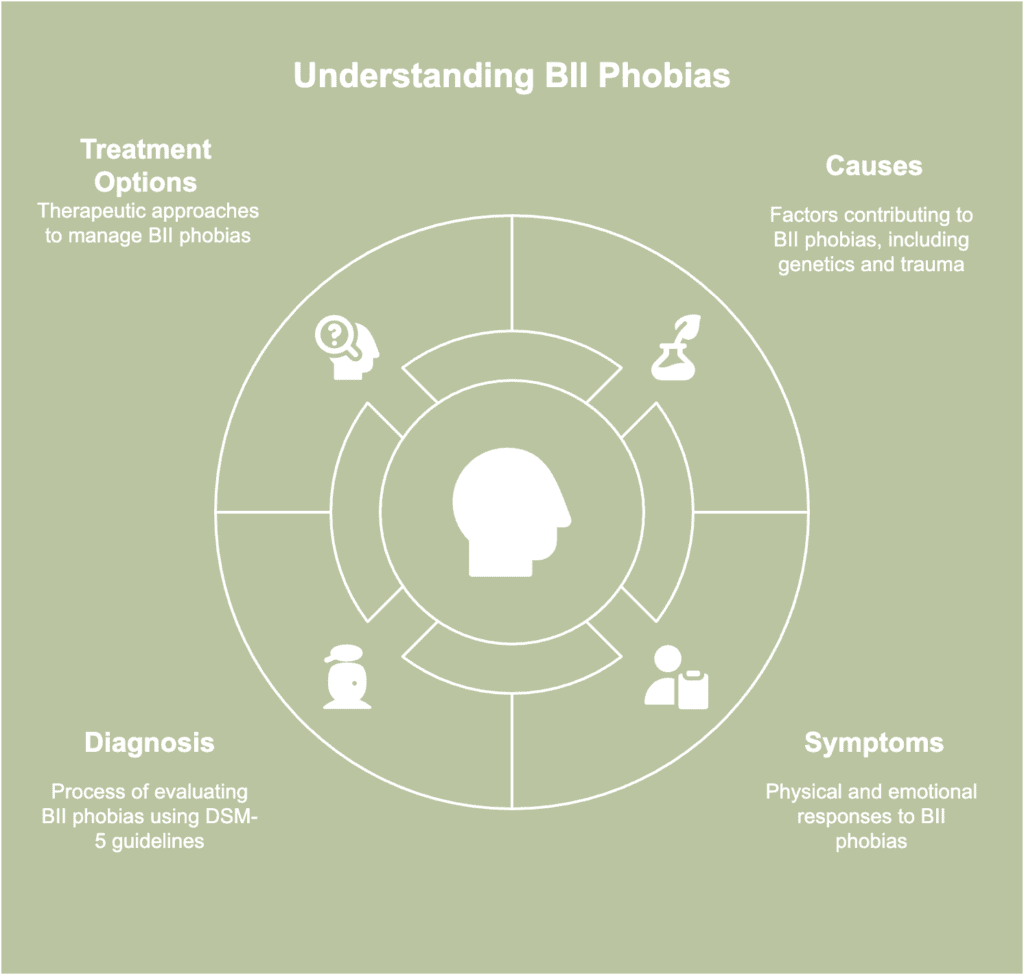
Blood-injection-injury (BII) phobias are a type of specific phobia involving an intense, irrational fear of blood, injections, injuries, or medical procedures often leading to physical and emotional distress.
Causes include genetic predisposition, past traumatic experiences with medical procedures, or learned fear from family or media exposure.
Symptoms differ from other phobias, as BII phobias frequently involve a fainting response or a sudden drop in blood pressure, alongside anxiety, nausea, and avoidance of medical situations. Fainting is a prevalent symptom of BII phobia, with 55.77% of individuals experiencing fainting episodes, according to a 2014 research article by Wani et al., titled “Blood Injury and Injection Phobia: The Neglected One.”
The typical physiological response is characterized by a diphasic cardiovascular pattern involving an initial rapid heartbeat, a subsequent decrease in heart rate, a decrease in blood pressure, and occasional fainting.
Diagnosis typically includes a mental health evaluation, where professionals assess the severity and impact of the phobia according to DSM-5 guidelines, confirming symptoms persist for at least six months and interfere with daily life.
Treatment options for BII phobias often include CBT to reshape negative thoughts, exposure therapy to eventually face feared stimuli, and applied tension techniques to prevent fainting by increasing blood pressure.
Common BII phobias encompass hemophobia (fear of blood), trypanophobia (fear of injections), and traumatophobia (fear of injuries), all eliciting comparable responses linked to medical or bodily harm.
Situational phobias
Situational phobias are marked by an overwhelming fear of particular scenarios, such as traveling by plane or being in small, confined areas. People with situational phobias often take extreme measures to avoid such circumstances, as the anticipation or experience of the triggering circumstances brings on intense feelings of panic and helplessness.
Causes of situational phobias include previous traumatic incidents, like being trapped in an elevator or enduring a turbulent flight, leaving lasting associations of fear. Family history plays a role as well, as genetic predispositions or observing a parent’s or loved one’s fear response increases susceptibility to developing similar phobias.
Symptoms typically include rapid heartbeat, sweating, nausea, dizziness, and an overwhelming urge to escape, with even the thought of exposure often triggering anxiety.
Diagnosing situational phobias involves observing how the person reacts and making notes about whether the fear is excessive and gets in the way of daily life. Clinicians look for patterns of avoidance and emotional distress when facing or thinking about the feared situation, using specific diagnostic criteria to confirm the phobia.
Treatment frequently consists of cognitive behavioral therapy (CBT) to assist in the management of anxious thoughts, exposure therapy to eventually confront feared situations, and relaxation techniques to alleviate physical symptoms of anxiety.
Common situational phobias include aviophobia (fear of flying), claustrophobia (fear of enclosed spaces), acrophobia (fear of heights), vehophobia (fear of driving), and tunnel phobia (fear of tunnels).
Other specific phobias
Other specific phobias involve intense and irrational fears of certain objects, situations, or activities outside the more common categories of animal phobias, natural environment phobias, situational phobias, or blood-injection-injury phobias.
Causes of other specific phobias include traumatic experiences, genetic predisposition, learned behaviors, or cultural influences instilling an exaggerated sense of danger. Childhood conditioning or observing fearful reactions in others contribute to the development of such phobias as well.
Symptoms include physical reactions like sweating, shaking, or a fast heartbeat, avoidance behavior impeding day-to-day functioning, and extreme fear or anxiety when exposed to the phobic stimulus. Even when thinking about the phobic stimulus, such reactions take place, resulting in anticipatory anxiety interfering with everyday interactions and relationships.
Diagnosis of other specific phobias involves a clinical evaluation based on DSM-5 criteria, including persistent, excessive fear disproportionate to the actual threat. Clinicians are additionally likely to use structured interviews or questionnaires to assess the severity and impact of the phobia on the individual’s daily life and functioning.
Treatment options include CBT with exposure therapy, relaxation techniques, and, in certain cases, medication like anti-anxiety drugs to manage severe symptoms. Treatment approaches for the condition teach coping strategies to control anxiety, progressively lower fear reactions, and target the underlying thought patterns causing the phobia.
Examples include fear of clowns (coulrophobia), fear of choking (pseudodysphagia), fear of vomiting (emetophobia), fear of holes (trypophobia), and nomophobia, short for “no-mobile-phone phobia” (fear of being without a mobile phone).
Complex phobias

Complex phobias are intense, persistent fears often associated with specific situations or social interactions and typically involve deeper emotional or psychological triggers compared to specific phobias. Common examples of complex phobias are listed below.
- Social phobia
- Agoraphobia
Social phobia
Social phobia, or social anxiety disorder, is an overwhelming fear of being evaluated or observed in social or performance contexts, resulting in considerable distress and the evasion of social engagements.
Individuals with the condition often experience overwhelming worry about embarrassing themselves or being negatively evaluated by others, even in routine or low-pressure environments.
The causes of social phobia are a combination of genetic factors, negative childhood experiences, and learned behavior resulting from the observation of others’ social discomfort. Social anxiety disorder additionally occurs as a result of a history of bullying, overprotective parenting, or a lack of social support during early life.
Symptoms often include blushing, trembling, excessive sweating, and a strong desire to flee from social settings due to fear of embarrassment or humiliation. During more severe cases, individuals struggle with a racing heart, difficulty speaking, nausea, or a sense of disconnection from reality in social interactions.
Diagnosis of social anxiety disorder is based on a clinical evaluation using DSM-5 criteria, with a focus on excessive and ongoing fear of social situations getting in the way of daily life. Clinicians additionally look at how long symptoms have been present, usually six months or longer, and rule out other conditions possibly causing the anxiety, like substance abuse or medical disorders.
A 2022 study by Alomari et al., titled “Social Anxiety Disorder: Associated Conditions and Therapeutic Approaches” highlighted medication and cognitive behavioral therapy (CBT) as the two primary treatment options for social anxiety disorder (SAD).
CBT is regarded as the gold standard, and other models—such as exposure techniques and cognitive restructuring—have shown promise in treating SAD. While medications, especially SSRIs (selective serotonin reuptake inhibitors), are widely used, side effects such as changes in weight and sexual dysfunction were observed. Using CBT in conjunction with medication produces superior outcomes.
Agoraphobia
Agoraphobia is an anxiety disorder marked by a severe fear of being in circumstances where one cannot escape or in which assistance is not available. People usually avoid crowds, open spaces, and unfamiliar surroundings due to such fear.
A continuing education activity, titled “Agoraphobia” by Kripa Balaram and Raman Marwaha last updated in November 2024 revealed the causes of agoraphobia, including parental overprotectiveness, childhood anxieties or night terrors, early experiences of grief or bereavement, traumatic or unpleasant childhoods, and genetic predisposition. Comorbid personality types encompass dependent, obsessive-compulsive, or otherwise “highly neurotic” traits.
Symptoms range from bodily symptoms such as nausea, dizziness, tightness in the chest, choking sensations, and a fast heartbeat accompanied by avoidance behavior, to dread and panic attacks in triggering situations.
Agoraphobia is diagnosed through a clinical evaluation based on the DSM-5 criteria, requiring persistent fear or anxiety about at least two situations, including public transportation, open or enclosed spaces, crowds, or being alone outside the home. The fear must be disproportionate to the actual danger and persist for six months or longer.
Treatment options for agoraphobia include CBT to challenge and change fear-based thoughts and medications like selective serotonin reuptake inhibitors (SSRIs) to manage severe anxiety. A healthy diet, regular exercise, and the use of relaxation techniques like deep breathing or meditation are examples of lifestyle modifications known to lower anxiety levels and enhance coping strategies.
What is a phobia?
A phobia is an intense, irrational fear of a specific object, situation, or activity resulting in avoidance and significant distress when faced with the feared trigger. Unlike general fear, a temporary and proportionate response to a threat, a phobia persists over time and often disrupts daily life, as individuals take extreme measures to avoid the object or source of fear.
According to a 2018 paper by Eaton et al., titled, “Specific phobias,” research shows the lifetime incidence of specific phobias globally varies between 3% and 15%, with fears related to heights and animals being the most prevalent.
Phobias endure for several years or even decades in 10–30% of instances and are highly indicative of the emergence of other anxiety, mood, and substance-use disorders.
Phobias generally arise from an interplay of factors, including genetic predisposition, traumatic experiences, or acquired behavior, and tend to present with both physiological and psychological symptoms.
Physical responses to phobia include sweating, rapid heartbeat, dizziness, or shortness of breath, while psychological symptoms often involve overwhelming anxiety, panic, or a strong desire to escape.
What are the 10 most common phobias?

The 10 most common phobias are the most prevalent fears affecting a wide range of individuals from different backgrounds. The 10 most common phobias are listed below.
- Arachnophobia: Arachnophobia, the fear of spiders, provokes extreme distress upon seeing a spider or even thinking about one. People with arachnophobia frequently steer clear of areas where spiders are likely to be found, largely interfering with day-to-day activities.
- Acrophobia: Acrophobia, the fear of heights, causes feelings of dizziness, vertigo, or panic when in high places. Often, acrophobia causes people to avoid heights—for instance, scenarios involving stairs, visiting towering buildings, or crossing bridges.
- Ophidiophobia: Ophidiophobia is an intense fear of snakes causing severe anxiety, even when viewing photos or videos of them. Individuals suffering from ophidiophobia often steer clear of environments likely to contain snakes to avoid triggering reactions like heightened anxiety or distress.
- Cynophobia: Cynophobia, the fear of dogs, stems from a past traumatic experience, such as being bitten or chased. The condition frequently induces panic attacks upon seeing a dog, causing persons to evade parks or locations where dogs are possibly present.
- Aerophobia: Aerophobia, the fear of flying, creates intense pre-flight anxiety or panic during air travel. Affected individuals experience travel disruptions in personal and professional plans due to a fear of flying.
- Astraphobia: Astraphobia, the fear of thunder and lightning, brings about extreme distress during storms, leading affected individuals to seek shelter or safety. Constant worry about upcoming storms affects daily plans and even results in checking weather forecasts obsessively.
- Social phobia (social anxiety disorder): Social phobia involves a fear of being scrutinized or judged by others in social or performance settings. Numerous individuals with social anxiety disorder avoid social situations to prevent possible embarrassment, negatively affecting friendships, professional growth, and general quality of life.
- Agoraphobia: Agoraphobia, a fear of open or crowded spaces, creates a sense of entrapment when escape appears difficult. Severe cases lead to isolation at home and often cause avoidance of public venues such as malls or public transit.
- Trypanophobia: Trypanophobia, the fear of injections, triggers severe discomfort and anxiety at the thought or sight of needles. Such an intense reaction complicates access to essential medical care, including vaccinations or blood tests.
- Claustrophobia: Claustrophobia, the fear of confined spaces, causes intense fear and even panic in small or enclosed areas, like elevators or packed rooms. Claustrophobic persons take precautions to stay out of confined areas, limiting their capacity to fully engage in everyday activities.
What are the worst phobias to live with?
The worst phobias to live with refer to particularly intense and debilitating fears significantly interfering with a person’s daily life, well-being, and functionality. The worst phobias to live with are listed below.
- Agoraphobia: The fear of open or crowded spaces tends to be severely limiting, often preventing individuals from leaving home or participating in daily activities, leading to extreme isolation and reliance on others.
- Social phobia: Anxieties over being embarrassed or judged lead to difficulties in engaging with people, negatively affecting personal relationships, professional performance, and even running errands in public.
- Claustrophobia: Fear of enclosed spaces disrupts both personal and professional life by causing difficulty in using elevators, public transportation, or undertaking necessary medical scans.
- Thanatophobia: The excessive fear of dying or losing a loved one, known as thanatophobia, interferes with everyday enjoyment and mental health and causes chronic anxiety.
- Emetophobia: The intense fear of vomiting, often in public, disrupts eating habits, causes social isolation, and results in avoidance of public places or medical care, significantly affecting mental and physical health.
- Nyctophobia: Often associated with sleep disturbances, nyctophobia, or the fear of darkness, disrupts nightly routines, leads to insomnia, and exacerbates overall anxiety levels.
- Glossophobia: Common in professional and social settings, a fear of public speaking hinders career growth, education, and the ability to connect with others.
- Atychiphobia: Extreme fear of failure causes people to forgo social, occupational, or educational activities, therefore impeding personal development and fulfillment by discouraging any apparent risk.
- Somniphobia: The fear of sleep or sleep-related issues often leaves individuals struggling with insomnia, chronic anxiety, and sleep deprivation, impacting overall health and cognitive abilities.

